
Amit Mandal
Department of Cardiology Christian Medical College Vellore.
*Corresponding Author: Amit Mandal, Department of Cardiology Christian Medical College Vellore.
Received Date: January 29, 2024
Accepted Date: April 22, 2024
Published Date: May 20, 2024
Citation: Amit Mandal. (2024) “Hemoptysis as an Index Presentation of Thoracic Aortic Aneurysm: An Unusual Scenario.”, International Journal of Medical Case Reports and Medical Research, 2(5); DOI: 10.61148/2994-6905/IJMCRMR/023.
Copyright: © 2024. Pramod Yadav. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Thoracic aortic aneurysm is a rare vascular disease. Patients with thoracic aneurysms are often asymptomatic at the time of presentation. Index presentation is usually due to compression of adjacent structures. Hemoptysis as a first presentation is usually rare. Here we present a case of a middle-aged gentleman who presented with recurrent blood in sputum and later diagnosed to have Thoracic aortic aneurysm.
Introduction:
Thoracic aortic aneurysm is a rare vascular disease. Patients with thoracic aneurysms are often asymptomatic at the time of presentation. Index presentation is usually due to compression of adjacent structures. Hemoptysis as a first presentation is usually rare. Here we present a case of a middle-aged gentleman who presented with recurrent blood in sputum and later diagnosed to have Thoracic aortic aneurysm.
57-year-old gentleman was admitted to hospital with history of recurrent blood in sputum around 5-6 cc for last two months. He was evaluated at a primary health care centre where he told to have a probable left sided lung mass on chest Xray, and he was referred to higher centre. He did not notice any fever, night sweats, loss of appetite or weight. There was no history of dysphagia, hoarseness of voice, chest pain, dyspnoea, back pain, or chest trauma. He presented to our emergency department after having a massive haemoptysis episode of 250 ml in the morning on the day of admission. He was a known case of diabetes mellitus for last five years. He was a heavy smoker (Occasional uses of E-Cigarette in the past) with no alcohol dependence.
On Arrival his blood pressure was 120/80 in both arms and heart rate was regular at the rate of 82 beats per minute. Respiratory rate was 18 breaths/minute and arterial oxygen saturation was 98% in room air. Rest of his systemic examination was unremarkable.
This gentleman presented with insidious onset and gradually progressing hemoptysis episodes of two months duration. Differentials considered were,
His routine blood investigations including bleeding parameters were within normal limits.
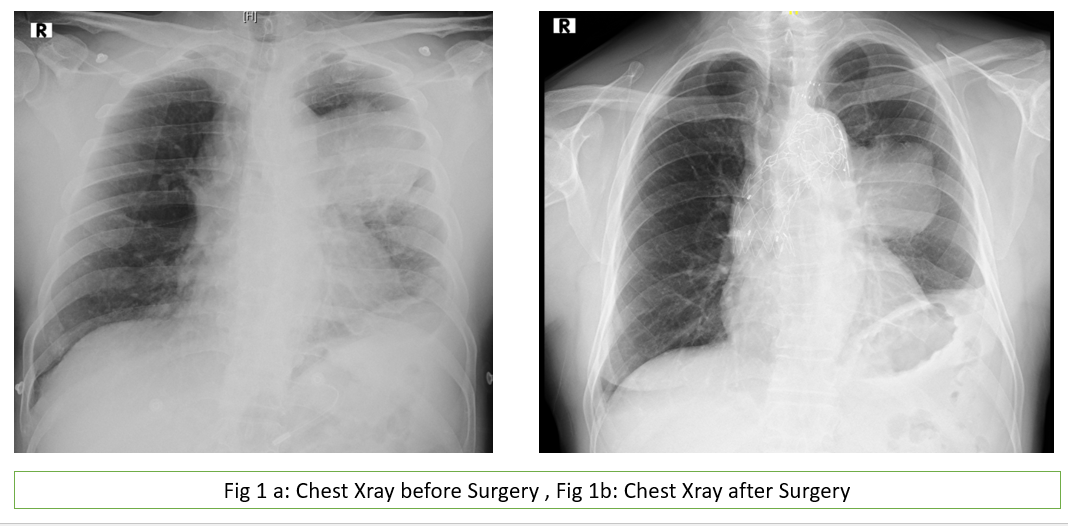
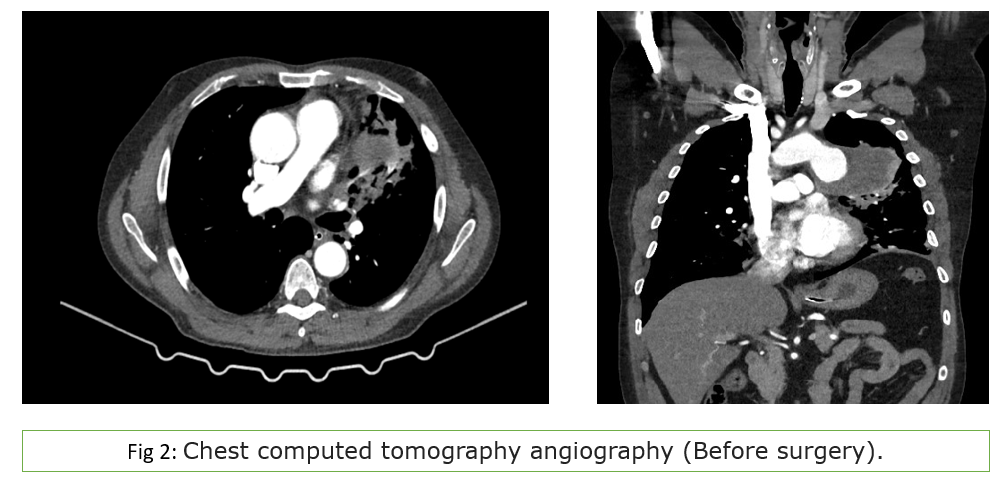
His chest Xray revealed mediastinal widening which was suggestive of mediastinal mass (figure1a %1b). He underwent CT angiogram (Fig 2a &2b) which showed a saccular pseudoaneurysm measuring 9.0 x 5.6 x 5.1 cm, arising from the anterolateral wall of arch of aorta with peripheral hypodense area (likely thrombus). There was dehiscence in the wall with fistulous communication with the subsegmental bronchus in the adjacent lung parenchyma which showed collapse consolidatory changes.
Considering the large size of the aneurysm and ongoing hemoptysis and to emergency fenestrated endovascular aortic repair (Ishimaru Zone 0 repair) of ruptured distal aortic arch aneurysm done under general anaesthesia was performed. (Fig 3a & 3b)
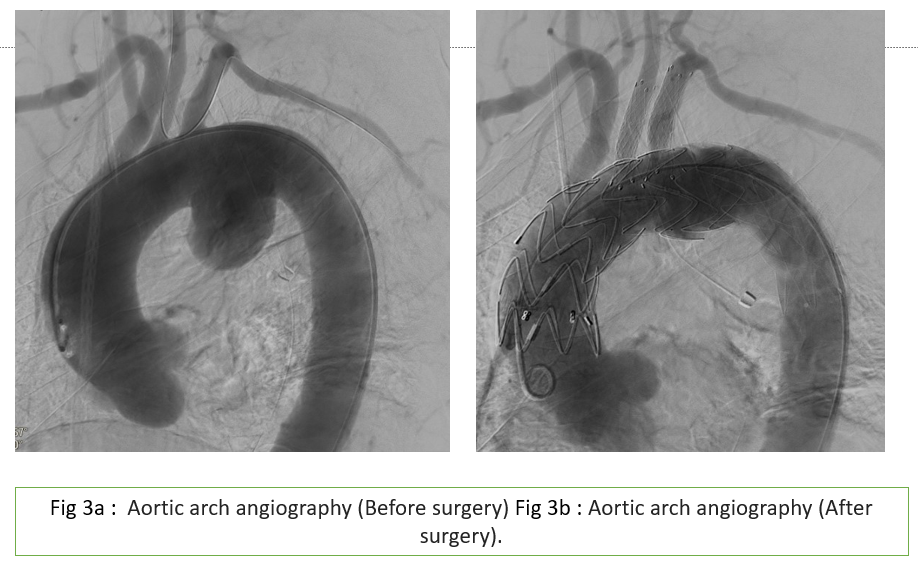
Pre-fenestrated Valiant thoracic endograft(38-38-200mm) was taken up to the LCCA fenestration just proximal to the LCCA marking with the correct linear and rotational orientation. The first stent was initially released - anchoring the proximal end of the graft following which the rest of the endograft was released with concomitant RV pacing. The orientation of the fenestrations was checked by the systemic blood pressures noted in the right radial artery, LCCA and LRA sheath pressures. After confirming the wire position in the respective fenestrations, Roadrunner wire loop was removed sequential stenting of the arch branches done. LCCA artery- A Fluency 9x40 mm self-expanding covered stent was deployed with optimal projection into the aorta. It was post-dilated with Mustang 7x20mm balloon at 14 atm. LSA artery- A Fluency 12x40 mm self-expanding covered stent was deployed with optimal projection into the aorta. It was post-dilated with 8x20 ATB balloon at 14 atm. Pigtail angiogram showed well-deployed fenestration stents with no endoleak.
Post operative his hemoptysis disappeared and he was discharged seven days later. Follow up visit after 2 weeks, there was no further episodes of hemoptysis, and he had no other discomfort other than mild chest tightness.
Discussion:
Thoracic aortic aneurysm (TTA) is a rare vascular disease. It is often difficult to assess the incidence and prevalence of this disease because at times it is clinically silent. In previous studies the annual incidence of TAA was estimated to be 5.6 and 10.4 cases per 100,000 patient years making it a relatively rare disease. [1,2] Thoracic aneurysm mostly occurs in six or seventh decade and more common in males. Most TAA are degenerative in origin and atherosclerosis and hypertension, aortitis secondary to infections or inflammatory disorders like giant cell arteritis, Takayasu arteritis, IgG4 related disease, rheumatoid arthritis, Bechet syndrome are other aetiology of TAA.[3] Natural history of the disease is generally associated with slow expansion and as the aorta enlarges there is an increased risk of sudden aortic dissection. Patients with thoracic aneurysms are often asymptomatic at the time of presentation. When present, symptoms are usually due to compression of adjacent structures, leading to chest, back, flank, or abdominal pain, pulmonary symptoms, or signs of nerve compression (eg, hoarseness, diaphragm paralysis). An aortic aneurysm or dissection that ruptures into the lung parenchyma or erodes into a bronchus can lead to acute and massive hemoptysis. [4] Aorto-bronchopulmonary fistulas account for 85% of cases of hemoptysis that occur in conjunction with a descending thoracic aneurysm. Thoracic aortic aneurysms with a small amount of hemoptysis as the initial symptom are rare in clinical practice, and only few case reports have been documented in literature and the mortality rate without surgical or interventional treatment is almost 100%. For patients with surgical indications, surgical treatments such as thoracic endovascular aortic repair (TEVAR) is always recommended.
Conclusion:
Thoracic aortic aneurysm is a relatively rare disease and high index of suspicion is required to diagnose a case, especially presenting with relatively uncommon index presentation like hemoptysis.
Due to extreme high mortality associated with the disease, five-year survival of untreated patients is only 10%. Hence patient suspected to have aortic aneurysm with hemoptysis urgent imaging in the form of
CT angiogram should be performed. For patients who has surgical indications it is advisable to actively perform procedure such as thoracic endovascular aortic repair (TEVAR)
Early diagnosis and appropriate treatment improve prognosis.