Orthopaedic Research and Surgery
OPEN ACCESS | Volume 5 - Issue 1 - 2025
ISSN No: 2994-8738 | Journal DOI: 10.61148/2994-8738/JORS
Mohammed Shahid, Fardeen Shariff, Sharat Balemane
Yenepoya Medical College, Deralakatte, Mangalore, India
*Corresponding Author: Mohammed Shahid, Yenepoya Medical College, Deralakatte, Mangalore, India.
Received date: March 05, 2021
Accepted date: March 25, 2021
Published date: April 02, 2021
Citation: Md Shahid, F Shariff, Sharat B. “Association between Body Mass Index and Bone loss in Osteoarthritis of the Knee – A cross sectional study’’. J Orthopaedic Research and Surgery, 2(1); DOI: http;//doi.org/03.2021/1.1008.
Copyright: © 2021 Mohammed Shahid. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
,
Introduction
It is a well-known fact that obesity is an important and a modifiable risk factor in the development of osteoarthritis of the knee [1,2]. Accordingly, weight loss is a recommended choice for the treatment or to delay the progression of osteoarthritis [3] and its short-term results are comparable to that of a joint replacement surgery [4]. In the elderly, studies have shown that weight loss of as little as two BMI units over a period of 12 years has reduced the risk of knee OA [5]. However, there is no definitive data on whether weight loss is beneficial for reducing progression of structural changes in OA, but available data from various studies support the fact that weight loss and exercise interventions slow the disease progression [3]. As OA knee is a slowly progressive disease, it is generally agreed that the disease modifying factors with respect to the structural changes in the knee should be assessed at the earliest.
While the evidence in favor of weight loss and weight loss maintenance with respect to symptomatic relief is indisputable, the effects of weight loss on progression of structural disease is not well documented. Ananda-coomarasamy et al [6]. showed that weight loss was associated with reduced loss of cartilage thickness and proteoglycan content over 12 months in a cohort of mixed OA and non-OA obese individuals.
We hypothesized that with increased body weight there is increased bone loss and progression of osteoarthritis of the knee.
Materials And Methods
Patient selection
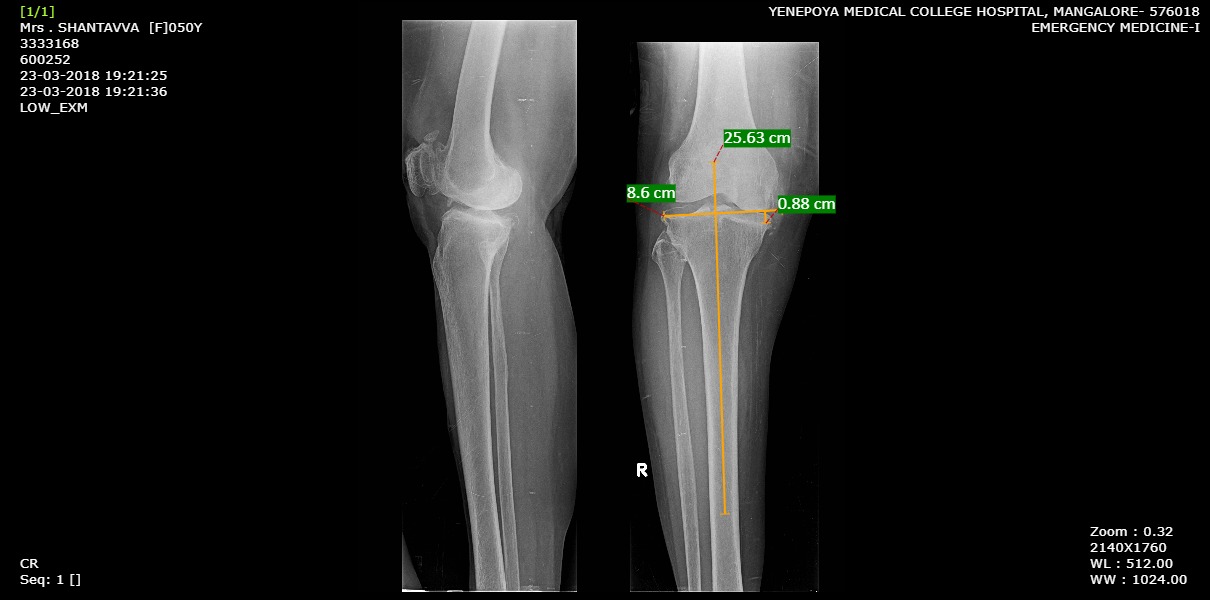
After obtaining the approval from our institutional ethics committee and obtaining informed consent from our patients, 60 patients, aged above 50 years, diagnosed with primary osteoarthritis of the knee were evaluated on OPD basis. Relevant clinical data (demographic- age, gender, place, occupation, weight, height) including chief complaint and clinical examination was obtained. BMI was calculated as a ratio of weight (in kilogram) by square value of height (in metres). Radiological assessment was done by obtaining a standard AP and Lateral view x ray of the involved knee joint. Kellgren-Lawrence (KL) grading for Osteoarthritis Knee was applied where Grade 0: No radiographic features of osteoarthritis, Grade 1: Doubtful narrowing of joint space, possible osteophytic lipping, Grade 2: Possible narrowing of joint space, definite osteophytes, Grade 3: Definite narrowing of joint space, moderate multiple osteophytes, some subchondral sclerosis, possible deformity of bone ends, Grade 4: Marked narrowing of joint space, large osteophytes, severe subchondral sclerosis, definite deformity of bone ends. Patients with KL grade ≥2 were taken into the study. The bone loss was measured radiologically using the Ahlbäck classification through the use of hospital PACS software.
Assessment of radiographs
Standard Antero-posterior and Lateral view weight bearing radiographs of the knee were taken. The bone loss was calculated as the bone defect in mm at the medial tibial plateau when a line is drawn from the lateral tibial plateau perpendicular to the long axis of the tibia. All films were assessed in a blinded manner. The Ahlbäck and Rydberg [7] grading was applied to assess the severity of bone loss where Grade 1: narrowing of the articular space; Grade 2: obliteration of the articular space; Grade 3: bone attrition less than 5 mm; Grade 4: bone attrition between 5 and 15 mm, and Grade 5: bone attrition greater than 15 mm.
Inclusion criteria
Exclusion criteria
Statistical analysis:
Data was entered in the Microsoft Excel and analysis done using SPSS Version 22.
Descriptive Statistics were reported for the required outcome variables (Frequency, Percentage, Mean, Standard Deviation).
Results:
Of the 60 patients included in the study, 27 were male and 33 were female in the age group of 50-74 years with a mean age of
61.86 years. 22 patients presented with OA knee of right side while 38 presented with OA knee of left side compared to the other side. The mean BMI of the population sample was 29.07±4.29. 24 patients had pre-existing co-morbidities (Diabetes Mellitus/Hypertension/Both).
The mean bone loss in the sample population was found to be 10.233±4.65mm, ranging from 1.8-24.7mm.
Patients were graded as per Kellgren Lawrence grade based on the severity of Osteoarthritis on radiographs. Of the 60 patients, 11 had grade 2 changes, 29 had grade 3 and 20 had grade 4 osteoarthritis. The bone loss was measured using the hospital PACs software and assessed using Ahlback’s grading. 2 patients belonged to grade 2 and grade 3 each, 33 patients belonged to grade 4 and 23 patients belonged to Ahlback grade 5.
|
Variables |
Range |
Mean (SD) |
Count (Percent) |
|
Age (years) |
50 -74 |
61.86 (6.696) |
|
|
BMI |
20.7-35.8 |
29.07 (4.29) |
|
|
Gender: Male Female |
|
|
27 (45) 33 (55) |
|
Bone loss (mm) |
1.8-24.7 |
10.233 (4.65) |
|
|
Co-morbidities |
|
|
24 (40) |
|
Side: Right Left |
|
|
22 (36.66) 38 (63.33) |
Table 1: Descriptive analysis of the patient data
It was found that there was a positive correlation between the BMI and bone loss based on Ahlback’s grading. However, this correlation was not found to be statistically significant.
|
Variables |
Count (Percent) |
||||||
|
KL grade: 2 3 4 |
11 (18.33) 29 (48.33) 20 (33.33) |
||||||
|
Ahlback grade: 2 3 4 5 |
2 (0.033) 2 (0.033) 33 (55) 23 (38.33) |
||||||
|
BMI
18.5-24.9 25.0-29.9 30 and above |
KL grade |
Ahlback grade |
|||||
|
2 |
3 |
4 |
2 |
3 |
4 |
5 |
|
|
2 5 4 |
7 5 17 |
3 11 6 |
1 1 0 |
1 0 1 |
6 11 16 |
4 9 10 |
|
|
Pearson’s correlation (r) P value |
0.126 0.3374 |
||||||
Table 2: Correlation between BMI and the bone loss
Discussion:
Prospective studies have shown that obesity and excess weight are the risk factors for knee osteoarthritis [8,9,10]. They are also risk factors for abnormal lower limb alignment, as this places excessive loads on the tibial plateau [11,12]. These excessive loads, no matter the cause, induce premature cartilage wear, probably by direct action. However, the pathophysiology is more complex and involve many other indirect phenomena [8].
Heightened precision and accuracy of radiographic classification of knee OA would be beneficial in facilitation of preoperative planning. It would reduce the degree of uncertainty concerning the choice of technique and implant, and also the surgical skills necessary to perform the operation. The Ahlback classification is probably the most frequently used system for classification of knee osteoarthritis in severe stages. The staging used today in the Ahlback classification was not described until 1980 (Ahlback and Rydberg 1980). In a study, consisting of 359 patients with medial OA, the distribution between the 5 stages varied between 3% and 38%, a scatter which Ahlback regarded as acceptable to test the value of his classification system [14].
According to radiographs presented in his thesis in 1968 [13], Ahlback was aware of some cases with obvious bone attrition despite the presence of a visible joint opening, but did not comment on this problem.
Thirty-seven years after the original concept was presented by Ahlback, it was confirmed that bone attrition is an additional radiographic dimension of knee OA. The assessment of this is useful primarily in monitoring the advanced stages of knee OA.
Our study assessed the bone loss at the medial tibial plateau radiographically and it was correlated with the BMI of the patients.
Ahlback grading is associated with a significant inter and intra-observer bias which was eliminated in our study using standard x rays and hospital PACS software for the radiographic measurements of bone loss.
It was found that, there was a positive correlation of BMI with increased bone loss. However, this was statistically not significant.
The limitations of our study were a limited sample size, which may not be generalized to the population. The Ahlback grading system cannot be used to evaluate cases with lateral OA [14].
Conclusion:
Even though BMI influences the severity of bone loss and Osteoarthritis, this correlation was not found to be statistically significant. A larger study may be required to strengthen the association between BMI and bone loss in Osteoarthritis of the knee.