Orthopaedic Research and Surgery
OPEN ACCESS | Volume 6 - Issue 1 - 2026
ISSN No: 2994-8738 | Journal DOI: 10.61148/2994-8738/JORS
Yogesh Kumar Balasubramanian 1, Ajay Kumar Shetty Papanna 2, Vidyadhara Srinivasa 3
1Department of Orthopaedics, Chettinad Hospital and Research Institute, Kelambakkam, Tamil Nadu, India
2HOD & Consultant, Department of Spine Surgery, Manipal Hospital, Bangalore, India
3Clinical Spine Fellow, Department of Spine Surgery, Manipal Hospital, Bangalore, India
*Corresponding Author: Vidyadhara Srinivasa, HOD & Consultant Spine Surgeon, Department of Spine Surgery, Manipal Hospital, Bangalore, India
Received date: December 08, 2020
Accepted date: December 15, 2020
Published date: December 18, 2020
Citation: Yogesh K Balasubramanian, Shetty Papanna A K, Srinivasa V. “Spinal Tuberculosis Presenting as Immune Thrombocytopenic Purpura – a Case Report.’’. J of Orthopaedic Research and Surgery, 1(1); DOI: http;//doi.org/03.2020/1.1001.
Copyright: © 2020 Vidyadhara Srinivasa. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
The association of ITP with tuberculosis is rare. Although very few case reports of Pulmonary and Lymph Nodal tuberculosis associated with immune thrombocytopenic disorder, there are no reports of Musculoskeletal Tuberculosis with ITP. We present a 30-year-old man with low platelet counts was treated with intravenous steroids and immunoglobulins for almost six weeks but in vain. The patient also suffered upper backache which on MRI was diagnosed to be infective spondylodiscitis T7-8. Closed vertebral biopsy revealed tuberculosis. Patient was started on anti-tubercular medications. Patient had steady increase in platelets on anti-tubercular treatment to reach normal levels in six weeks. Tapering and stopping of anti-thrombocytopenic medications after three months did not cause relapse in ITP. At two years of follow up patient was cured of tuberculosis and had complete remission from Thrombocytopenia.
Introduction:
Immune Thrombocytopenic Purpura (ITP) secondary to tuberculosis of spine has not been described in the literature. We herewith report the first case of tuberculosis of spine presenting as ITP. The purpose of the study is to emphasize that TB to be considered as one of the causative factor in ITP, so that the treatment related complications of ITP can be avoided. Medical treatment of tuberculosis seems restore the platelet levels to normal over time.
Case report:
A 30-year old male with upper backache and girdle pain of one month duration presented to Hemato-oncologist with Thrombocytopenia. He had no fever, constitutional symptoms or diabetes mellitus. Patient had localized tenderness over mid-thoracic spine and grade 1 paraparesis (exaggerated ankle jerks, clonus and extensor plantar reflexes bilaterally). Clinical examination revealed no organomegaly or lymphadenopathy. Blood picture was as follows: RBC Count 5·4 million/mm3, WBC count 9800/mm3, Platelet count was 2000/mm3, Hemoglobin 15·6g/dL and ESR was 30 mm/hour. Peripheral smear demonstrated thrombocytopenia, with normal red blood cells and white blood cells. The bone marrow was normocellular with normal myeloid to erythroid ratio of 3:1 and no abnormal cells. His serology for HIV, HBsAg and HCV were negative. X-rays of the thoracic spine (anteroposterior and lateral views) showed spondylodiscitis of T7-8 with para-vertebral abscess (Figure 1).
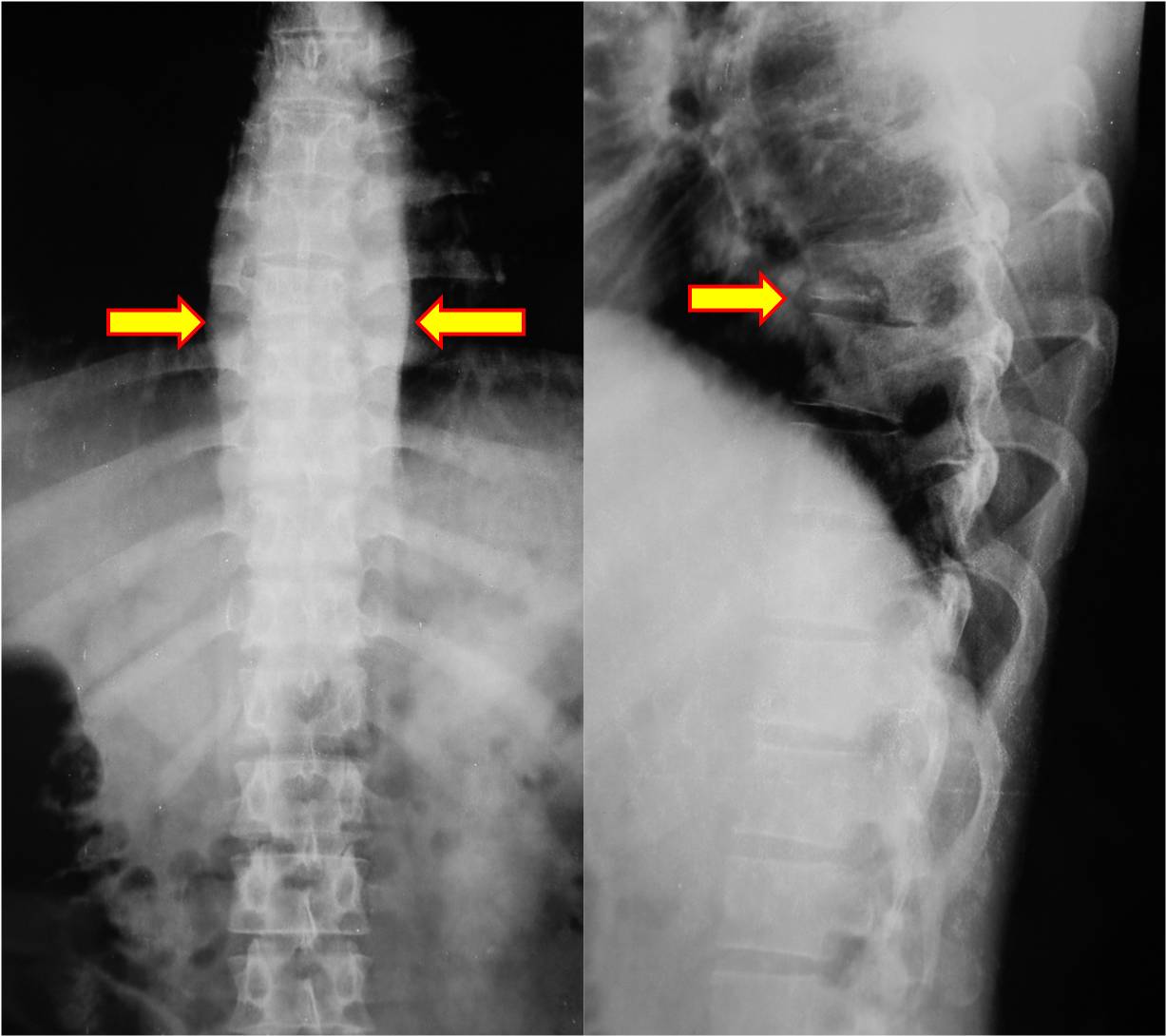
Figure 1: Radiographs of thoracic spine (anteroposterior and lateral views) showing spondylodiscitis of T7-8 with para-vertebral abscess.
MRI of spine revealed infective spondylodiscitis of T6-7 and T7-8 with pre- and para-vertebral abscesses along with significant epidural component compressing the thecal sac (Figure 2).
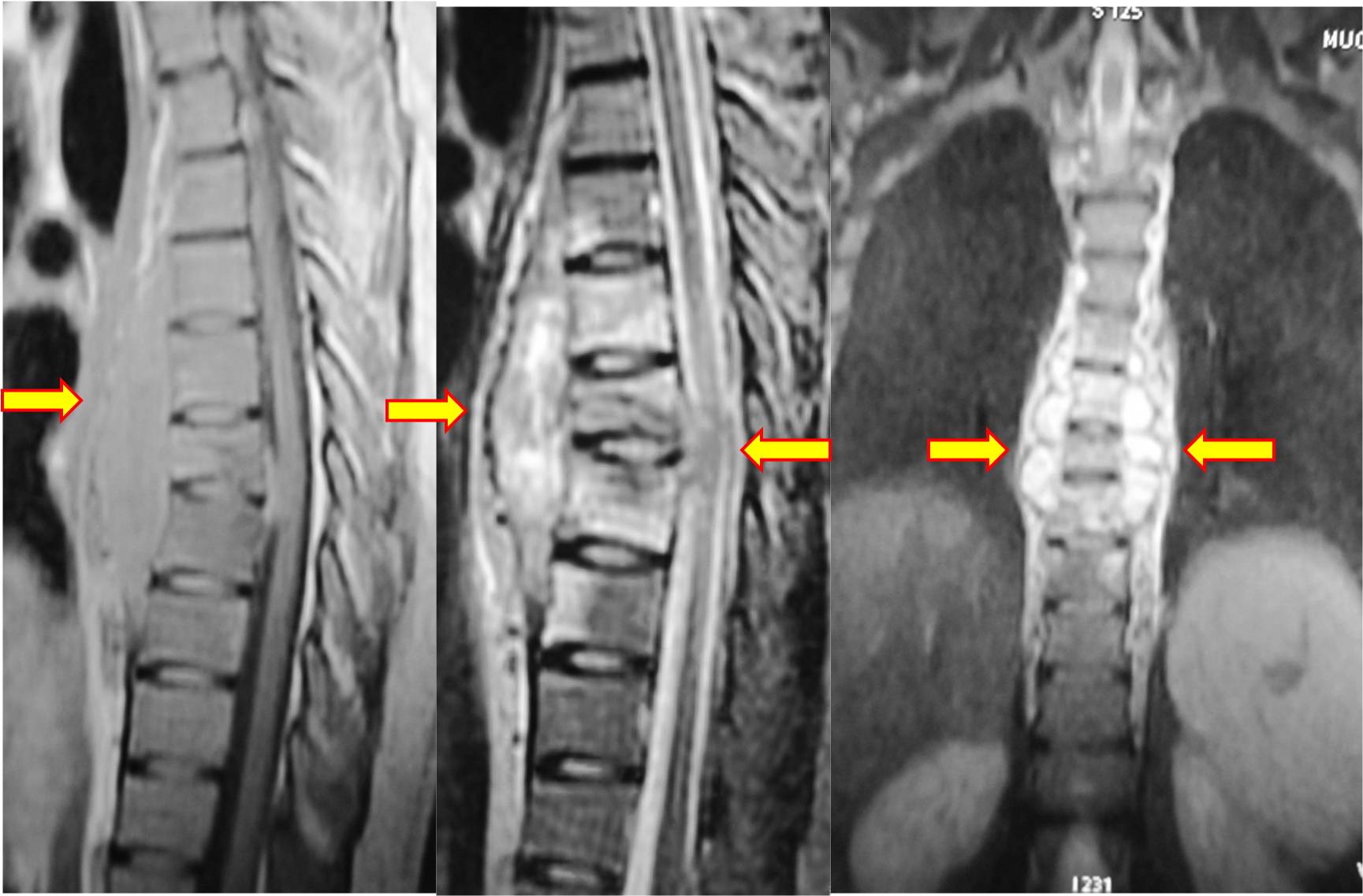
Figure 2: MRI of the thoracic spine in coronal and sagittal views (T1- & T2-weighted images) showing infective spondylodiscitis of T6-7 and T7-8 with pre- and para-vertebral abscesses along with significant epidural component compressing the thecal sac.
In view of very low platelet count, closed vertebral biopsy was not attempted initially.
From the above parameters, he was diagnosed to have Immune Thrombocytopenia and was started on high dose steroid therapy with Methyl Prednisolone 1g/day for two days. He developed generalized purpura and his platelet count had dropped to 1000/cu.mm. He was given platelets transfusion to prevent further bleeding and was started on human immunoglobulins 1g/kg/day. In view of ineffectiveness, the steroids were changed to oral Prednisolone 20mg thrice daily. Despite being on steroid and immunoglobulin for over one week, he did not respond. Meanwhile, patient developed steroid induced diabetes which was controlled with diet modifications, regular monitoring of blood glucose and insulin injections.
He was taken up for percutaneous fluoroscopy guided trans-pedicular biopsy from T7 vertebra which diagnosed Spinal Tuberculosis. He was started on anti-tubercular drugs (4-drug regimen) and discharged on Prednisolone 60mg/day. At the time of discharge his platelet count was 13,500/mm3 and ESR 25mm/hour within a week of Anti-Tubercular medications. After two weeks of Anti-Tubercular medications, the platelet count improved to 49,000/mm3. Prednisolone was tapered gradually over a period of next three weeks. The platelet count reached normal of 2,25,000/mm3 and ESR was 7·5mm/hour at six weeks follow-up. All other medications were stopped and he was continued only on standard anti-tubercular medications for a period of twelve months. At two-year follow-up the patient had a normal platelet count with complete remission of the immune thrombocytopenia and healed Pott’s Spine T7-8 with bony ankylosis.
Discussion:
Tuberculosis still exists in developing countries and it has been described to present as a variety of clinical syndromes. Hematological disorders such as anemia, pancytopenia, leucopenia, leukocytosis, monocytosis, lymphopenia, thrombocytopenia, thrombocytosis, leukemoid reactions etc. have all been described secondary to tuberculosis [1,2] Thrombocytopenia in tuberculosis can occur as a result of granulomatous infiltration of bone marrow and as well as due to histiophagocytosis, thrombotic thrombocytopenic purpura (TTP), disseminated intravascular coagulopathy (DIC), immune-mediated platelet destruction or side effect of anti-tuberculous therapy particularly rifampicin [3,4]
Isolated thrombocytopenia via immune mechanism due to tuberculosis is rare and there are only few case reports in literature suggesting its association [5, 8]. Most of the reports are associated with pulmonary tuberculosis 33%, tubercular lymphadenitis 19% and disseminated tuberculosis in 19% [9].
The pathogenesis of immune mediated thrombocytopenia in tuberculosis is controversial. Tuberculosis infection stimulates suppressor monocytes activity together with reduction of the T-lymphocytes. Moreover, purified protein derivative of tuberculin may be a non-specific B- lymphocyte stimulator. Jurak et al postulated that the mycobacterium tuberculosis stimulates B-cell nonspecifically and the antibodies thus produced destroy platelets [10]. Boots RJ contradicted the above as he could not find any such antibodies against mycobacterium and the antibodies that were found against platelets were also nonreactive to other donor platelets [11]. We believe that thrombocytopenia in tuberculosis is mainly due to antigenic mimicry, whereby antibodies targeting the micropathogens cross-react with platelet glycoproteins resulting in accelerated platelet clearance.
Immune thrombocytopenia purpura is diagnosed based on decrease in platelet count in a previously healthy patient with normal blood counts, normal peripheral smear, and after exclusion of other causes of thrombocytopenia. The identification of these auto-antibodies has no role in either diagnosis or treatment [12].
In the reported case a platelet count of less than 2000/cc3, made us to defer a closed vertebral biopsy from the spinal lesion initially for the fear of bleeding. Eventually when the closed vertebral biopsy was performed, the platelets were as low as 1,000/cc3 and there was no procedure related complication. Hence we can infer that closed vertebral biopsy in thrombocytopenic conditions can be performed safely as the needle is going into a vertebra with intact posterior cortical shell and the bleeding would stop by tamponade effect. However, non-responsiveness of thrombocytopenia to steroids and immunoglobulin and histopathologically proven spinal tuberculosis, made us suspect patient immune thrombocytopenia purpura secondary to spinal tuberculosis. Predictably, the platelets started increasing with anti-tubercular treatment. The diagnosis of secondary immune thrombocytopenia purpura was confirmed and the steroids were tapered gradually and then stopped. On stopping the steroids, thrombocytopenia didn’t recur and his platelet count and glucose level remained normal, which reconfirmed tuberculosis as a cause for immune thrombocytopenia purpura.
Conclusion:
This is the first reported case of spinal tuberculosis causing Immune Thrombocytopenic Purpura in the literature. It proves that ITP secondary to tuberculosis has a good prognosis as the condition remits completely when tuberculosis is controlled and can be managed only with anti-tubercular drugs without the need for immunosuppression [13, 14]. This will avoid the unnecessary treatment of the ITP with immunosuppression and related complications.