Neurosurgery and Neurology Research
OPEN ACCESS | Volume 7 - Issue 1 - 2025
ISSN No: 2836-2829 | Journal DOI: 10.61148/2836-2829/NNR
Traore MM1, Diallo M2-3, Barrey C3, Kakou M4, Ndri Oka D4, Boni Nr4, Bazez V4
1Department of Radiology Hospital of Mali
2Faculty of Medicine and Odontostomatology Bamako
3Department of Neurosurgery Unit 100, Pierre Wertheimer Hospital Lyon
4Neurosurgery Department CHU Yopougon Abidjan
*Corresponding authors: DIALO Moussa, Faculty of Medicine and Odontostomatology of Bamako (Mali) University of Sciences, Techniques and Technologies of Bamako BP 1204, Mali
Received date : November 09, 2021
Accepted date : November 15, 2021
published date : November 18, 2021
Citation: Traore Mm, Diallo M, Barrey C, Kakou M, Ndri Oka D. “Simultaneous Ischemic and Hemorrhagic Stroke in The Same Brain: A Case Report”. J Neurosurgery and Neurology Research, 2(5); DOI: http;//doi.org/011.2021/1.1030.
Copyright: © 2021 DIALO Moussa. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
Chronic low back pain is the 3rd leading cause of disability claims. Surgical intersomatic fusion of degenerative levels is an effective treatment on low back pain. The purpose of this work was to compare the therapeutic result of two arthrodesis techniques: posterolateal arthrodesis (PLIF) and combined arthrodesis (ALIF associated with posterolateal arthrodesis by screws) at the L5-S1 level.
Materials and Method
This was a descriptive study carried out in the Neurosurgery C department of the Pierre Wertheimer Hospital in Lyon between January 2010 and May 2012. It concerned patients surgically treated with L5-S1 mono-segmental disc disease. Epidemiological, radiological, surgical and evolutionary parameters were studied. Our data has been processed by the STUDENT test. A p-value < 0.05 is considered statistically significant in data analysis. Two groups of 17 patients each treated for L5-S1 mono-segmental disc disease were compared. Group I consisted of patients treated with PLIF. Group II consisted of people treated first Combined.
Results
A female predominance with a sex ratio of 0.8 had been found. The mean age was 42.3 ± 8.6 years for group I patients and 44.3 ± 10.3 years for group II patients, p=0.27. The pain assessment (VAS) prior to surgery was 4.15 ± 2.3 for group I patients and 4.75 ± 2.9 for group II patients (p=0.23). The average operating time was 121 ± 43.1 min for PLIF compared to 147.7 ±49.5 min for combined first surgery (p=0.05). Operative complications consisted of injury to the left external iliac artery one case (5.8%) in group II versus one case of dural breach (5.8%) and 3 cases of postoperative neurological deficit (17.6%) in group I. The 4-month post-surgical EVA was 1.14 ±1.55 for group I and 1.14 ± 1.62 for group II (P=0.49). At 1 year, lalombalgia was found in 52.9% of patients in group I compared to 41.1% of those in group II (p=0.04).
Conclusion
The first combined in one time in the treatment of disc disease an interesting surgical technique that can be improved by replacing the later time with minimally invasive surgery.
Introduction
Chronic low back pain is the 2nd cause of consultation with the doctor and the 3rd cause of disability application [1]. Surgical intersomatic fusion of degenerative levels is an effective treatment option for stabilizing the painful segment [2]. This surgery for its success will have to take into account the sagittal balance of the spine. This work on the surgical management of L5-S1 mono-segmental disc disease aimed to compare the therapeutic result of two arthrodesis techniques: posterolateal arthrodesis (PLIF) and arthrodesis by combined approach (ALIF associated with posterolateal arthrodesis by screws) at the level of the lumbosacral hinge affected by disc disease. The goal was to find the most effective and least harmful technique for patients: the most suitable technique for the treatment of L5S1 mono-segmental disc disease.
Material and Method:
This is a cross-sectional descriptive study carried out in the Neurosurgery Unit -C department of the Pierre Wertheimer Hospital in Lyon between January 2010 and May 2012. It concerned patients surgically treated with L5-S1 mono-segmental disc disease. On the exploitation of medical records, the following parameters were studied: age, sex, therapeutic time (time between the first clinical signs and surgical treatment), operative therapeutic choice (between Postero-lateral Interbady Fusion PLIF and first combined), blood loss, operative time, quality of life parameters (EVA, OSWESTRY), time to return to work and impact on sagittal balance. Our data was uploaded to Excel and processed by student's statistical test. A p-value < 0.05 is considered statistically significant in data analysis.
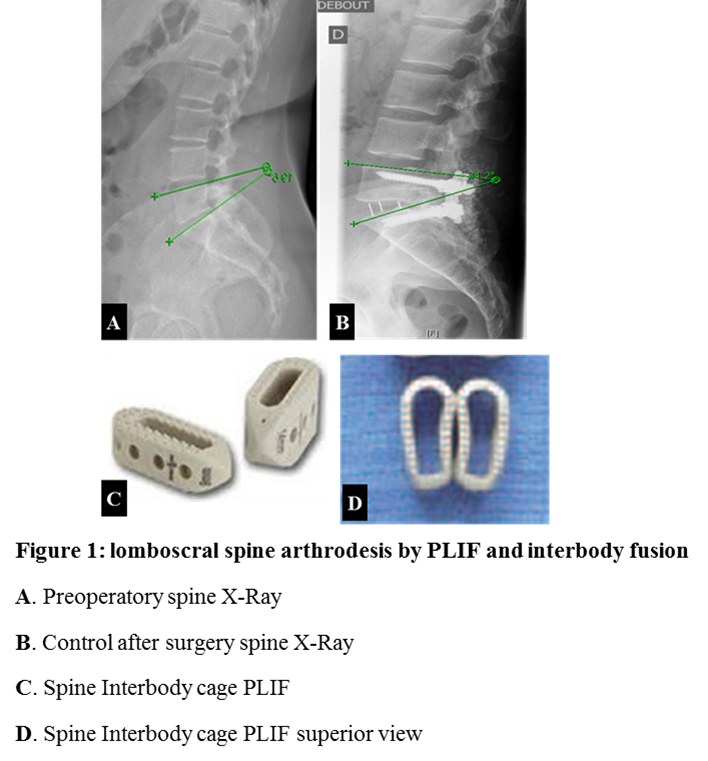
The work that consisted in comparing two groups of 17 patients each treated for L5-S1 mono segmental disc disease had made it possible to collect 34 patient records between January 2010 and May 2012 (17 months). The first group (group I) consisted of patients treated with the posterolar lateral fixation technique by screws associated with the establishment of a pair of interdody cage in L5-S1 (PLIF) Figure 1.
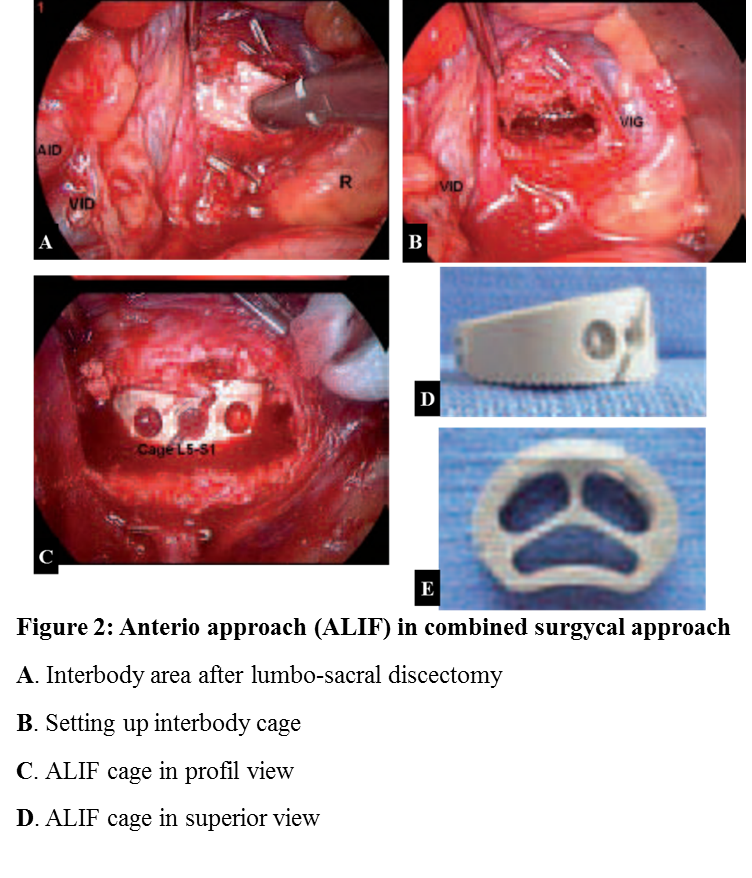
The second batch consisted of people treated at the same time operatively with an ALIF (anterior retro-peritoneal and pre-vertebral approach of the spine for the establishment of an L5-S1 cage by way Anterior Figure 2) associated with a posterolateral fixation by 2 pairs of pedicle screws: Combined approach (group II).
Inclusion criteria were patients who received surgery by PLIF or first combined between January 2010 and May 2012 for lumbosacral mono segmental disc disease (L5-S1); Consenting patients who have been regularly monitored for at least one year after surgery; actionable patient records. Patients treated for multi-stage disc disease were not included in this work; patients treated with mono-segmental disc disease with osteosynthesis beyond L5-S1; Patients who did not have regular follow-up during the 1st year after their surgery.
A total of 34 files were retained. Our work had some limitations which are: the lack of assessment of the quality of the fusion, the blood contained in the Jars of Redon was not taken into account in the losses, the sample size was not very large.
Results
Our female-dominated study population sex ratio with a 0.8 (16 men/18 women) had an average age of patients was 43.3 ± 11 years. It was 42.3 ± 8.6 years for patients operated on PLIF-type arthrodesis (group I) and 44.3 ± 10.3 years for those treated by combined first (group II) with a p=0.27 >0.05. Among group I patients, and 44.3 ± 10.3 years for those treated by combined approach (group II) with a p=0.27 >0.05. Among group I patients, the age group of 30-36 years was the largest with 35.29% compared to 17.6% for those in group II where the majority of patients had an age between 37-42 years. Patients in both groups came from all walks of life. Disabling single or bilateral lumbar and radicular pain dominated the clinical picture in patients, one-third of whom had been off work for at least 3 months. The pain assessment (VAS) prior to surgery was 4.15 ± 2.3 for patients in group I and 4.75 ± 2.9 for those in group II (p=0.23 > 0.05: NS). (Table I).
|
EVA/10 |
0 |
1 |
2 |
3 |
4 |
5 |
6 |
7 |
8 |
9 |
10 |
||
|
Technique |
PLIF |
actual |
- |
- |
2 |
1 |
4 |
2 |
5 |
2 |
1 |
- |
- |
|
% |
0 |
0 |
11,7 |
5,8 |
23,5 |
11,7 |
29,4 |
11,7 |
5,8 |
0 |
0 |
||
|
Combined |
actual |
- |
- |
- |
2 |
2 |
3 |
1 |
4 |
5 |
- |
- |
|
|
% |
0 |
0 |
0 |
11,7 |
11,7 |
17,6 |
5,8 |
23,5 |
29,4 |
0 |
0 |
||
patients in group II had EVA greater than 5 compared to 47% of those in group I.
Table 1: Preoperative assessment of lumbo-radicular pain by the visual analogue scale (VAS) in both groups.
The mean therapeutic time (the time between first clinical signs and surgery) was 15.8 ± 28.4 months for group I patients versus 16.7 ± 13.9 months for group II (p= 0.45 > 0.05: NS). Seventy-three comma fifty-three percent of our patients suffered from degenerative isolated disc disease (25 patients). Three patients in group II had postoperative disc disease of a lumbosacral disc herniation. Disc disease was associated with Grade I spondylolisthesis in 26.47% in our study population. A lumbosacral angiography-CT scan had been performed preoperatively for patients of group II as well as radiological of the total spine: EOS or "FULL SPINE". The average operating time was estimated at 121 ± 43.1 min for PLIF versus 147.7 ±49.5 min for combined first surgery (p=0.05). Blood loss averaged 270 ± 206 ml in group I patients (PLIF) and 258.19 ± 182.55 ml in group II (first combined) (p=0.43 > 0.05: NS). PEEK (poly-ether-ether-ketone) cages were used in both cases, filled with INDUCTOS® (bone substitute) for the anterior implanted cage (group II) and autograft for group I cage in which a pair of cages was used against a single cage in group II. Table II presents the different interbody cages used in the 2 groups with their size and degrees of lordosis.
|
Characteristic cages |
|
12° 13mm 24mm |
10° 13mm 25mm |
10° 11mm 25mm |
10° 10mm 25mm |
10° 8mm 25mm |
10° 4mm 25mm |
5° 13mm 25mm |
5° 12mm 25mm |
4° 12mm 25mm |
4° 10mm 25mm |
|||||||||
|
PLIF (Groupe I) |
|
actual |
|
1 |
1 |
1 |
7 |
1 |
1 |
1 |
1 |
1 |
2 |
|||||||
|
% |
5,8 |
5,8 |
5,8 |
41,1 |
5,8 |
5,8 |
5,8 |
5,8 |
5,8 |
11,7 |
||||||||||
|
Cage features |
17° 13mm 25mm |
13° 15mm 25mm |
13° 13mm 25mm |
12° 12mm 25mm |
9° 11mm 25mm |
|
||||||||||||||
|
Combined (Group II) |
actual |
1 |
6 |
5 |
3 |
2 |
|
|||||||||||||
|
|
|
|
|
|
|
|
||||||||||||||
|
|
% |
5,8 |
35,2 |
29,4 |
17,6 |
11,7 |
|
|||||||||||||
The previous approach (group II) allowed the establishment of cages with a high degree of lordosis and a better opening of the interbody space than surgery by PLIF (group I)
Table 2: Distribution of patients by surgical technique and type of interbody cages used.
All patients had been lifted the day after surgery (J1) except one in group I who had an intraoperative dural breach. The average length of hospital stay was 6.5 ± 2 days for group I patients versus 8.1 ± 4 days for group II patients (p=0.07). Three patients (17.6%) from group I and one (5.8%) from group II had been admitted to rehabilitation centre for postoperative neurological deficit (group I) and persistence of preoperative neurological deficit (group II). A group I patient (5.8%) transferred to a convalescent home for the persistence of low back pain. Surgical complications consisted of injury to the left external iliac artery one case (5.8%) in group II versus one case of dural breach (5.8%) in group I. Three patients in group I (17.6%) had a post-surgical neurological deficit and one patient was taken back to the operating room for staphylococcal Aureus infection of operative scar 20 days after surgery. The assessment (EVA) of root pain 4 months after surgery was 1.14 ±1.55 for group I and 1.14 ± 1.62 for group II (P=0.49 > 0.05: NS). At 6 months of evolution, 62% of patients in group II had already returned to work compared to 50% of patients in group I. At 1 year, the average return to work was estimated at 7.5 ± 3.5 for group II patients compared to 6.5 ± 2.12 for group I patients (p=0.38> 0.05: NS). Lombalgia with a type of "bar" in the back was found in 52.9% of patients in group I compared to 41.1% of those in group II (p= 0.04). This symptom required professional redeployment or reorganization of working time in 17.6% (3 cases) of patients in group I compared to 11.8% (2 cases) of those in group II. In Group I, the mean segmental lordosis was 42.75 ± 5.6° preoperative and 45.92 ± 4.7° postoperative (p=0.01). For group II, it was 38.93 ± 6.3° before surgery and 43.98 ± 5.7° after surgery (p= 0.04). On the other hand, the angle of local lordosis was 17.16 ± 5.4 ° preoperative and 24.01 ± 3.9 ° postoperative (p >0.05) for group I. This was 16.67 ± 3.9° preoperatively and 28.3 ± 3.9° (p >0.05) for Group II. Fifty-eight percent of group I patients had been significantly improved. The OSWESTRY score (ODI) before and after surgery in group II patients is recorded in Table III.
|
Score OSWESTRY |
0-20 |
21-40 |
41-60 |
61-80 |
81-100 |
|
|
Before surgery |
actual |
3 |
3 |
5 |
4 |
2 |
|
% |
17,6 |
17,6 |
29,4 |
23,5 |
11,7 |
|
|
After surgery (1 year) |
actual |
10 |
5 |
1 |
1 |
0 |
|
% |
58,8 |
29,4 |
5,8 |
5,8 |
0 |
|
After one year 58.8% of patients had been significantly improved their quality of life.
Table 3: Distribution of group II patients by OSWESTRY score (ODI) before surgery and one year of postoperative course.
Discussion
The annual incidence of low back pain in France is estimated to be between 5% and 10%. According to a survey by the health research, study and documentation center (CREDES), the frequency of low back pain tripled between 1982 and 1992 in France. Less than 10% of patients will progress to chronicity and will represent 70% to 80% of the costs related to the condition [3]. The female predominance of lumbar disc disease found during our study was reported in the literature [4]. Some authors report a high frequency in physical workers [5]. Modic1 disc disease responds very favourably to arthrodesis [6]. Although statistically insignificant, the treatment time was somewhat longer in group II patients. This is related to the selection of patients and the performance of examinations to plan surgery in order to reduce the risk of surgery. These examinations include a lumbosacral spinal computed tomography (CT) to evoke the diagnosis, magnetic resonance imaging (MRI) of the lumbosacral spine for the classification of MODIC, an X-ray of the whole spine "Full Spine" to assess the sagittal balance and an Angiography-CT-Scan of the iliac vessels to assess the path of the artery and iliac veins in relation to the spine and the L5-S1 disc. Several elements make it possible to evaluate the effectiveness of the surgery. The two main ones are the maintenance and or correction of the sagittal balance of the spine and the quality of spinal fusion. A good arthrodesis must be able to obtain a good spinal static with an adequate vertebral fusion to suppress inflammation of the vertebral plateaus. Obtaining a better degree of lordosis by ALIF during the combined first found during our study has been reported by some authors [2]. This arthrodesis technique (ALIF) allows a direct median view of the disc space, a good discectomy and better preparation of the trays. These have the advantage of maximizing the size and surface area of the implant and therefore obtaining a high degree of lordosis and the contact surface to increase the fusion rate [7; 8; 9; 10]. Fusion can reach 88.6% in ALIF surgery [8]. This rate of consolidation may be even higher with the use of autograft [11]. All of our Group II patients received an allogeneic bone substitute transplant and those in Group I an autologous transplant. This was a matter of choice related to the surgeon's appreciation. ALIF arthrodesis spares the posterior spinal muscles and anteterolateral psoas, which can reduce postoperative pain and disability [8]. When first combined this preservation of lumbar musculature is not fully respected. In our patients, the posterior time was done by open focus surgery. Chen et al to minimize the decay of the posterior spinal muscles and reduce the risk of infection had opted for percutaneous surgery for the installation of pedicle screws [12]. The posterior approach by pliF provides excellent visualization of nerve roots, decompression of nerve roots, and adequate restoration of intersomatic height while maintaining posterior support structures [13]. As a result, PLIF is of great interest in the treatment of disc disease associated with spondylolisthesis with associated isthmic lysis due to the high risk of L5 nerve damage [14]. In this case a root decompression associated with spinal relordosis and arthrodesis may have a net benefit on the symptoms. The posterior channel (PLIF) allows an adequate and rigid stabilization of the column [15]. Studies have shown that there are no significant differences between PLIF and combined approach compared to sagittal balance parameters between the two techniques [16]. This result is the opposite of ours where we found that the combined approach allowed to obtain a higher degree of lordosis than PLIF surgery. Results from a prospective trial observed an improvement in EVA and ODI in 86% of patients treated with PLIF with a 98% fusion rate at 2 years. The authors concluded that PLIF with a cage was a safe and effective surgical treatment for low back pain caused by degenerative disc disease [17]. Other authors in 2013 came to the same conclusion for the combined approach [18]. But, the effectiveness of this surgery does not say to hide its sometimes formidable complications even if they are rare. It is a sexual disorder manifested in men by retrograde ejaculation and in women by vaginal dryness, peritoneal breach and vascular injury [9; 19]. One case of the latter was recorded during our study. Significant paraspinal iatrogenic lesions associated with prolonged muscle retraction described by some authors [20] can be seen in both surgical techniques. They can delay recovery and mobilization due to approach-related muscle trauma. Nerve root retraction and chronic radiculopathy caused by fibrosis may be seen after PLIF surgery [21; 22]. The combined approach can gain in efficiency by replacing the open focus surgery "open surgery" of the posterior approach by the percutaneous surgery (MIS: "Minimaly invasive surgery") for the installation of pedicle screws like.
Conclusion
The one-step combination approach (ALIF + posterolateral arthrodesis) in the treatment of L5-S1 mono-segmental disc diseases seems to be an interesting alternative to conventional posterior surgery (PLIF). It allows to have both the advantages of the anterior surgery and those of the posterior approach. To increase its effectiveness, the open-focus surgery of the posterior time must be replaced by a percutaneous approach in "Minimaly Invasive Surgery (MIS).