Neurosurgery and Neurology Research
OPEN ACCESS | Volume 7 - Issue 1 - 2025
ISSN No: 2836-2829 | Journal DOI: 10.61148/2836-2829/NNR
Suhasish Ray 1*, D.K. Jha 2
1 (M.B.B.S.; M.Ch;M.Sc; Doctorate on Ortho spinal surgery) Fellow Spine Surgery- SRS,IOA,WBOA,WESS,Innsbruck University Director=spineservices india
Spine Surgeon- Woodland Multispeciality Hospital. 10 Alipore Road, Kolkata, India
Ramakrishna Mission Seva Pratisthan and Vivekananda Institute of Medical Sciences, Sishumangal Hospital. Kolkata, India.
2 (M.S, -0rtho)- Professor and Head, Department of Orthopaedic and spine surgery, Ramakrishna Mission seva Pratisthan and Vivekananda Institute of Medical Sciences, Sishumangal Hospital, Kolkata, India.
*Correspondence author: Suhasish Ray, (M.B.B.S.; M.Ch;M.Sc; Doctorate on Ortho spinal surgery) Fellow Spine Surgery- SRS,IOA,WBOA,WESS,Innsbruck University Director=spineservices india.
Received date: July 12, 2021
Accepted date: July 16, 2021
published date: July 20, 2021
Citation: Ray S, D.K. Jha. “Muscle Fat Fascia Graft in Pedicle Screw Malposition- a New Technique to Prevent Post Operative Neurodeficit”. J Neurosurgery and Neurology Research, 2(4); DOI: http;//doi.org/06.2021/1.1022.
Copyright: © 2021 Suhasish Ray. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction:
Pedicle screws are important in stabilizing the vertebrae. Incidence of neurologic injury secondary to a malpositioned screw is 7-12%. [1]. 4% patients undergo revision surgery. The pedicle is separated from the dura by a variable thickness of epidural fat.(Avg.2mm). There has been no study to show whether trilayer autologous graft can act as a buffer in Pedicle breach. Trilayer patch of muscle-fat-fascia can be interposed between dura/ root at risk and pedicle screw malposition to prevent subsequent neurological injury or screw revision.
Materials and Methods:
The aim of study was to see the effect of trilayer fat-muscle-fascia graft interposed between an unrevised malpositioned Pedicle Screw and the immediate adjoining dura/root at risk both as short- and long-term barrier against dural /root breach with its subsequent complications.
The study was conducted after appropriate approval and consent. Between January 2011 – August 2015, 118 patients (68 males/50 females, mean age 60 years, range 27-87 years) were enrolled after informed and explicit consent. We only included pedicle screw encroachment in the vertebrae canal with medially/superior/inferior perforation of pedicle wall. 572 Pedicle screws were inserted by direct visualisation and palpation in the Lumbar spine. Screws were stimulated with cutting monopolar diathermy. Visible twitching of local paraspinal muscles and/ or of lower limb muscles was termed “positive response”, suggestive of pedicle breach. Screws with a positive response on diathermy stimulation but without evidence of dural or neural injury were left in situ . A trilayer closed/open book graft spanning the entire breach area was interposed between the breach and duraCT images were evaluated by an independent radiologist blinded to the intervention.
Results:
3 peroperative and 5 post operative dural leaks were revised.1 patient did not turn up. 109 patients remaining were followed up for 2 years. Criteria for follow up were clinical and CT scan.11 out of 51 grafted screws were revised. Number of revised screws and no. of trilayer grafts preventing complications were compared using Chi-square test, paired t-test and z-test. We defined statistically significant as p<0.0005.
Conclusion:
In our series trilayer graft was found to have an effective barrier in 62 pedicle screw malpositions without any long term dural and/or neurological injury between an unrevised malpositioned screw and the dura at risk.It is a simple, cost effective and patient friendly technique. Performing a thorough search, no similar technique was found to have been done elsewhere.
Introduction:
Pedicle screws have been effectively used to enhance spine arthrodesis. A significant advantage in using transpedicular screws is the rigidity that securely fixes the vertebral motion segments. Compared with cervical and thoracic spine, lumbar or lumbosacral spine can provide a safer margin for screw insertion due to morphometric and anatomical characteristics (1-3). Since its first introduction by Harrington and Tullos in 1969(4) and further development by Roy-Camille et al.,(5), Louis,(6) fixation device for disorders of the lumbar and thoracolumbar spine.In the late 1980s, it has become the mainstay of spinal instrumentation. Despite technical advances over the last few decades, pedicle screw insertion is still associated with complications. Among them, the most commonly reported complication is screw malpositioning, with an overall incidence of 0%–42% in the literature.(7,8). Fortunately, more serious screw-related complications, such as neurological, visceral, or vascular, are very rare. (9) However, the rate of screw misplacement, especially in the lumbosacral canal, is more than 8.7%.(10). Screw malpositioning may result in serious complications, including vascular and neurological deficits (radicular pain, motor and sensory dysfunction), dural tear, epidural haematoma, and pedicle fracture due to instruments loosening and pulling out.(11,12,13). The risk of neurological injury caused by cortical perforation is induced by the pedicle’s proximity to the neural elements. The pedicle cortex is separated medially from the dural sac by a thin layer (2 mm in thickness) of epidural fat.(14) Nerve root irritation may be a very common phenomenon for medially misplaced screws. A study of 131 misplaced screws in 30 patients showed that the incidence rates of cortical penetration and medial wall penetration were 40% and 29%, respectively. Moreover, the deviation on 6 mm CT scans indicated a high risk of nerve root injury. (5). In another study, (3) researchers attempted to define the anatomical relationships quantitatively between the lumbar pedicle and the dural sac medially, and the lumbar pedicle and the nerve roots superiorly/inferiorly. The results demonstrated that from L1 to L5 levels, average pedicle-dural sac distance (PDSD) and pedicle–superior nerve root distance (PSRD) increased significantly from 1.29 mm to 1.56 mm and from 4.12 mm to 5.25 mm, respectively, while the mean pedicle–inferior nerve root distance (PIRD) was 1.1 mm at the L1 level and 1.06 mm at the L5 level.(3)In agreement with Mayfield,(15) as fat can be used effectively in sealing CSF leaks it can also act as a buffer between malpositioned pedicle screw and dura/nerve root immediate at risk.3 grades of Pedicle Screw Malposition (PSM). Grade 0: ideal screw position in the centre of the pedicle without any breach in any cortex. Grade 1: acceptable screw position with cortex breach of <2mm. Grade 2: cortical bone injury with penetration >2 mm, and grade 3: cortical bone injury with penetration into the theca (16). Though it is prudent to revise a malpositioned screw else complications arise, it is not reported how to deal with a malposition screw remaining in situ with dura/ root at risk. We've searched all available sources to find out any reports which deal with the above topic, the result was null.
Aims and objectives of the study:
Our aim is to study the effect of fat-muscle-fascia trilayer graft interposed between an unrevised Pedicle Screw Malposition and the immediate adjoining dura/root at risk. The study is a prospective case control study to see whether the graft acts as an effective long term barrier against dural leak or root/cord injuries.
Materials and Methods:
A retrospective cohort study hence ethical board approval was not required. Between January 2011 – August 2015, 118 patients (68 males/50 females, mean age 60 years, range 27-87 years) were enrolled after informed and explicit consent. We only included pedicle screw encroachment in the vertebrae canal with medially/superior/inferior perforation of pedicle wall Grades 1 and 2 PSM. 572 Pedicle screws were inserted by direct visualisation and palpation in the Lumbar spine under fluoroscope control. Pedicle screws were stimulated with 3W, 6W and 7.5W cutting monopolar diathermy stimulation for one second. Visible twitching of local paraspinal muscles and/ or of lower limb muscles was termed “positive response”, suggestive of pedicle breach. Screws with a positive response on diathermy stimulation but without evidence of dural or neural injury were left in situ . A trilayer closed/open book graft spanning the entire breach area was interposed between the breach and dura and left in situ. Rest of procedure followed as per schedule. Prior to closure, Valsalva manoeuvre performed by anasthaetist to detect any dural breach. Watertight wound closure was done. Non-suction dependant drain was applied. Postoperative CT scan was a routine for all patients. CT images were evaluated by an independent radiologist blinded to the intervention.
Statistical Analysis:
Number of revised screws and no. of trilayer grafts incorporated preventing complications were compared using Chi-square test, paired t-test and z-test. Statistical software used SPSS(SPSS IBM Inc. Ver22.0) We defined statistically significant as p< 0.0005.
Results:
3 peroperative and 5 post operative dural leaks were revised.1 patient did not turn up beyond 3 months (assumed complication).109 patients remaining were followed up for 2 years. Criteria for follow up were clinical (back pain-VAS 7/10 or more, unexpected rise of body temperature, severe or recurrent headache postural or otherwise, fluctuation or pseudomeningocele formation, CSF fistula, motor and sensory changes) CT scan(CSF cyst/fistula or meningocele).11 out of 51 grafted screws were revised.
Conclusion:
In our series trilayer graft was found to have an effective barrier in 62 pedicle screw malpositions without any long term dural and/or neurological injury between an unrevised malpositioned screw and the dura at risk.It is a simple, cost effective and patient friendly technique . Performing a thorough search, no similar technique was found to have been done elsewhere.
Figures And Tables
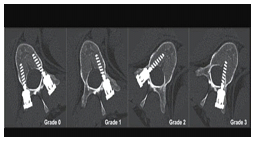
Figure 1: Glasgow grading of Pedicle screw malposition (PSM) 4GRADES OF PEDICLE
SCREW MALPOSITION (PSM). 4 GRADES 0=IN PEDICLE
1= BREACH <2MM OF MED. WALL
2= BREACH >2MM BUT NOT IN CORD
3= BREACH OF MED WALL, SCREW IN CORD
4= TRANSECTION OF CORD.

Figure 2: Illustrative technique of harvesting a trilayer graft

Figure 3: Materials which can be used as grafts/flaps.

Figure 4: harvested trilayer graft
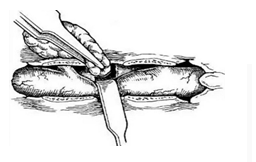
Figure 5: pencil drawing of technique to harvest trilayer graft

Figure 6: Method of accurate placement of trilayer graft.
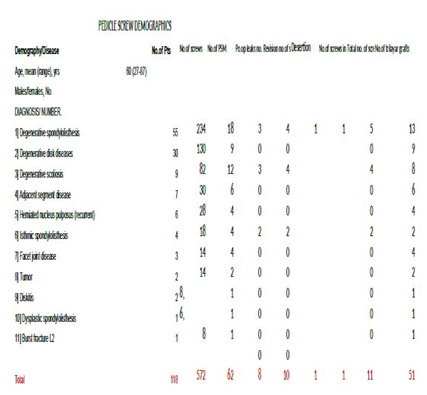
Table 1: Patient Demography
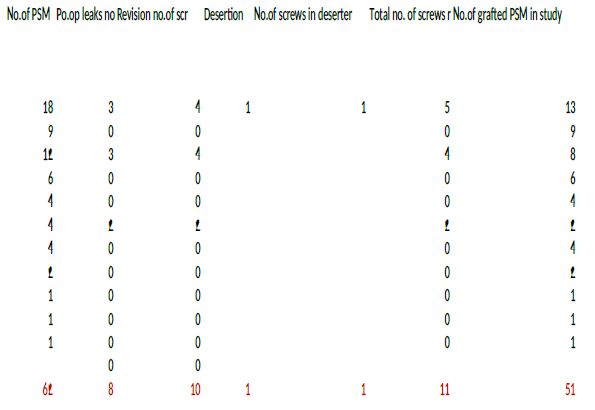
Table 2: Management Demography.
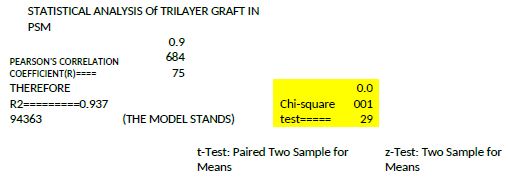
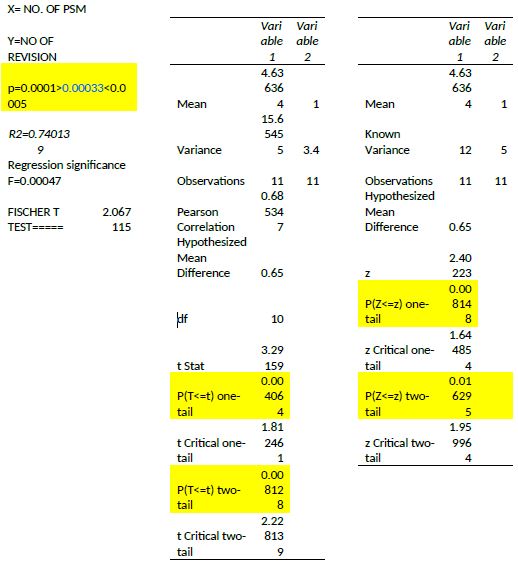
Table3: Statistical Results
Cases for Discussion:
Case-1
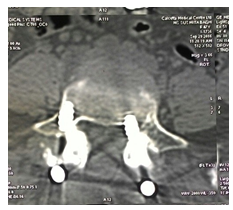
Figure 7: A 47 YR FEMALE GR 2 PSM - 1 year post-operative CT scan showing Grade 2 PSM with trilayer graft without complications
Case-2

Figure 8: Grade 2 pedicle breach with trilayer graft. In a 59yrs female 16 months post operative grade 2 PSM without complications
Case-3

Figure 9: Axial cut demonstrating 47 yrs female grade 2 PSM since 08/2014 with trilayer graft without complications.
Conflict of interest: None Whatsoever.
Etical Board Review: Since this is a retrospective study, ethical board approval was not required.