Neurosurgery and Neurology Research
OPEN ACCESS | Volume 7 - Issue 1 - 2025
ISSN No: 2836-2829 | Journal DOI: 10.61148/2836-2829/NNR
BOUCHENAKI. F1., HABCHI N2., BOUSTIL K1., HAMROUCHE F1, BAKHTI S. 1
1Neurosurgery Department ALI AIT IDIR Hospital Health Establishment, Algiers, Algeria
2Neurosurgery Department, MUSTAPHA PACHA University Hospital, Algiers, Algeria
*Corresponding author: Bouallag Magdouda, Neurosurgery Department ALI AIT IDIR Hospital Health Establishment, Algiers, Algeria.
Received date: September 19, 2022
Accepted date: September 03, 2022
published date: October 19, 2022
Citation: OUCHENAKI. F, HABCHI N, BOUSTIL K, HAMROUCHE F, BAKHTI S, (2022) “A Case Study and Assessment of the Literature Regarding Multiple Cerebral Hydatidosis”. J Neurosurgery and Neurology Research, 4(3). DOI: http;//doi.org/11.2022/1.1045.
Copyright: © 2022 Bouallag Magdouda. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cerebral hydatidosis is relatively rare and has a favorable prognosis after surgical treatment. The multiple forms of cerebral hydatidosis complicate surgical management and change the pathology's good prognosis. We present the case of a 19-year-old young man who presented to the emergency department with generalized convulsive seizures, behavioral disorders, and an intracranial hypertension syndrome. A normal clinical examination was performed, and computed tomography revealed two right frontal hydatid cysts with significant mass effect on median structures. As part of the emergency procedure, he was operated on, and the two cysts were evacuated using hydropulse technique. We noticed a significant clinical improvement. We highlight the rarity and difficulty of surgical management of multiple cerebral hydatidosis in this case.
Introduction:
In the midst of new technologies, microsurgery, and neurosurgical advancement, we still have an infectious pathology that has been eradicated elsewhere: the hydatid cyst.It is an anthropozoonosis caused by Ecchinococcus granulosis, with the dog as the sole host.
The man is affected accidentally (Fig 3). Its cerebral localization is rare and poses real therapeutic problems when it is multiple.
Material and methods:
Without any specific medical or surgical history, the 19-year-old Algerian boy who left for a two-month plumbing internship in Tiaret will be the subject of this case study. He visited the emergency department complaining of an HIC syndrome, behavioral issues, and generalized epileptic seizures that had lasted for ten days.
A frontal syndrome was the only notable aspect of the clinical evaluation.
Two right frontal cysts with a sizable mass effect on the median structures were detected by a cerebral CT scan.(Fig 2, 3 and 4)
The results of the abdominal ultrasound and chest X-ray were unremarkable.
The patient underwent emergency surgery, and hydropulse technique was used to remove the two cysts.
The postoperative course was marked by the regression of the frontal syndrome and the appearance of a CSF fistula treated in the service.The results of the anatomo-pathological investigation supported a hydatid cyst.
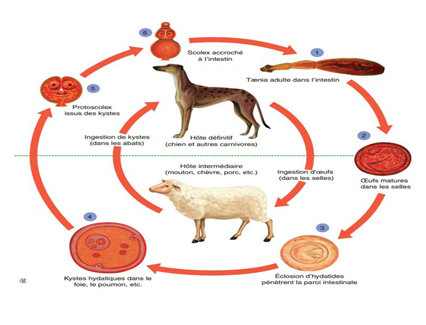
Figure 1: Cycle of the tænia Echinococcus granulosus
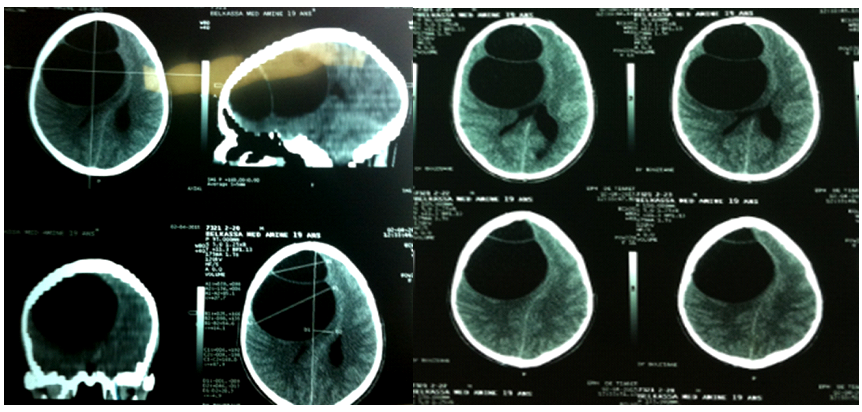
Figure 2: typical hypodense CT image of a frontal double hydatid cyst

Figure 3: Porencephalic cavity D3 post operative Figure 4: Appearance of a non-compressive hygroma D8 post operative
Discussion and a review of the literature:
Even in nations where the disease is endemic, it accounts for 1% to 3.4% of all intracranial processes [1.2.3], although according to GUPTA [4], it can occasionally account for a higher percentage between: 1-10%. With an average age of onset of 15 years, it far more frequently affects children than adults; in the Mediterranean basin, this might range from 7.4 to 8.8% of cases in children [5].
After consuming the larva in humans, the embryophore passes through the intestinal mucosa and enters the portal vein, where it travels to the liver. The pulmonary capillaries normally keep the embryo after it has passed the hepatic filter.
Although the hydatid cyst can affect any organ, the liver and lungs are the most commonly afflicted (15–30%).
The systemic circulation can only carry embryos to the brain if they are able to get past the hepatic and pulmonary filtration systems.Frontal and parietal areas of the brain are the most commonly impacted [6].
In most cases, patients who have been infected have a rural background.Simple headaches to temporal engagement are examples of symptoms that vary depending on the location. The syndrome of intracranial hypertension is the most prevalent presenting type ( table 1).
|
Authors |
Percentage of HTIC (%) |
|
El Saqui et al. [39] |
93 |
|
Bukte et al.[15] |
83,3 |
|
Khaldi et al. [24] |
75 |
|
Ben Becher et al. [45] |
100 |
Table 1: Percentage of Intracranial Hypertension as indicative sign of cerebral hydatid cyst in the literature
The diagnostic means nowadays are represented by brain MRI and CT scans.
Imaging also allows for the measurement of the cyst's size and, consequently, the risk of intraoperative rupture. Computed tomography (CT) of the brain
Appearance: The CT image is often consistent. The cyst is a single, well-circumscribed, large, thin-walled structure with the density of cerebrospinal fluid (CSF) that is spherical or oblong in shape [18].
Without contrast enhancement or perilesional edema, it is directly in the parenchyma.
When they are present, this is a symptom of inadequate sealing connected to the cyst fissuring with the ensuing inflammatory response [8].
The cerebral hydatid cyst would expand by 4.5 cm every six months. Cyst and intraacystic wall calcifications are rare.
- Appearance of hydatid cyst on MRI shows the hydatid cyst as a spherical structure, with fine contours and containing a liquid having the magnetic appearance of CSF, hypo intense in T1 sequence and hyper intense in T2 sequence. [15-18].
Differential diagnostic problems may arise especially in cases of cyst remodeling such as cystic gliomas, arachnoid cysts, other infectious processes; the cyst wall is thick in these cases with or without contrast enhancement.
Other locations may be associated; Hepatic localization is the most common (50 to 70%), followed by pulmonary localization (25 to 40%), but in practice, any organ can be affected, with simultaneous localization to one or more viscera in 25% of cases. approximately [1,12,19]
Processing
Surgery is the first and effective therapeutic option in the cerebral localization of the hydatid cyst, the goal is the complete removal of the cyst without rupture; by forced hydrostatic expulsion, using hypertonic saline solution introduced around and under the cyst (Fig 5).
The hydrodissection technique of Arana-Iniguez and San Julian 1951 [13] is the most widely used method. It consists of mass enucleation of the cerebral hydatid cyst by injecting hypertonic saline under pressure between the cerebral parenchyma and the cyst membrane.
childbirth then takes place without difficulty.
Subsequently, the residual cavity is carefully examined and then filled with hypertonic saline which will be aspirated before the closure of the various planes and the placement of an extradural siphoning drain.
The successful delivery of KHC without rupture requires certain conditions [14,15]:
1. Proper anesthesia is essential to keep the brain relaxed to prevent accidental bursting of the cyst
2. The exact size and location of the cyst should be traced on the surface of the scalp, and the bone flap should be wider than the diameter of the cyst
3. Initially the head should be elevated 30°
4. Drilling must be done manually, slowly and without vibration. The insertion of the GIGLI guide must be done with special care in order to avoid any tearing of the dura.
5. Electrocoagulation should be avoided as much as possible if the dura mater is exposed
6. open the dura mater where the cyst is most superficial
7. great care should be taken when opening the dura because in large cysts the dome often lies just below and is covered by a thin layer of leptomeningeal adhesions
8. To uncover such a dome, the arachnoid adhesions can be separated from the cyst by gentle dissection without coagulation
9. Once the dome of the cyst is bare, the surgeon can decide if the cerebral opening is large enough for safe delivery of the cyst. This opening must represent at least 3/4 of the section of the cyst
10. The cyst will be delivered by tilting the operating table 45° and using gentle irrigation. The cyst then descends under the effect of gravitational force
11. After delivery of the cyst, the residual cavity should be carefully examined and washed with hypertonic serum. Subsequently all the saline and CSF present therein must be aspirated
12. A full examination should be performed to ensure that there are no retained daughter vesicles, and if present ensure that they are not ruptured by aspiration.
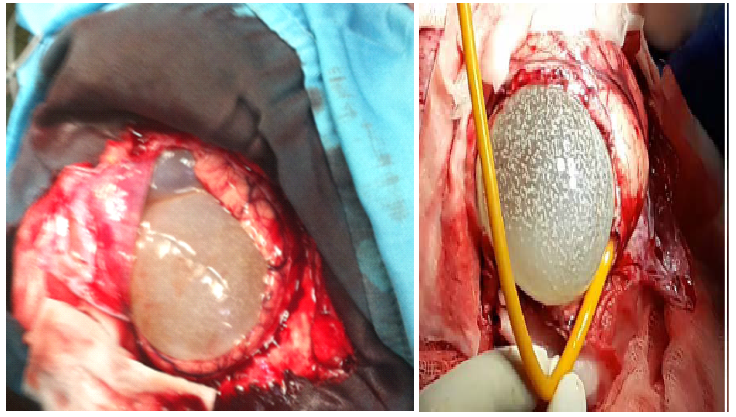
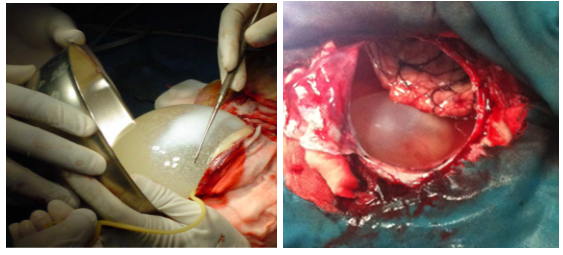

Figure 5: different stages of surgery
- Intraoperative incidents:
Two distinct categories of complications are related: According to numerous studies, the cyst can rupture in 16 to 25% of instances even with diligent treatment [16].
Secondary spreading and anaphylactic shock are potential complications of this rupture [15].
-In the event of rupture, the cyst's contents and capsule must be aspirated very away, and the cavity must be irrigated with liquids that are parasiticidal (1 to 3% hypertonic saline or 0.5% silver nitrate solution) [17].
-Other intraoperative, but non-specific, complications may be encountered such as subdural hematoma, pneumocephalus, intraparenchymal hemorrhage or hydrocephalus.
-The risk of recurrence is about 19%, [14] and it is correlated with the rate of intraoperative rupture of the cyst, then causing seeding by the scolices, and the birth of new vesicles within 6 to 12 months according to Tlili-Graiess et al. [11]
A voluminous hydatid cyst contains 3 to 6 ml of hydatid sand, of which 1 ml contains 400,000 scolex, which explains why a minimal oozing of liquid during the operation can lead to recurrences of the hydatid cyst [14].
-The mortality associated with cerebral hydatid cyst of the CNS is very rare, it is between 0 and 10.12% according to the review of the literature.It may be related to intraoperative rupture of the cyst responsible for a severe anaphylactic reaction with circulatory collapse and death.The sequelae are often of the type of epilepsy, blindness secondary to the syndrome of intracranial hypertension (related to the delay in diagnosis) and motor deficit.
Conclusion:
Cerebral hydatidcyst is a rare condition that affects young adults, often from rural areas, who have had previous contact with dogs. It is most commonly manifested by an intracranial hypertension syndrome with seizures and a focal neurological deficit that is location dependent. The diagnosis is strongly suspected on cerebral CT; however, in the case of a remodeled hydatid cyst, cerebral MRI is especially useful in making the differential diagnosis with other intracranial cystic processes. Serology for hydatidose is only suggestive. Surgery is the first line of defense. Apart from multiple cerebral localizations, which pose a serious therapeutic problem, the prognosis is generally good in the event of early diagnosis.