
Savita Rani Singhal 1, Bhupali Das 2*, Anjali Gupta 3
1 Department of Obstetrics and Gynecology, Pt. B.D. Sharma Post Graduate Institute of Medical Science, Rohtak, Haryana, India, 124001.
2 Department of Obstetrics and Gynecology, Pt. B.D. Sharma Post Graduate Institute of Medical Science, Rohtak, Haryana, India, 124001.
3 Department of Obstetrics and Gynecology, Pt. B.D. Sharma Post Graduate Institute of Medical Science, Rohtak, Haryana, India, 124001.
*Corresponding Author: Bhupali Das, C-7, St. Stephen’s Hospital staff Quarters 4- Rajpur Road, Tis Hazari New Delhi, Delhi India; Email: dasbhupali999@gmail.com
Savita Rani Singhal 1, Bhupali Das 2*, Anjali Gupta 3
1 Department of Obstetrics and Gynecology, Pt. B.D. Sharma Post Graduate Institute of Medical Science, Rohtak, Haryana, India, 124001.
2 Department of Obstetrics and Gynecology, Pt. B.D. Sharma Post Graduate Institute of Medical Science, Rohtak, Haryana, India, 124001.
3 Department of Obstetrics and Gynecology, Pt. B.D. Sharma Post Graduate Institute of Medical Science, Rohtak, Haryana, India, 124001.
*Corresponding Author: Bhupali Das, C-7, St. Stephen’s Hospital staff Quarters 4- Rajpur Road, Tis Hazari New Delhi, Delhi India; Email: dasbhupali999@gmail.com
Received date: Janaury 04, 2021; Accepted date: Janaury 08, 2021; Published date: Janaury 12, 2021
Citation: Das B., (2021) Leiomyoma In Mullerian Remnant Of Mayer Rokitansky Kauster Hauser (Mrkh) Syndrome - A Case Report. Womens Health Care and Analysis, 1(1); DOI: http;//doi.org/03.2020/1.1001
Copyright: © 2021 Bhupali Das, This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background: MRKH syndrome is characterised by varying degrees of uterovaginal atresia in phenotypically normal females with 46XX karyotype with reported incidence of one in 4000 -10000 female births. Occurrence of leiomyoma in mullerian remnant is extremely rare with very few reported cases. Here we are reporting a patient of MRKH syndrome with leiomyoma originating from the uterine remnant.
Case report: A 22 year old, married, primary amenorrhic female presented in OPD with complaints of cyclical pain in lower abdomen for 1 year. Detailed work- up showed features suggestive of MRKH syndrome with a fibroid adherent to left rudimentary horn with left sided haematosalpinx. Patient was taken up for laparotomy where removal of leiomyoma with bilateral rudimentary horn with left sided salpingectomy was done. Histoplathology revealed features of leiomyoma with a rudimentary mullerian lining and haematosalpinx of left tube. The couple was also counselled pertaining to infertility and option for surrogacy was given and same was successful.
Conclusion: In very rare cases, fibroids can originate from fibromuscular tissue of remnant uterus in patients of MRKH syndrome. Excision of tumours with uterine remnants is indicated when symptomatic.
MRKH Syndrome; Leiomyoma; Mullerian anomaly
Introduction
Background
MRKH syndrome is characterised by varying degrees of uterovaginal atresia in phenotypically normal females with 46XX karyotype with reported incidence of one in 4000 -10000 female births.[1] Occurrence of leiomyoma in mullerian remnant is extremely rare with very few reported cases . Here we are reporting a patient of MRKH syndrome with leiomyoma originating from the uterine remnant.
Case Report
A 22 years old, married female with primary amenorrhea presented with complaints of cyclical pain in the lower abdomen, progressively increasing since last one year. She has never been evaluated for primary amenorrhea before. Physical examination revealed normal stature with well developed secondary sexual characters without any gross deformity. Per abdomen examination was within normal limits. External genitalia was normal. Per speculum examination showed blind vagina with no cervix. On bimanual examination, vaginal length was approximately 5 cm (may be achieved through sexual activity). A mobile, nontender, well defined and firm mass approx. 8×8 cm size was also felt in left fornix. The same was felt on per rectal examination. Laboratory investigation revealed normal hormonal profile. CA-125 was 25.8 IU/ml. Transabdominal USG showed absence of the uterus with a heterogeneously hypoechoic mass measuring 8×8 cm in the left side of the pelvis. Right ovary was normal in size, but left ovary was not visualised. MRI confirmed the well circumscribed mass in the pelvis of size 7×7 cm, with low to intermediate signal intensity on T2 weighted images . The mass also had maintained fat planes with urinary bladder and adjacent bowel loops. MRI also showed absent uterus and dilated left sided fallopian tube with hyperintense signal intensity on T2 weighted images suggestive of hematosalpinx. Both the ovary was found to be normal in location, size and signal intensity. On the basis of morphology and signal characteristics of the mass, provisional diagnosis of MRKH syndrome with leiomyoma from mullerian remnants with left sided hematosalpinx was made. IVP was normal and chromosomal study showed normal 46xx karyotype. Any associated Skeletal, hearing defect or cardiac anomalies are also ruled out in this patient by respective work up. With a diagnosis of MRKH syndrome associated with leiomyoma and left sided hematosalpinx, she was taken up for laparotomy. Intraoperatively no uterus was seen. On the left side, there was a large mass approx 7×7 cm seen, adhering to the rudimentary horn and distended fallopian tube with normal looking ovary. A small rudimentary horn measuring approx. 2×1 cm with normal ovary was seen on the right side. Both horns were seen to be attached with a fibrous band in between.[Fig.1]

Figure 1: Peroperative picture showing leiomyoma adherent with left rudimentary horn, right rudimentary horn with normal ovary, both horn connected by fibrous band and dilated left fallopian tube.
Removal of the mass with bilateral rudimentary horn with left sided salpingectomy was done.[Fig.2].

Figure 2: Excised specimen.
Cut section of the mass was grey white in colour and had whorled appearance. Histopathological examination revealed features of leiomyoma with rudimentary mullerian lining and haematosalpinx of left tube [Fig.3].
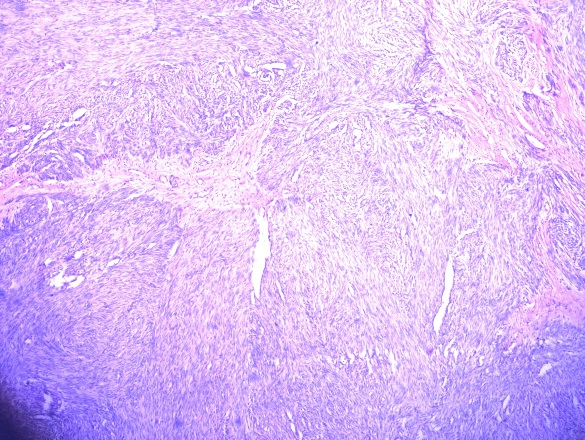
Figure 3: Microscopic image (Haematoxylin-eosin) showing tumour of smooth muscle cell origin, arranged in whorls suggestive of leiomyoma.
The patient had an uneventful recovery. The couple was given proper counselling emphasising the fertility potential and offered surrogacy. They opted the same and got successful result after.
Discussion
Mayer - Rokitansky – Kauster – Hauser (MRKH) syndrome is a rare disorder defined as varying degrees of uterovaginal aplasia due to early onset of arrest in the development of mullerian duct.[2] After gonadal dysgenesis, it is the second most cause of primary amenorrhea. Other characteristics of this syndrome are the presence of XX chromosome, normal female phenotype, normal ovarian function, and underdeveloped vagina.[3] They may also have associated renal, skeletal, cardiac and hearing defects which are ruled out in our patient.[4,5] But the presence of leiomyoma in MRKH syndrome make it a very rare event. Only a few cases are reported in literature.[6-8]
Etiopathogenesis of leimyoma in normal uterus is yet to be established. Their occurrence has been linked with various genetic predisposition, hormones and few growth factors by various studies. Leiomyomas are estrogen dependent tumours. So normal ovarian function and presence of smooth muscle cell in mullerian duct make leiomyoma in MRKH syndrome to be a theoretical possibility. However possible reason for the rare occurrence of leiomyoma in MRKH syndrome could be decreased concentration or sensitivity of the estrogen receptors.[9]
MRKH syndrome patients usually complain of primary amenorrhea and infertility. These typical symptoms make diagnosis of MRKH delayed till late puberty. Among them, 6-10% of the patient complaints of pelvic pain. Reasons may be hematometra,endometriosis and myoma.[10]
First diagnostic modality is trans abdominal ultrasound which shows absence of uterus with hypoechoeic mass in associated myomas like our case. The imaging technique of choice is MRI because of its excellent soft tissue resolution which make accurate evaluation of uterine aplasia as well as a clear visualisation of rudimentary horn and ovaries. MRI shows leiomyomas as masses of low to intermediate signal intensity compared to myometrium on T1 and T2 weighted images.[11] Diagnostic laparoscopy is the gold standard for definitive diagnosis of MRKH syndrome.[12]
Differential diagnosis of leiomyoma in mullerian remnant of MRKH syndrome may be gastrointestinal stromal tumour of intestine (GIST), ovarian fibroma and extravesical leiomyoma of the urinary bladder.[2]
Treatment of patients of leiomyoma with MRKH syndrome is myomectomy or hysterectomy and vaginal reconstruction.[2] In our case the vaginoplasty was not done due to the presence of a functional vagina already. With advances in minimal access surgery, the Vecchietti and Devydov procedures can now be performed. Surrogacy may be an important option for retaining motherhood. Proper counselling is very necessary to emphasise the fertility potential through surrogacy. For those who donot opt for surrogacy, adoption is another good option.
Conclusion
It is very rare to find leiomyoma to originate from fibromuscular tissue of remnant uterus in patients of MRKH syndrome. So this rare case is being reported. Excision of tumour with uterine remnant is indicated when symptomatic.
Acknowledgements
The authors would like to thank Dr. Pankaj Kumar Doloi of St. Stephen’s Hospital, New Delhi for ENT consultation and editing the article.
Funding Sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declarations Of Interest: The authors have no conflicts of interest relevant to this article.