
Caitlin G. Haydek MD1, Francisco Bravo Puccio MD2, Patricia Alvarez MD3, Juan Garcia MD4, Yoko Shuda5, Yuan Chang MD5, Carla Torres-Zegarra MD1
1Department of Dermatology, University of Colorado School of Medicine, Aurora, CO, USA.
2Universidad Peruana Cayetano Heredia, Lima, Perú.
3Patología cutánea, Lima-Perú.
4Pediatric Oncologist staff, Clinica Angloamericana.
5Hillman Cancer Center, Cancer Virology Program, University of Pittsburgh, Pittsburgh, PA 15213, USA.
*Corresponding author: Carla Torres-Zegarra, 5Hillman Cancer Center, Cancer Virology Program, University of Pittsburgh, Pittsburgh, PA 15213.
Received Date: February 28, 2024
Accepted Date: March 04, 2024
Published Date: March 08, 2024
Citation: Caitlin G. Haydek, Francisco B Puccio, Alvarez P, Garcia J, Shuda Y, Chang y, Carla Torres-Zegarra. (2024) “Trichodysplasia Spinulosa Successfully Treated with Topical 5-Fluorouracil.” Journal of Dermatology and Venereology, 2(1); DOI: DOI: 10.61148/JCED/005.
Copyright: © 2024 Carla Torres-Zegarra. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Trichodysplasia spinulosa is a rare skin condition by caused by trichodysplasia spinulosa-associated polyomavirus (TSPyV), which results in the development of folliculocentric papules in a subset of immunocompromised individuals. Treatment options classically include reduction of immunosuppression and topical or oral antivirals. We present the case of a 5-year-old Hispanic female with acute lymphoblastic leukemia and biopsy/immunohistochemistry confirmed trichodysplasia spinulosa due to TSPyV with resolution of her skin lesions with use of topical 5-fluoruracil. This is the first report of successful treatment of trichodysplasia spinulosa with topical 5-fluoruracil although the contribution of chemotherapy cessation during treatment cannot be discounted. Pending further evaluation, topical 5-fluoruracil may represent a new and readily available treatment option for this difficult-to-manage condition.
TSPyV; oral antivirals, lymphoblastic leukemia; biopsy/immunohistochemistry
Case:
A 5-year-old Peruvian female presented to clinic with a 2-month history of tiny, pinhead spicules on her face and body, predominantly clustered around her nares, bilateral helices, frontal hairline and occipital hairline (Figure 1).

Figure 1A: Skin findings on initial presentation. Tiny spicules on the ear and face.

Figure 1b: mSkin findings on initial presentation. Tiny spicules on the ear and face.
These skin findings were associated with moderate pruritus. The patient had a history of low-risk B-cell precursor acute lymphoblastic leukemia and had been undergoing chemotherapy for one and a half years prior to the onset of the rash. She was receiving vincristine, dexamethasone, mercaptopurine and methotrexate at the time of her clinic visit. A punch biopsy of a representative lesion was performed, and pathology demonstrated follicular plug filling the follicular infundibulum, as can be seen in lichen spinulosus and keratosis pilaris. Urea 10% cream was started as a topical keratolytic. The patient’s chemotherapy was completed one month later.
Due to a lack of clinical improvement after 4 months of use of keratolytics and cessation of chemotherapy, the patient returned for reevaluation. Additional biopsies of the ear and scalp were performed. Pathology revealed a normal epidermis and expanded anagen follicles with dilatation of the infundibula. Lack of hair formation was observed, and the follicles contained disorganized, hyperkeratotic masses of parakeratotic cells and eosinophilic debris. The follicular bulbs appeared abnormally large, and there was a marked expansion of the inner root sheath by abnormal germinal cells that contain numerous enlarged trichohyaline granules (Figure 2).
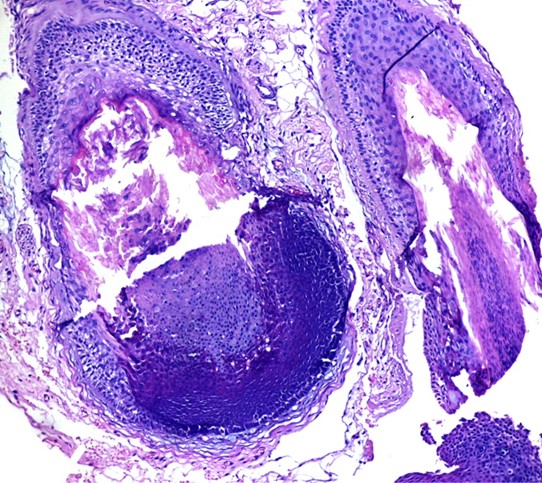
Figure 2a: Abnormal enlargement of the follicular bulbs with marked expansion of the inner root sheath by abnormal germinal cells that contain numerous enlarged trichohyaline granules (H/E 200x)
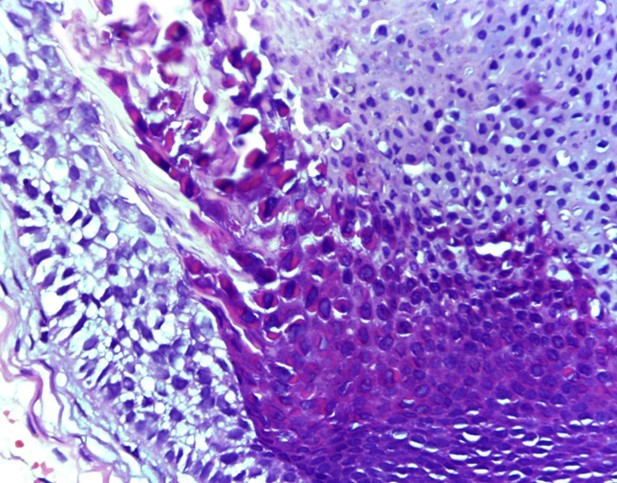
Figure 2b: Abnormal enlargement of the follicular bulbs with marked expansion of the inner root sheath by abnormal germinal cells that contain numerous enlarged trichohyaline granules (H/E 400x)
These findings were consistent with trichodysplasia spinulosa (TS) caused by the human TS polyomavirus (TSPyV).
The biopsy specimen was additionally processed for the presence of TSPyV using immunohistochemistry. Although an antibody directed specifically against TSPyV Large T antigen (LT Ag) has not been developed, the PAb416 antibody which broadly detects the LT Ag of several human polyomaviruses including TSPyV LT Ag (add REF: Toptan et al, JCI Insight. 2016 Feb;1(2):e85562 demonstrated positive staining in nuclei of cells populating the external root sheath in the deep follicle or bulb (Figure 3).
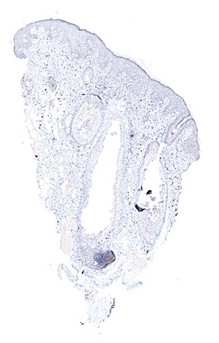
Figure 3a: Expression of TSPyV Large T antigen via the PAb416 antibody. Note the positive staining in nuclei of cells populating the external root sheath in the deep follicle (40x)
 Figures 3b and 3c: Expression of TSPyV Large T antigen via the PAb416 antibody. Note the positive staining in nuclei of cells populating the external root sheath in the deep follicle (200x)
Figures 3b and 3c: Expression of TSPyV Large T antigen via the PAb416 antibody. Note the positive staining in nuclei of cells populating the external root sheath in the deep follicle (200x)
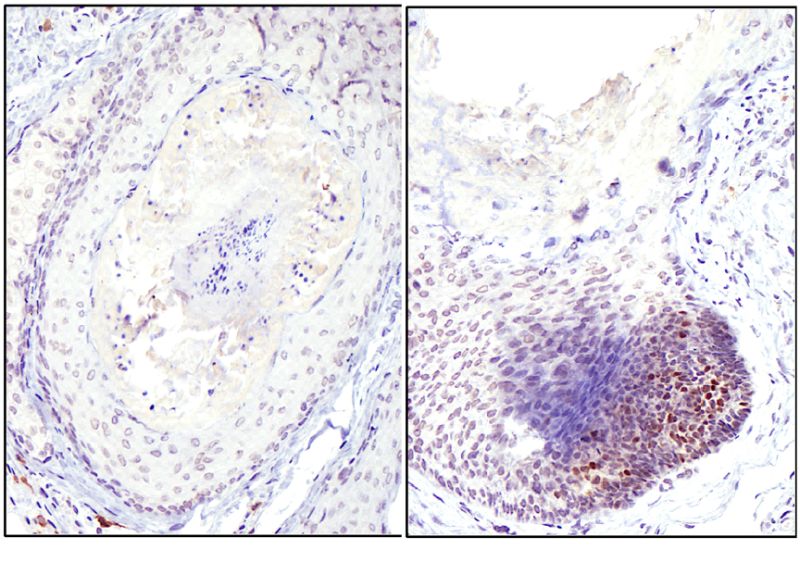
Additionally, positivity for the capsid protein (VP1) using a TSPyV-VP1 specific antibody, (TSP-VP1, clone #12) was also seen in the inner root sheath of follicles (Figure 4).
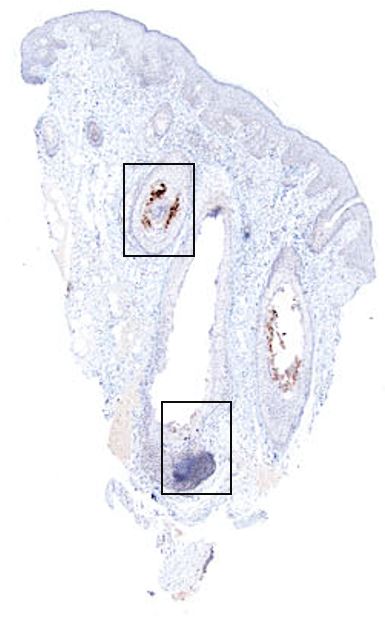
Figure 4a: Staning of the capside protein (VP1) via the TSV VP1#12 antibody. Note weak positive in the inner root sheath of follicles (40x).
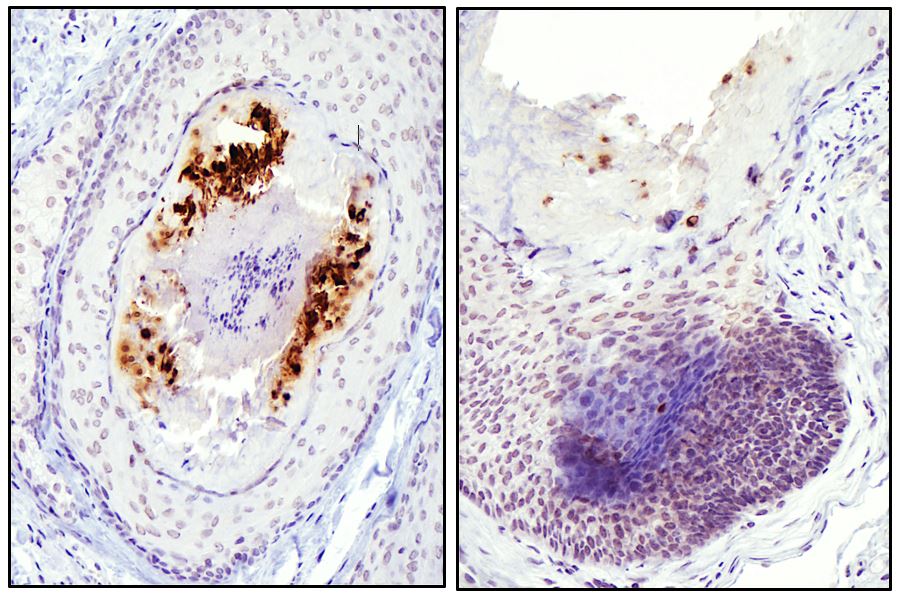
Figures 4b and 4c: Staning of the capside protein (VP1) via the TSV VP1#12 antibody. Note weak positive in the inner root sheath of follicles (200x)
This combination of antibodies confirms the specific involvement of TSPyV in the pathoetiology of this patient’s skin lesion.
Topical cidofivir was not locally available for treatment. Because of this, a trial of topical 5-fluorouracil cream was initiated. The cream was applied nightly to the affected areas. After 4 weeks, the patient had clearance of her skin lesions and resolution of associated pruritus (Figure 5).

Figure 5a: Resolution of skin lesions after treatment with topical 5-fluorouracil.

Figure 5b: Resolution of skin lesions after treatment with topical 5-fluorouracil.
The patient has not experienced recurrence for at least 1 year since completion of treatment.
Discussion:
Trichodysplasia spinulosa is a rare skin condition resulting in the formation of folliculocentric spiny papules, predominantly on the face, in immunocompromised patients.1 This condition is caused by trichodysplasia spinulosa-associated polyomavirus (TSPyV), a non-enveloped DNA virus.2 The seroprevalence for TsPyV is high across healthy populations, ranging from 41 to 70% in children ten years old and even higher rates in adults.3-6 Despite this high seroprevalence, it remains unknown why certain immunocompromised individuals manifest clinical findings of this infection while others do not.
A number of treatments have been proposed for trichodysplasia spinulosa and used with variable success, including oral antivirals, topical antivirals, oral leflunomide, manual extraction, keratolytics, and retinoids.7-9 Curman et al. reviewed trichodysplasia spinulosa treatment and suggested that first line therapy when reduction of immunosuppression is not possible is topical cidofivir 3%, which has been shown to inhibit human polyomavirus in vitro and reduce TSPyV viral load in patients treated with cidofivir 1%.2, 10, 11 There is also limited evidence for the use of oral valganciclovir.11 A recent case reported the successful use of photodynamic therapy for this condition in an adult patient, but the utility of this treatment in pediatric patients would likely be more limited due to potential side effects.12
Cidofivir is used as an off-label treatment for various human papillomaviruses and human polyomaviruses, both of which are non-enveloped DNA viruses. Cidofovir has been shown to be an effective treatment for plantar warts, and is thought to act through competitive inhibition of viral DNA polymerase.13 Unfortunately, topical cidofivir is not available in some countries, as in our case. Because of the similarities in use of topical cidofivir and topical 5-fluorouracil for warts caused by human papillomavirus, and the similarities in human papillomavirus and human polyomavirus, use of topical 5-fluoruacil was pursued with great success.14, 15
In our patient, with biopsy proven trichodysplasia spinulosa secondary to TSPyV, topical 5-flurouracil was used with complete, rapid resolution of her skin lesions. This topical treatment occurred after cessation of chemotherapy for the patients low-risk B-cell precursor acute lymphoblastic leukemia, and it is unknown what degree of immune reconstitution may have occurred and contributed to the effectiveness of topical 5-flurouracil treatment. To our knowledge, this is the first description of topical 5-fluorouracil being used as an effective treatment for trichodysplasia spinulosa and, pending confirmation, may represent a more cost effective and widely available treatment than topical cidofivir.