
Ashwin Agrawal, Sameer Imdad, Lesley Small-Harary, Anupama Chawla and Keith Breglio*
Division of Pediatric Gastroenterology and Nutrition, Department of Pediatrics, Stony Brook Children’s Hospital, Renaissance School of Medicine, Stony Brook, NY.
*Corresponding Author: Keith Breglio, Division of Pediatric Gastroenterology and Nutrition, Department of Pediatrics, Stony Brook Children’s Hospital, Renaissance School of Medicine, Stony Brook, NY.
Received Date: April 11, 2024
Accepted Date: April 22, 2024
Published Date: April 25, 2024
Citation: Ashwin Agrawal, Sameer Imdad, Lesley Small-Harary, Anupama Chawla and Keith Breglio. (2024) “Crohn’s or Eating Disorder: The Role of Fecal Calprotectin.”, International Journal of Medical Case Reports and Medical Research, 2(4); DOI: 10.61148/2994-6905/IJMCRMR/038.
Copyright: © 2024. Keith Breglio. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Diagnosing Crohn’s Disease (CD) in the setting of Anorexia nervosa (AN) is challenging with overlapping symptomatology. We present a 19-year-old female with AN hospitalized for weight loss with non-specific gastrointestinal symptoms. Elevated fecal calprotectin and inflammatory markers raised suspicion of CD. She underwent an esophagogastroduodenoscopy, colonoscopy, and magnetic resonance enterography revealing mucosal erosions/ulcerations and small bowel wall thickening, diagnosing CD. She was started on infliximab therapy with subsequent weight gain, normalization of inflammatory markers, and improved fecal calprotectin. This case emphasizes the importance of checking fecal calprotectin to evaluate suspicion of CD in a patient with anorexia nervosa.
Introduction:
Crohn’s disease (CD) is an inflammatory bowel disease (IBD) characterized by a chronic immune-mediated process that affects the intestines. Common symptoms include abdominal pain, diarrhea, rectal bleeding, and weight loss. [1] Up to 25% of IBD is diagnosed prior to the age of 20 years. Eating disorders are seen in high prevalence in this age group as well. Typical symptoms of eating disorders include anxiety or fear around eating, limiting caloric intake, and weight loss. [2] Given the overlap of symptoms, CD can be difficult to identify in patients with suspected eating disorders. Biochemical markers can help differentiate patients with intestinal inflammation from those with functional disorders. Fecal calprotectin has a high predictive value and sensitivity in detecting intestinal inflammation.[3] We present a case of an adolescent initially hospitalized for an eating disorder eventually diagnosed with CD with the help of fecal calprotectin testing.
Case Presentation:
A 19-year-old female presented with depression, weight loss, and malnutrition. She reported unintentional weight loss of 15 pounds over two years attributed to lack of appetite. She denied body image issues or a desire to lose weight. Initial labs were significant for mild leukocytosis, thrombocytosis, and low prealbumin. She was followed by adolescent medicine and received psychotherapy. She had complaints of early satiety and epigastric pain with a few episodes of non-bloody, non-bilious emesis, which resolved with H2 antagonist therapy. The patient denied diarrhea, hematochezia, or stool urgency. She initially showed weight gain in response to cyproheptadine; however, cyproheptadine was discontinued due to fatigue.
She was admitted to adolescent medicine eleven months later due to continued weight loss. The admission weight was 27.6 kg. Initial labs revealed WBC 14.4 x10^3/mL, Hgb 11.9 g/dL, ESR 49 mm/hr (normal 0-19), albumin 3.5 g/dl, and pre-albumin 15.6 mg/dl. Repeat ESR the following day was 19 mm/hr. Two weeks later, repeat labs revealed albumin of 2.5 g/dL, Hgb of 9.6 g/dL, ESR of 74 mm/hr, and CRP of 2.9 mg/L (normal <0.5).
Pediatric Gastroenterology was consulted and recommended celiac serologies and stool occult blood which were normal. A fecal calprotectin was elevated to >3000 mcg/g (normal <50). The patient underwent an EGD and colonoscopy. The EGD was significant for erythematous mucosa in the gastric body. The duodenum was dilated with diffuse erythema, localized erosions, friability, and deep ulcerations (Figure 1). Colonoscopy, including the terminal ileum, was grossly normal. Pathology revealed duodenitis and colitis. Magnetic Resonance Enterography (MRE) showed a long segment of proximal small bowel wall thickening and inflammation suggestive of small bowel Crohn’s disease (Figure 2).
The patient was subsequently diagnosed with CD and started on infliximab (IFX) 10 mg/kg/dose. Due to poor clinical response with undetectable IFX levels, IFX was increased to every 2-weeks and prednisone was initiated. Therapeutic IFX levels were achieved. Steroids were tapered and discontinued. IFX was spaced to every 8 weeks. Clinically, the patient reported resolution of her GI symptoms and improvement in appetite. After 12 months, the patient gained 12.2 kg from her lowest recorded weight (Figure 3). She had normalization of her Hgb, albumin, ESR, and CRP. In addition, her fecal calprotectin improved to 148 mcg/g.
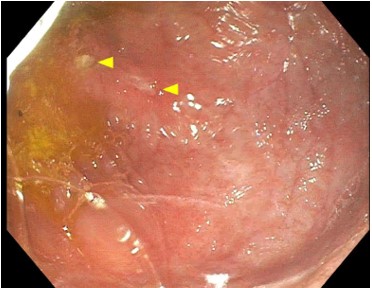
Figure 1: The figure shows the patient’s duodenum seen on upper endoscopy. The yellow arrows point to ulcerations. The mucosa is also seen to be erythemous and friable.
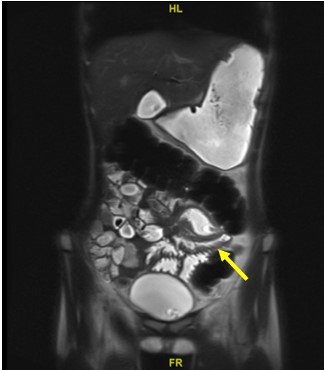
Figure 2: MRE image with yellow arrow pointing to the area of terminal ileum with bowel wall thickening.
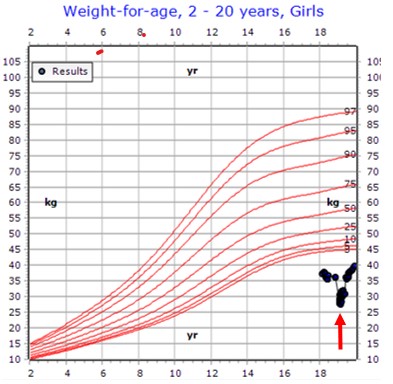
Figure 3: This figure shows the weight of the patient. The red arrow is the patient’s lowest weight. The figure shows the significant weight gain that occurred with initiation of infliximab therapy.
Discussion:
One must have a high suspicion for IBD, especially CD, in patients diagnosed with anorexia nervosa (AN) unresponsive to treatment. IBD is a chronic immune-mediated disease that affects the gastrointestinal tract. The incidence of IBD has been increasing worldwide [1].
Patients with IBD can have varied intestinal and extraintestinal symptoms. GI symptoms include abdominal pain, constipation or diarrhea, fever, oral ulcerations, hematochezia, weight loss, anorexia, bowel obstruction, among others. [1] Extraintestinal symptoms can include uveitis, erythema nodosum, pyoderma gangrenosum, alopecia, pancreatitis, iron deficiency anemia, osteopenia, arthritis, and others. [1] As there are varied phenotypic presentations of IBD, the practitioner must carefully consider IBD when any of these symptoms are present even in isolation.
Eating disorders are diagnosed based on DSM-5 criteria. Studies show the lifetime prevalence of eating disorders ranges from 1-22.7% for females and 0.3-0.6% for males. [2] Diagnosis of eating disorders is primarily based on history and symptoms. Patients often have significant anxiety or fear around eating, body dysmorphia, fear of weight gain, constipation, and changes in exercise and eating behaviors. [2]
Previous publications have reported associations between eating disorders and CD. One study reported an increased prevalence of eating disorder behaviors in patients with CD. [4] A study in Sweden of 2.5 million individuals revealed an increased risk of AN in females diagnosed with CD. [5] This same study showed an increased risk of CD in females initially diagnosed with AN [5]. Another study of 109 adults with IBD revealed that 13% had disordered eating. [6] This study also found a greater risk of eating disorders in patients diagnosed with IBD in childhood. [6] Few case reports have shown delayed diagnosis of CD in patients initially diagnosed with eating disorder. [7,8] There have been reports of a dual diagnosis of AN and CD. [9]
High suspicion of an organic pathology instead or in association with AN should be noted if the patient denies body image issues as demonstrated in a case series of four pediatric patients with AN ultimately diagnosed with CD. [7] Though laboratory evaluation for IBD often demonstrates abnormalities in hemoglobin, WBC count, albumin, and inflammatory markers, many IBD patients can have normal lab values. [10] In our case, obtaining a fecal calprotectin was crucial in leading to the diagnosis of IBD in the absence of classic symptoms. Fecal calprotectin measures a protein in neutrophils that migrates into intestinal mucosa in the setting of inflammation and is sensitive for detecting intestinal inflammation [3]. A recent study found that the positive predictive value and sensitivity of FC were 83% and 36%, respectively, in identifying ileal CD [3].
Due to the overlap in symptoms that can occur in both AN and CD, a high level of suspicion for IBD should be maintained in certain patients. In patients denying body dysmorphia, a fecal calprotectin can help determine the need for further workup for IBD. With prompt treatment of her IBD, our patient was able to gain weight successfully with marked improvement in her quality of life.
Author Contributions: Each author was involved in planning/writing/editing of this article and meets ICMJE guidelines for authorship.
Acknowledgements:
No financial contribution was provided for writing this article.
The corresponding author affirms that everyone who contributed significantly to the work is listed as an author.
Conflict of Interest: Authors have no conflicts of interest to disclose.
List of Abbreviations:
CD – Crohn’s disease
AN – Anorexia nervosa
IBD – Inflammatory bowel disease
WBC – White blood cell
Hgb – Hemoglobin
ESR – Erythrocyte sedimentation rate
CRP – C-reactive protein
EGD – Esophagogastroduodenoscopy
MRE – Magnetic resonance enterography