Orthopaedic Research and Surgery
OPEN ACCESS | Volume 5 - Issue 1 - 2025
ISSN No: 2994-8738 | Journal DOI: 10.61148/2994-8738/JORS
Daniel Ribeiro Mesquita1*, Aline Hamilton Goulart2, Bruna Gizele Noronha de Medeiros3, Claudio Feitosa de Albuquerque Junior4, Danilo de Oliveira Parra5
1Major Orthopedic Surgeon and Member of the Knee Surgery Committee at the Brazilian Army Health Corps; Chief of the Division of Medicine and Orthopaedics at the Porto Velho Military Hospital, Rondonia, West Amazon; Orthopaedic Surgeon at the João Paulo II Emergency Hospital, State Health Department at Porto Velho, Rondônia; Titular Member of the Brazilian Society of Orthopedics and Traumatology; Titular Member of the Brazilian Society of Knee Surgery; Titular Member of the Latin American Society of Arthroscopy, Knee and Sports Medicine.
2Captain Vascular Surgeon of the Brazilian Army Health Corps; Member of the Brazilian Society of Angiology and Vascular Surgery, Title of Specialist in Vascular Surgery by SBACV and International Member of the Society for Vascular Surgery.
3Nurse graduated from the Federal University of Rondônia Foundation, post-graduated in Higher Education Methodology and in Nursing in Gynecology and Obstetrics. Public employee at the João Paulo II Emergency Hospital; Preceptor of the Multiprofessional Residency Program in Urgency and Emergency (Ordinance No. 1006/2019 / SESAU-ASTEC) and is the Nursing Coordinator of the Surgical Clinic (ALA III).
4Ten Cel Orthopaedic Surgeon and Member of the Hip Surgery Committee at the Brazilian Army Health Corps; Chief of the Orthopaedic Surgical Center at the Army Central Hospital, Rio de Janeiro, RJ; Member of the Hip Surgery Group at the Orthopaedics and Traumatology National Institute (INTO), Rio de Janeiro; Titular Member of the Brazilian Society of Orthopedics and Traumatology; Titular Member of the Brazilian Society of Hip Surgery.
5Lieutenant Plastic Surgeon at the Brazilian Army Health Corps; Plastic Surgeon at the Porto Velho Military Hospital, Rondonia, West Amazon.
*Corresponding Author: Daniel Ribeiro Mesquita, Major Orthopedic Surgeon and Member of the Knee Surgery Committee at the Brazilian Army Health Corps; Chief of the Division of Medicine and Orthopaedics at the Porto Velho Military Hospital, Rondonia, West Amazon; Orthopaedic Surgeon at the João Paulo II Emergency Hospital, State Health Department at Porto Velho, Rondônia; Titular Member of the Brazilian Society of Orthopedics and Traumatology; Titular Member of the Brazilian Society of Knee Surgery; Titular Member of the Latin American Society of Arthroscopy, Knee and Sports Medicine.
Received date: April 13, 2021
Accepted date: April 23, 2021
Published date: April 26, 2021
Citation: Daniel Ribeiro Mesquita, Aline Hamilton Goulart, Bruna Gizele Noronha de Medeiros, Claudio Feitosa de Albuquerque Junior, Danielo de Oliveira Parra. “Multidiscipilnary Approach to Firearm Injuries of The Extremities in Emergency Trauma’’. J Orthopaedic Research and Surgery, 2(2); DOI: http;//doi.org/03.2021/1.1012.
Copyright: © 2021 Daniel Ribeiro Mesquita. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Firearm injuries of the extremities are common in military and civilian settings. Usually associated with open fractures, soft tissue damage and vascular injury, such lesions can be life threathening and/or cause limb loss and severe impairment. Our purpose is to discuss the multidisciplinary decision-making in such injuries at the arrival in the emergency department, focusing on Orthopedics and Traumatology, Vascular Surgery, Plastic Surgery and Nurse Care.

Figure 1- Gunshot fracture of the leg that needed Orthopaedic and Vascular intervention (author´s archive)
Introduction
During the 2nd World War, the development of protective equipment decreased the incidence of thoracoabdominal injuries by firearms (1). On the other hand, injuries to the extremities were in greater evidence. These injuries are characterized by high- energy and comminuted fractures, vascular damage and important soft tissue loss. More recently, in the Global War Against Terrorism, reports from the United States Navy Medical Corps revealed an incidence of 58 to 88% of firearm injuries, with 23 to 39% of fractures in more than 56,000 patients (2).
The increasing use of high-energy weapons in modern warfare is associated with severe vascular injuries. The amputation rate of American soldiers in World War II was 35.8% after repair and 49% after ligation, emphasizing the superiority of repair (3-9). In the Iraq War (at the beginning of the 21st century), the proportion of trauma victims attained 50% to 70%.(2,3)
After the Korean and Vietnam Wars, modern fixation implants and methods and vascular repair soowed better results with gunshot and blast injuries. Vascular repair replaced ligation and amputation rates fell to 13% [38]&&Limbs are preserved after limb artery injury in >95% of cases. Even popliteal artery damage, earlier often associated with amputation, is now associated with >90% limb survival. (4-8). Since the 1970s, vascular trauma surgery in civilian hospitals has improved greatly (3, 5).
In the civil environment, violence and crime have been the main causes of firearm injuries, particularly in large urban centers in developing countries. In Brazil, data show that more than 40 thousand people die each year from firearms injuries (9 -12). By affecting more frequently young and male patients, gunshot injuries have social and economical impact on the health system and population, with loss of labor capacity and productivity, raise of costs with hospitalization and psychological consequences for the patient and relatives.
Advances in the treatment of injuries by firearms of the extremities and open fractures have occurred in the last decades, with emphasis in Reconstructive Plastic Surgery and new dressing techniques in Nursing Care, improving results. Nevertheless, such lesions continue to be a great challenge for health professionals in Emergency Trauma. Therefore, complex injuries by firearms to bones, soft tissue and vessels are better managed by a multidisciplinary team. The aim of this article is to review the multidisciplinary approach of patients with firearm injuries in the extremities, with special focus on Orthopedics and Traumatology, Vascular Surgery, Plastic Surgery and Nursing Care.
Initial Evaluation (Pre-Hospital Care And Trauma Care Team)
ATLS has been used for more than four decades to approach trauma victims (13). The ABCDE protocol standardizes the sequence of priorities in the care of trauma patients. Phases A and B (Airways and Breathing) are hardly altered in patients with gunshot injuries to the extremities, unless they have projectiles elsewhere. Phase C (Circulation) is the most critical, as they may suffer bleeding from fractures and / or adjacent structures, especially in the long bones. It is important to perform calibrated venous access to the upper limbs whenever possible and occlusive and compressive dressing to contain bleeding in phase C. In phase D (Disability), firearm injuries need to be evaluated with respect to central nervous system disorders. Phase E (Exposure) is the phase of exposure and evaluation of injuries in segments and other systems. It is the moment when the characteristics of gunshot wounds of the extremities are observed.
Vascular/ Orthopaedic Evaluation And Classification Of Injury
The suspicion of vascular injury occurs easily when there is persistent bleeding in the injured area. A hematoma with increased volume, temperature decrease, pallor of the affected limb, absence of distal pulses to the injury and/or poor blood perfusion of the extremities are evidences of vascular damage.
After support and maintenance measures, the firearm victim with vascular injury must be transfered to a hospital unit where there is a vascular surgeon on duty, so that the lesion can be corrected at the appropriate time. During this transport, measures such as compression of the wound site, use of a vascular tourniquet and elevation of the injured limb can be performed.
Vascular tourniquet application has been proven to save lifes, especially in the military setting, where gunshot injuries anb blasts are more common and severe (14). In the civil environment, tourniquet is not much applied and more scientific data must be collected (14- 18) for better conclusions.
The evaluation of the limbs takes place through inspection and palpation. During inspection, attention should be paid to the appearance and characteristics of the wound and on palpation, it is necessary to evaluate the painful regions, and fractures can be detected. The Gustillo and Anderson Classification has been used to define the treatment and prognosis of exposed fractures (Chart 1) (19). In firearm fractures, it is often difficult to define the path and energy of the projectile. Therefore, detailed evaluation and meticulous description of the lesion is extremely important to determine the severity of the lesion (19, 20). At the time of the evaluation, it is important to perform a local cleaning with saline to better assess the characteristics of the wound.
Table 1. Open fractures-gustilo classification* (19)
Type I- Open fracture with a skin wound < 1 cm in lenght and clean.
Type II- Open fracture with a laceration > 1 cm in length without extensive soft tissue damage, flaps, or avulsions.
Type III- Open segmental fracture with > 10 cm wound with extensive soft tissue injury or traumatic amputation (special categories in Type III include gunshot fractures and open fractures caused by farm injuries).
IIIa- Adequate soft tissue coverage.
IIIb- Significant soft tisuue loss with exposed bone that requires soft tissue transfer to achieve coverage.
IIIc- Associated vascular injury that requires repair for limb preservation.
Gunshot injuries with vascular damage can be life threatening and occur in 5% of the time (6, 14) .The mechanism of popliteal artery injury is penetrating in 39–51 % of patients, and gunshot injuries are the main cause of such dangerous lesion (6, 14, 21-24), that can lead to amputation or massive blood loss. Another site of vascular damage in gunshot injuries is the superficial femoral artery.
The presence of major signs of vascular injury are indicators of immediate surgical exploration (14) . In the presence of minor signs with ankle-arm index less than 0.9, further investigation with imaging tests is necessary. The examination begins with palpation of the wrists. Absence of a pulse is not a reliable sign, but it is important for further investigation or immediate surgery. The absence of a pulse can be a false positive sign in shocked patients and it can occur due to segmental vasospasm, use of dressings and compressive molds, congenital absence of pulse and pre-existing vascular diseases. False negative signs are found in cases of strong collateral circulation. Based on the clinical examination, the patient is assigned to one of the three categories that determine the diagnosis and management plan:
Category 1 (major signs): include pain, pallor, absence of pulse, paraesthesia, paralysis, pulsatile bleeding and large or expanding hematoma. If the patient shows these signs, he will have a> 90% chance of vascular injury.
Category 2 (Minor signs): includes a relatively reduced but palpable pulse, non-expandable hematoma and peripheral nerve damage; 30-35% of these patients will have vascular injury.
Category 3 (high risk - asymptomatic): includes penetrating wounds 1 cm from the main areas of the neurovascular bundle (for example, axillary, femoral and carotid) and knee dislocations or long bone fractures with severe displacement. Up to 15-20% of these patients have vascular injury.
The types of vascular injury can be:
Complementary Exams
The radiographs of the affected segments and their adjacent areas are taken after the initial evaluation. It is very important that the patient is bandaged and immobilized before going to the imaging sector to avoid further infections and injuries. Laboratory tests such as complete blood count, TAP, PTT, blood typing, RH factor and cross-examination also help in the evaluation, especially in patients with active bleeding and suspected shock and in need of blood transfusion. Other exams such as CT, MRI and US are useful, but can be requested later. They are not the priority in assessing gunshot injuries at the Emergency Room.
Patients who present with significant clinical instability, apparent ischemia or active bleeding are referred directly for surgical intervention. However, complementary exams are indicated to assess the presence or absence of vascular injury when the patient has no major signs and is hemodynamically stable. Tests should be ordered to prevent unnecessary surgery, document the presence of a surgical injury and plan for surgical treatment (14, 25-27) Arteriography can be performed in the emergency room or in the operating room and has long been the gold standard in vascular assessment, but it has gradually been replaced by angio-tomography in the study of vascular lesions (25-27). However, it is the exam of choice when an endovascular intervention is being considered.
Doppler ultrasonography has the advantage of being performed at the bedside in critically ill patients, it gives an image of the vessels and their lesions in real time, but it has the disadvantage of requiring a trained doctor and being an operator-dependent examination.
Magnetic resonance imaging has many limitations because the acquisition time of the images is very long and is contraindicated when the patient has metallic fragments, such as fragments of a firearm.
Angiotomography had its accuracy increased with the sophistication of the devices and the accumulated experience in the interpretation of the findings, being today the most requested image exam in the emergency room, especially in the decision to treat the vascular injury by open surgery or by endovascular techniques (14, 25-27) TABLE 2. It has the advantage of assessing, together with vascular lesions, the presence of lesions in other organs or tissues. For this it is always necessary to perform a full scan with a phase without contrast, an arterial phase and a late phase. The most frequent findings in the diagnosis of vascular injury are: contrast leakage, narrowing of the contrast column and luminal dilation.
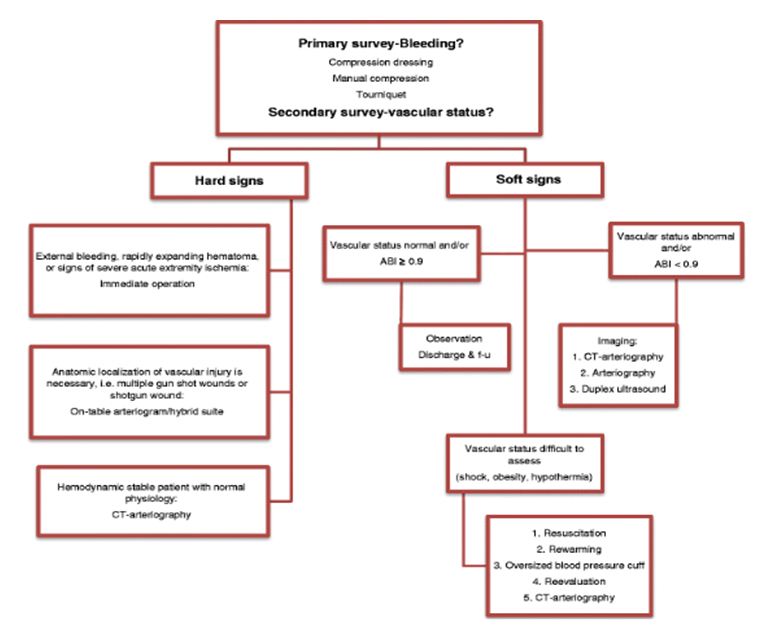
Table 2: Clinical presentation and management algorithm in penetrating extremity vascular trauma (modified from the Western Trauma Association) (14, 26)
Treatment
The treatment of firearm fractures follows the same principles as the treatment of open fractures, paying attention to some peculiarities about the circumstances of the trauma, especially the environment in which they occur and the biomechanics of the trauma. Any fracture with a wound or hematoma in contact with the external environment is considered an open fracture and should be treated as an Emergency, due to the great risk of complications. Intravenous antibiotic therapy is routine for open fractures, although some studies report that patients with grade I lesions do not need antibiotic therapy (28).
In our practice, in which many patients experience trauma in rural areas and in areas of the Amazon rainforest, we chose to administer an initial dose of 2 g of intravenous cephalosporin, followed by an additional 5 days of treatment. In less contaminated lesions, this dosage is performed in a single dose. In hospitalized patients, antibiotic therapy is performed for a period of 48h to 72h, depending on the degree of exposure and contamination. In these cases, the choice is a combination cephalothin, gentamicin and metronidazole for 5 days.
Soft tissue care is described as one of the main factors to prevent infections. Some works on open fractures question the “6 hours rule”, considered the ideal time to start treatment (29-35). In high-energy and highly contaminated injuries, however, early treatment has been identified as an important factor to prevent infections (11, 12, 29, 30, 33, 34). Despite the controversies, there is a consensus that venous antibiotic therapy and meticulous debridement are the most effective initial approaches in preventing infections in firearm injuries and exposed fractures in general (6, 11, 12, 15, 20).
Another point of controversy is skin coverage, which can be primary and immediate, or delayed for 48 to 72 hours. Recently, Ukai and cols, in a retrospective study published in 2020, observed that few studies have focused on how to cover soft tissue loss in order to prevent deep infection (41). In injuries with great loss of bone substance and soft tissue, it has been observed that after cleansing and debridement, early bone coverage with local muscle flaps and filling in remaining spaces left by severe tissue loss may favor better results (36-44), combined with prolonged antibiotic therapy (45-49). Severe exposed injuries have been being treated using soft tissue coverage techniques with local flaps and even microsurgical procedures (TABLE 3). At this stage, the presence of a Plastic Reconstructive Surgeon can be extremily useful in the surgical procedure, since these procedures are not so familiar to Orthopaedic Surgeons (40).
Table 3- Operative Sequence Of Treatment In A Gunshot Fracture Gustilo Iii With Tissue Loss (Author's Archive)

A- Initial presentation if the lesion (Author’s archive).
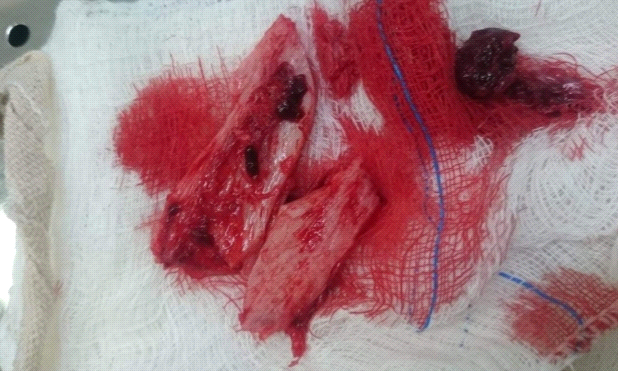
B- Excision of devitalized bone fragments (Author’s archive).

C- Aspect of debridated lesion with bone exposion and "dead space" (Author’s archive).

D- Initial management of the local flap with dislocation of adjacent viable tissue to the affected area (Author’s archive).

E- Suture of the flap and filling of the "dead space" (Author’s archive).

F- Final bone coverage with local muscular flap (Author’s archive).

G- Subtotal skin coverage (Author’s archive).
The projectile fragment is not routinely removed, except in cases with joint block, when there is risk of injury to other structures such as peripheral nerves and vessels and in patients with lead poisoning. Fragments located in the subcutaneous tissue, in an easily accessible location, can be resected. The risk-benefit of these excisions should always be evaluated, in order not to promote further tissue damage, to avoid bleeding and infections. In isolated places or with few resources, it is recommended to transfer the patient to a trauma center before performing soft tissue procedures (40, 50, 51). During the period, the wound should be protected with a clean dressing, antibiotic therapy and venous hydration.
Regarding the fixation methods, there has been controversy regarding the technique and implant used in the first moment. Surgical cleaning and debridement followed by immediate permanent fixation has been advocated in Gustillo grade I, II and IIIA fractures by firearms, especially in large-scale trauma services in urban centers in developed countries (11,12). In type III B and IIIC fractures, external fixation is performed and, with the improvement of soft tissue conditions, definitive osteosynthesis (11,12). In war situations and in remote places, or with few resources, early internal fixation of exposed fractures and firearms has been avoided and the most prudent approach has been considered cleaning, surgical debridement and immediate and temporary external fixation (11, 12 , 40, 24, 25). In our service, we treat open fractures with external fixation, regardless of the degree of exposure. Subsequently, these patients undergo definitive osteosynthesis in a period ranging from 7 to 14 days. In grade III C injuries, the approach is external fixation, sometimes definitive.
Fracture stabilization with external fixation is ideally prior to vascular treatment, which is another point of controversy. Some studies in Trauma Vascular Surgery believe that Vascular repair must occur before fracture estabilization with Major Vascular Injuries from Gunshot Wounds. We believe that the good sense is always the best option and that decisions are taken in accordance of both professionals, Orthopaedic and Vascular Surgeons. For example, rapid external fixation of an unstable gunshot femoral fracture can be an excellent option before definitive vascular repair or shunt. On the other hand, patients with massive blood loss, severe ischemia, vascular procedures should be prior to bone fixation. (11, 12)
Low to moderate bleedings can be controlled by compressive dressings. Large hematomas can be best explored by proximal control of the uninjured part of the vessel through tissue adjacent to the injury site. However, active massive bleedings sometimes need to approached by direct digital control.
The general principles of surgical correction of traumatic vascular injury to the vessels of the extremities begin with the use of a radiolucent operating table, availability of tourniquets, balloons for temporary occlusion, Fogarty catheters and temporary shunts.
Vascular firearm injuries are associated with hemorrhage and ischemic issues. In the Second World War, patients treated via vascular ligation suffered amputation rates as high as 48.9%. As vascular prostheses improved, the amputation rates in the Korean and Vietnam Wars fell to 13%. In the recent Iraq War, the early amputation rate was only 5% to 10%.(1-8, 40)
The extent of blood vessel damage is often greater than evidenced by Physical Exam. Debridement remains controversial. Some authors consider that tissue around high-speed bullet wounds should be removed within a diameter of 1 cm, and that around low-speed wounds within a diameter of at least 3 mm, so that microscopic damage will not compromise blood vessel wall repair (3, 8). As a matter of fact, many surgeons simply remove the visible portions of the injured vessels to avoid infection and ensure high-quality repair (3, 8, 52, 53).
Close and distal thromboembolectomy should be performed when proximal and distal blood flows do not occur properly, taking care not to cause further endothelial damage, as well as extensive debridement of the contaminated area with removal of all non-viable tissue. Systemic heparinization, which is routinely used in elective arterial surgery, has many contraindications in the treatment of vascular trauma, such as a patient with associated traumatic brain injury or the presence of other bleeding sources. Locoregional heparinization is recommended during the surgical procedure. The importance of effective correction of these injuries favors the early rehabilitation of these patients. Injuries that are not effectively corrected can lead to serious complications, from functional limitations to limb loss.
A cardinal operative principle in the management of an important vascular injury is to obtain proximal and distal control of the injured vessel. At the extremities, control is achieved using standard longitudinal vascular exposure techniques. In severe injuries, a temporary shunt may be indicated before definitive vascular repair (14, 26, 27) TABLE 4

Table 4: Operative management algorithm in penetrating extremity vascular trauma (modified from the Western Trauma Association) (14, 27)
The choice of conduit depends on the anatomical site and the availability of an adequate venous graft. The reverse great saphenous vein of the contralateral limb remains the standard conduit for the repair of vascular lesions. However, the diameter discrepancy between the graft and the vessel to be treated, the unavailability of an adequate vein, the longer surgical time for removal and graft preparation may indicate the use of a heterologous graft.
The advantages of using PTFE (Polytetrafluoroethilene) prosthetic grafs of are the immediate availability of the graft and the greater resistance to infection when compared to other synthetic grafts and that PTFE kills its structural integrity during infection, with a low rate of anastomosis and bleeding dehiscence .
Currently, endovascular treatment has shown beneficial results mainly in circumstances of hemodynamic stability, and for treatment in places of difficult access. Endovascular treatment may include placement of an endoprosthesis / stent or embolization of vessels that have active bleeding and cannot be corrected (54, 55). The endovascular approach has the advantages of shorter surgical time, less blood loss, can be used as a temporary repair of the lesion and can access complex anatomical regions or where there is greater difficulty in controlling bleeding.
Eventually, compartment syndrome may occur and fasciotomy is applied when there is prolonged ischaemia. Fasciotomy should be performed liberally and prophylactically, not only in cases of prolonged ischemia, massive volume resuscitation, injury to the popliteal artery, associated venous and musculoskeletal injury (56).
Nursing Care
The importance of nursing care and intervention has been recognized as a determinant factor for good results in the evolution of wounds (57).
The immediate postoperative follow-up in gunshot injuries is carried out with special attention to the conditions of the soft tissues, dressing changes and nursing care. In this sense, daily assessment and whenever necessary of the peripheral perfusion of the affected limb and keeping it warm and elevated is of fundamental importance. With regard to patients undergoing external fixation of the exposed fractures of the above types, with corrected vascular injury, in which there are risks for Compartmental Syndrome and Pulmonary Thromboembolism, the focus is on daily inspection, superficial palpation of the limb, evaluation of SpO² and breathing pattern. Signs of infection of the lesions should also be assessed daily (58).
In type III B and IIIC fractures, in which external fixation is performed, the dressing is performed with initial care of the soft tissues with a 0.9% saline jet and antiseptic solution, as well as elimination of devitalized tissue. The coverings of open lesions - as is the case in which it was necessary to perform fasciotomy - are performed with special attention in keeping the medium moist for granulation tissue proliferation. In this case, in our hospital routine, the Hydrogel or Rayon Gauze is used as the primary cover. Subsequently, secondary occlusive coverage is performed with sterile gauze on the wound and primary coverage also with gauze at the insertion sites of the fixators. Finally, these must be disinfected with alcohol 70% from the proximal to the distal region, in a single movement. The dressing is changed every 24 hours or whenever necessary (58-60).
Vaccum assisted dressing is a good choice for management of open fractures and can be more effective than conventional dressings (57). Unfortunatelly, this technique is not available in all hospitals. In Brazil, although it has been recognized as an excelent choice for severe open fractures, many trauma centers do not have it.
Complications
The main complications of firearm fractures are infections, healing disorders and pseudoarthrosis. The control of hemorrhage, care for the soft tissues and antibiotic therapy are essential to prevent infection, especially in high-energy injuries. In these cases, delayed skin coverage can be beneficial until the edema and the wound conditions show a substantial improvement (29). The literature is not conclusive as to the benefits of serial debridement, vacuum dressings with negative pressure or other adjuncts can be useful in reducing the high infection rates of these lesions.
When extremity fractures are associated with vascular injuries, the main complication is failure in vascular correction with consequent ischemia and progression to amputation of the affected limb. In the immediate postoperative period, we may have reperfusion syndrome, which can lead the patient to shock and acute renal failure, in cases where the patient has undergone prolonged limb ischemia. Compartmental syndrome can also occur when fasciotomy was not performed in the first surgical approach.
Conclusions
Injuries of firearms of extremities are challenging and potentially complicated. The fisrt approach is determinant for better results, independently from the circunstances. Low energy injuries can be treated with soft tissue care, limited antibiotics and definitive early osteheossynthesis with lower rates of complications. High energy and contaminated with extensive soft tissue loss, contamination and vascular injuries have higher rates of complications, such as deep infection and pseudoarthrosis. Such injuries are better treated with soft tissue care, extensive debridement, broad and prolonged antibiotics, external fixation and vascular repair/shunt, when necessary. Although its controversies towards time of delay, bone /skin coverage and the methods of initial fracture fixation in severe lesions, effective and coordinated multidisciplinary approach at the Emergency Room is determinant for better results in firearm injuries of extremities.