Neurosurgery and Neurology Research
OPEN ACCESS | Volume 7 - Issue 1 - 2025
ISSN No: 2836-2829 | Journal DOI: 10.61148/2836-2829/NNR
Mohammed H Habib
Department of Cardiology and Cardiac Catheterization, Al-Shifa Hospital, Gaza, Palestine
*Corresponding author: Mohammed H Habib, Department of Cardiology and Cardiac Catheterization, Al-Shifa Hospital, Gaza, Palestine.
Received date: November 12, 2022
Accepted date: November 21, 2022
published date: December 21, 2022
Citation: Mohammed H Habib, (2022) “A Case Study and Assessment of the Literature Regarding Multiple Cerebral Hydatidosis”. J Neurosurgery and Neurology Research, 4(3). DOI: http;//doi.org/12.2022/1.1046.
Copyright: © 2022 Mohammed H Habib. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
The management of synchronous cardiocerebral infarction poses a great challenge for the clinician. Both acute ischemic stroke and ST segment elevation myocardial infarction are emergencies with different treatment strategies in the acute phase. The main goal is timely reperfusion of both the cardiac and cerebral circulation. The aim of this case report is to describe the diagnosis, causes clinical profile and treatment outcomes of patients with synchronous CCI.
Introduction
Cardiocerebral infarction (CCI) is the rare occurrence at the same time (synchronous) of acute ischemic stroke (AIS) and acute ST elevation myocardial infarction (STEMI), with an incidence of 0.009%.(1)
The order in which percutaneous coronary intervention (PCI) for AMI and endovascular thrombectomy (EVT) for AIS are performed is also controversial since performing one ahead of the other leads to compromise of either the heart or the brain.
Case report
A 61-year-old patient without history of any chronic illness. right-handed, independently functioning man, the patient was admitted to our emergency department due to chest pain since 9 hours with heart rate of 140 beats/min and blood pressure (BP) of 110/60 mmHg. Emergency ECG showed sinus rhythm, ST elevation in anterior leads (Figure 1). Intravenous streptokinase 1.5 million unit given over I hour was given in emergency room. After 90 minutes the ECG suggested failed thrombolytics and ST elevation still the same. Then the patient transport to coronary care unit with stable condition. After 4 hours a sudden, witnessed onset of slurred speech and right-sided weakness. He is alert with severe aphasia, facial weakness on the right side, and weakness in the right arm and leg with decreased sensation to light touch and severe agitation. His plasma glucose level 92 mg per deciliter with NIHSS of 21, BP:60/30 mmHg, HR: 150/min/regular Urgent noncontrast computed tomography (CT) of the head shows slight hypodensity and left middle cerebral artery hyperdense with no hemorrhagic conversion (figure 2)

Figure 1: ECG in emergency room, sinus tachycardia, anterior ST elevation

Figure 2: brain noncontrast computed tomography (CT) shows slight hypodensity and left middle cerebral artery hyperdense with no hemorrhagic conversion
After discussion with the patient with family and medical team, a decision was made to proceed with emergency cerebral and coronary angiogram keeping in mind the risk of intracerebral hemorrhagic conversion.
Under general sedation selective cerebral angiography and suggested left middle cerebral artery MCA occlusion ,urgent after thrombus aspiration was done and TICI floe2b/3 was seen. Figure 3a, 3b
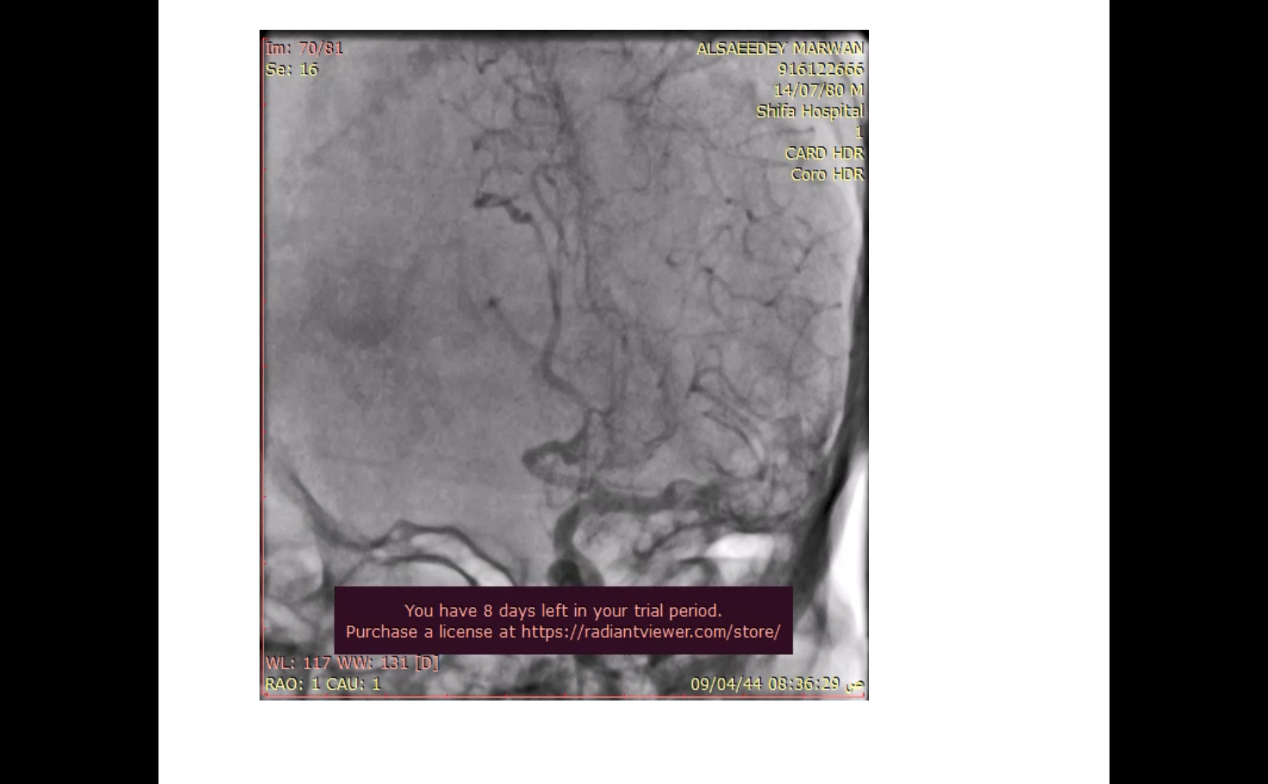
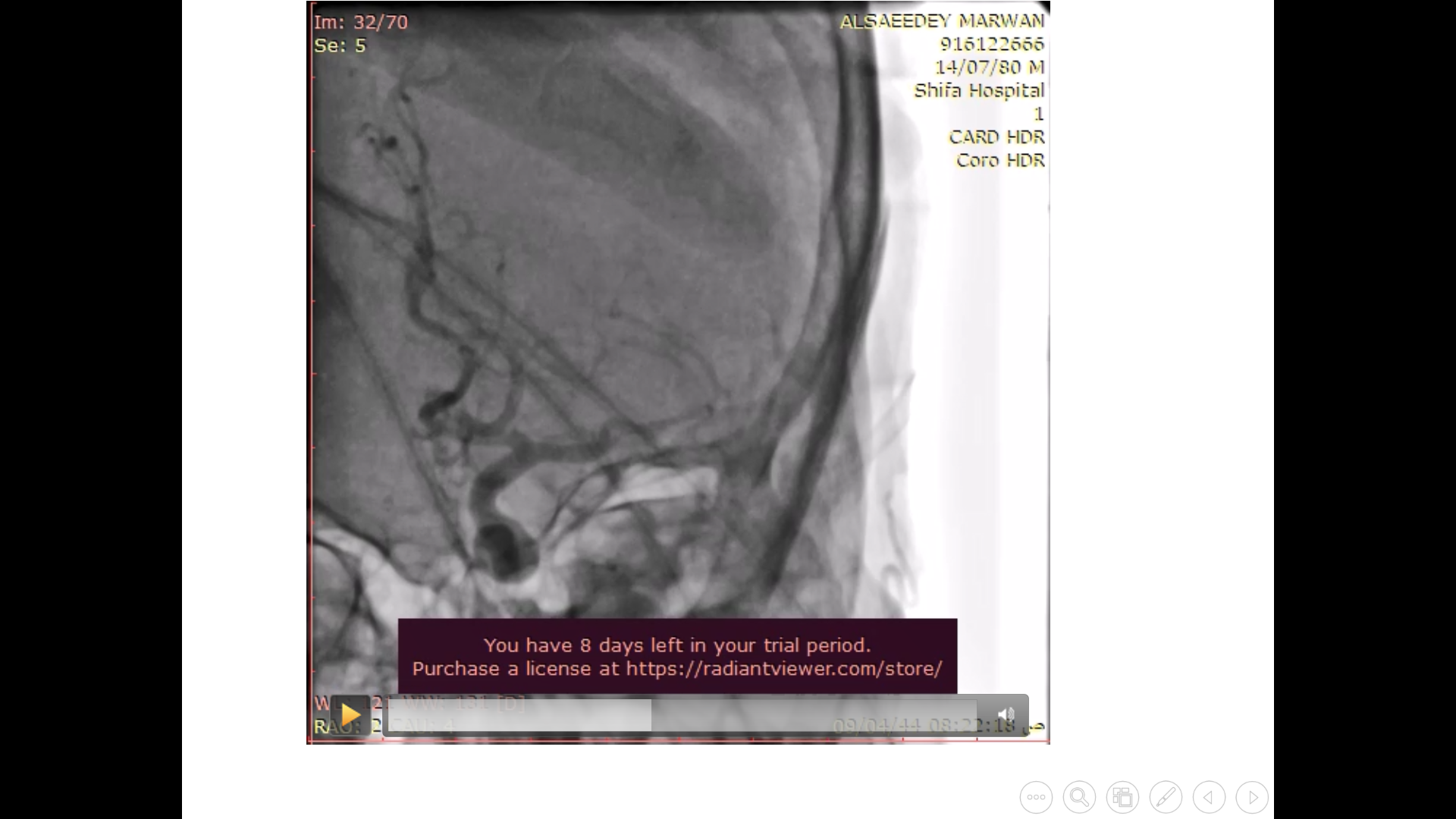
Figure 3a: Baseline cerebral angiography Figure 3b: after thrombus aspiration: left middle cerebral artery occluded middle cerebral artery patent
Then emergency coronary angiography was done and suggested subtotally occluded in proximal left anterior descending artery with TIMI flow 0-1 and involved large diagonal branch with medina classification (1:1:1) 0.014 inch coronary PT2 wire was cross the lesion in mid LAD with placed in distal LAD with free movement in distal LAD another wire was cross the lesion and placed in ostial diagonal branch with free movement. Balloon dilatation was done by using 2x15 mm maverick balloon then 2.5x18 mm resolute stent (drug eluting stent) was deployment in mid LAD with TIMI flow 2-3. Tirofiban 4 mg intracoronary was given to improve intracoronary flow. Figure 4a, 4b

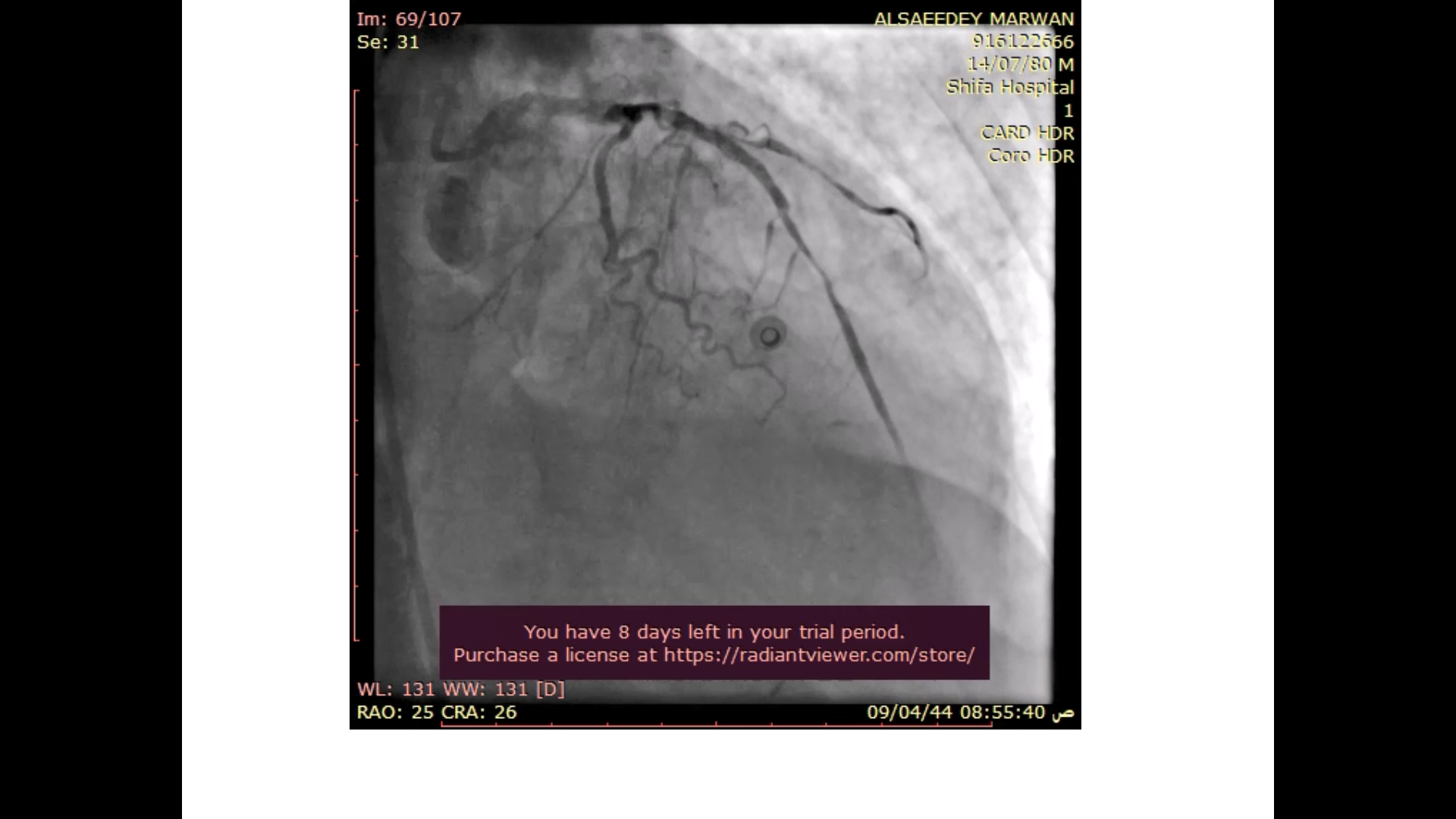
Figure3a: mid LAD subtotally occluded Figure 4b: after angioplasty patent stent in LAD
Involved ostial diagonal branch. With TIMI flow2-3
Subsequent echocardiogram showed LVEF of 35%. Septo-apical hypokinesia and left ventricle 1.2x2.3 mm thrombus. Figure5

Figure 5: left ventricle apical thrombus.
Because of severe agitation and hypotension norepinephrine with 17 mcg/kg/min was started, and continues general sedation with Midazolam continuous was infusion of 0.1 mg/kg/h. and follow up in intensive care unit (ICU).
After 4 days blood pressure stable 100/65 mmHg, heart rate atrial fibrillation was developed during 2nd day in ICU and amiodarone bolus 150 mg over 30 min and continuous infusion was done by 1050 mg (7 ampoule) in 500 cc normal saline over 24 hours (21 cc/hour). After 7th day the patient discharge from hospital with good clinical condition and without and neurological deficit.
Discussion
The new definition of cardiocerebral infarction syndrome was according to
The Al-Shifa Hospital Classification of Cardio-Cerebral Infarction Syndrome divided into 3 types (2)
Type I: concurrent cardio-cerebral infarction syndrome: acute myocardial infarction (< 12 hours) with acute ischemic stroke (<4.5 hours) from last known well
Type 2: Acute ischemic stroke (<4.5 hours) from last known well, after
recent myocardial infarction (myocardial infarction in the previous 3 months but more than 12 hours).
Type 3: Acute myocardial infarction (< 12 hours) after recent ischemic stroke (ischemic stroke in the previous 3 months but more than 4.5 hours
The most rare type is type 1 . In large recent cross sectional trail of single institutional series showing the prevalence rate of synchronous cardiocerebral infarction to be 0.25% with patients presenting as moderate-severe acute ischemic strokes and high-risk acute myocardial infarction. These patients have a high mortality rate with a significant proportion having cardiovascular deaths (3)
The most recent data in 2017 from Yeo et al. showed that 6% of patients with acute stroke had ST segment elevation [4,5]. Notably, these reported incidences are mostly for non-synchronous presentation, rather than simultaneous presentation of AIS and AMI.
Recent metanalysis of cardiocerebral infarction with A total of 44 cases of CCI were identified from 37 case reports and series; 15 patients (34.1%) were treated using percutaneous coronary intervention (PCI) with stent, 8 patients (18.2%) were treated with a PCI without stent, 10 patients (22.7%) were treated via a cerebral vessel thrombectomy and 8 patients (18.2%) were treated via a thrombectomy of a coronary vessel. (6)
Although uncommon, simultaneous cardiocerebral infarction one of the most challenging medical emergency conditions and requires timely management. therapeutic strategies and efficient team-work among neurologists and cardiologists are required for ideal management for such exceptional cases. We believe that invasive treatment using mechanical thrombectomy for cerebral arteries and PCI to culprit coronary artery must be done. Future clinical trial study, though difficult to perform due to its rarity, is required in order to develop the optimal management of this catastrophic clinical scenario.
Ethics Statement
Due to the patient’s condition, written consent was obtained from the patient’s relative for the publication of this manuscript