
Abdulwahab F. Alahmari
Radiology Specialist, Radiology Department, Al-Namas General Hospital, Ministry of Health, Al-Namas City, Saudi Arabia.
*Corresponding Author: Abdulwahab F. Alahmari, Radiology Specialist, Radiology Department, Al-Namas General Hospital, Ministry of Health, Al-Namas City, Saudi Arabia.
Received Date: June 13, 2024
Accepted Date: June 21, 2024
Published Date: June 26, 2024
Citation: Abdulwahab F. Alahmari. (2024) “Idiopathic Lower Back Pain Causes: Iliolumbar Ligament Variations or Thoracolumbar Fascia Involvement.”, International Journal of Medical Case Reports and Medical Research, 3(2); DOI: 10.61148/2994-6905/IJMCRMR/048.
Copyright: © 2024. Abdulwahab F. Alahmari. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Idiopathic lower back pain is affecting many patients and it’s causes are unknown so far. But there are two possibilities that are causing the idiopathic lower back pain, which are iliolumbar ligament anatomical variations or thoracolumbar fascia involvement. The iliolumbar ligament passes through it many spinal nerves, which could be compressed when the nerve passes through a narrow space in the iliolumbar ligament. Microtraumas to the iliolumbar ligament can cause the ligament to compress the passing spinal nerve through it. The thoracolumbar fascia can increase in thickness and show shear strain on ultrasound imaging. On a lateral X-ray, it will show a straight vertebral column.
idiopathic lower back pain; iliolumbar ligament; thoracolumbar fascia; magnetic resonance imaging
Introduction:
Idiopathic lower back pain is very common, but its causes are unknown. The prevalence of Lower Back Pain (LBP) is affecting 80% of adults at some point worldwide [1, 2, 3, 4]. Women are more affected by LBP [1]. The iliolumbar ligament connects the iliac crest with the body and the transverse process of the fifth lumbar vertebra (L5) in 96% of the patients [5]. The nerve that is closer to the area is the 5th lumber plexus, which supplies the superior gluteal, inferior gluteal, common fibular, tibial, quadratus femoris, inferior gemellus, and obturator internus. The iliolumbar ligament developed at an early age (i.e. at 12 weeks of gestation). It is easily recognized from quadrates lumborum muscle by seeing the direction of the muscle fiber bands (craniocaudal) and the ligament fibers (horizontal).
Theories of Idiopathic Lower Back Pain Causes:
Many cases of chronic low back pain come from micro-trauma to the iliolumbar ligament because: [1] it is the weakest link of the multifidus triangle; [2] its angulated attachment makes it more vulnerable to injury; [3] it is the main inhibitor of excessive sacral flexion; [4] it is a highly innervated nociceptive tissue; and [5] it has a greater role in progressive disc degeneration [6]. The anatomical variation could be in the ligament or in the spinal nerve path see (Figs. 1 and 2). Some spinal nerves might be crossing in the wrong space. The iliolumbar ligament could have any type of variation, like a small gap to let the nerves pass through or a large part that compresses the spinal nerve from above (i.e. the craniocaudal part).
The fascial system is an underestimated system in the human body that is responsible for many pathologies, but medical professionals ignore it [7, 8]. The Terminologia Anatomica replaced the term “superficial fascia” with “hypodermis” or “subcutaneous fat” [9, 10]. In line with how the surgeons use it, when they use the word "fascia,” they refer to the deep fascia. Radiological imaging can’t effectively resolve the superficial fascia’s deep membranous layer, so subcutaneous fat is a better term to be used as a simple nomenclature. The connective tissue lining the body cavities is called visceral fascia, but it has specialized names like omentum, peritoneum, etc.
The Thoraco-Lumbar Fascia (TLF) is an aponeurotic complex layer that separates the paraspinal muscles and posterior abdominal wall. TLF is attached to the thoracolumbar spinous processes and the cranial edge of the ilial wing see (Fig. 3). These anatomical relations cause LBP when there is tension and stiffness in the fascia. Chronic tension in the aponeurotic tissue and it affects the posture and alignment of the patient. On a simple lumbosacral lateral X-ray, the muscle spasm can be seen as a straightened vertebral column (with no knee flexion). TLF can be evaluated using ultrasound imaging, which in cases of idiopathic lower back pain will show decreased shear strain and 25% increased thickness [11, 12, 13, 14].
Idiopathic LBP is defined as pain in the lower back in patients who have normal X-rays and MRI scans. But other imaging modalities, like ultrasound, might help in assessing the TLF. As well, any pressure on a spinal nerve branch that is so small that an MRI scan might not be able to visualize it or the pressure on that nerve might cause pain that is undetected on MRI scans. A lateral X-ray of the lumbosacral spine might show a straightened vertebral column.
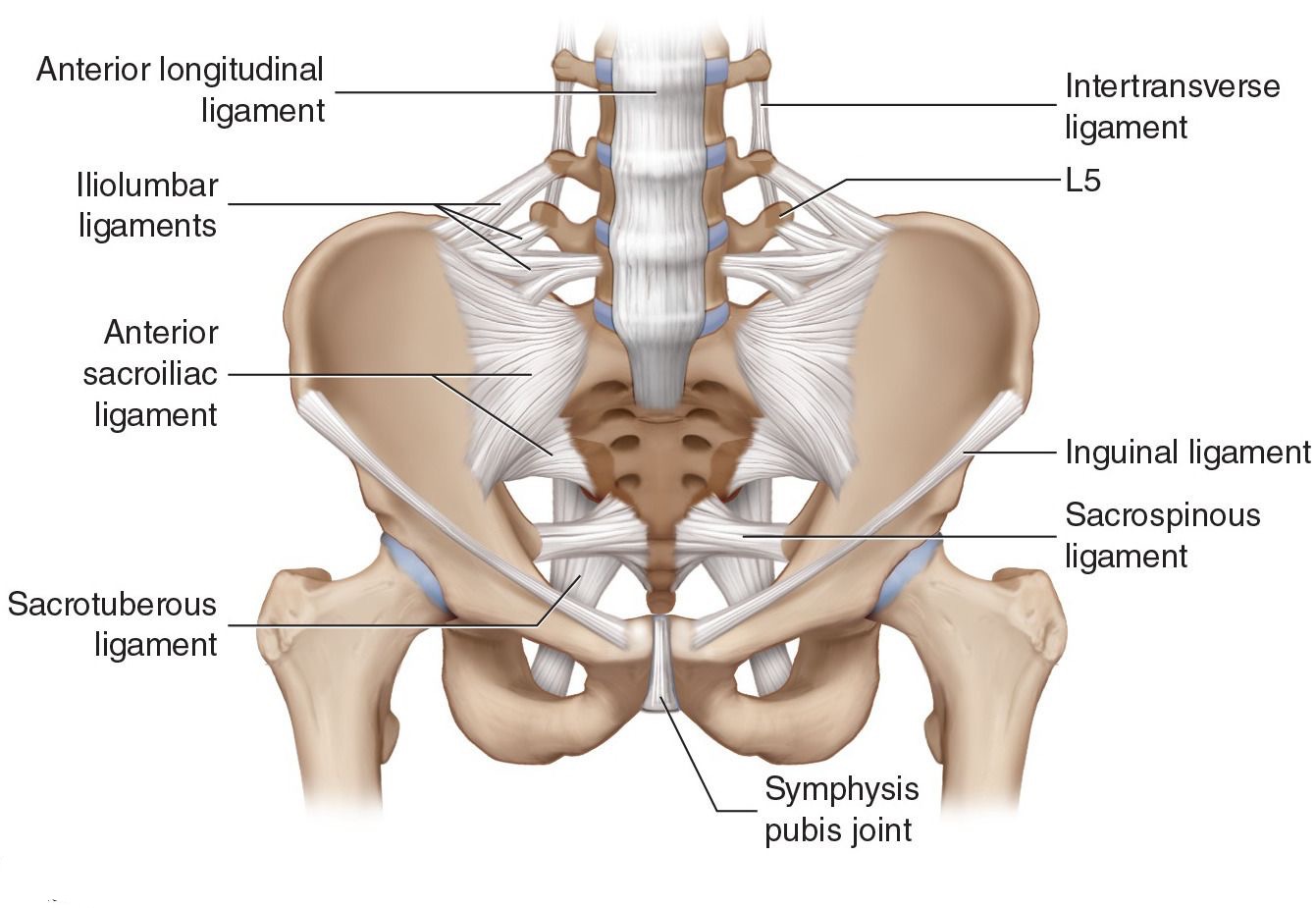
Figure 1: The anatomy of the iliolumbar ligament. The gap
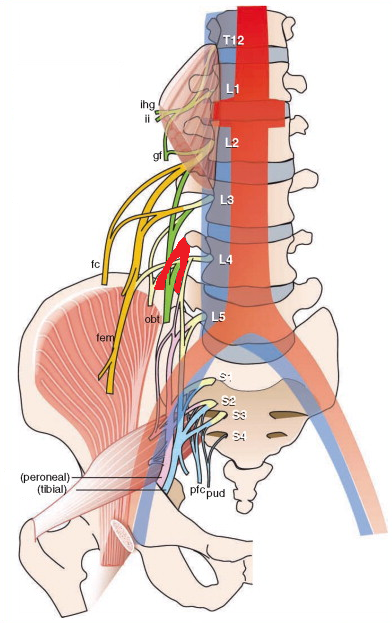
Figure 2: The iliolumbar ligament compresses the spinal nerves passing through the ligament.
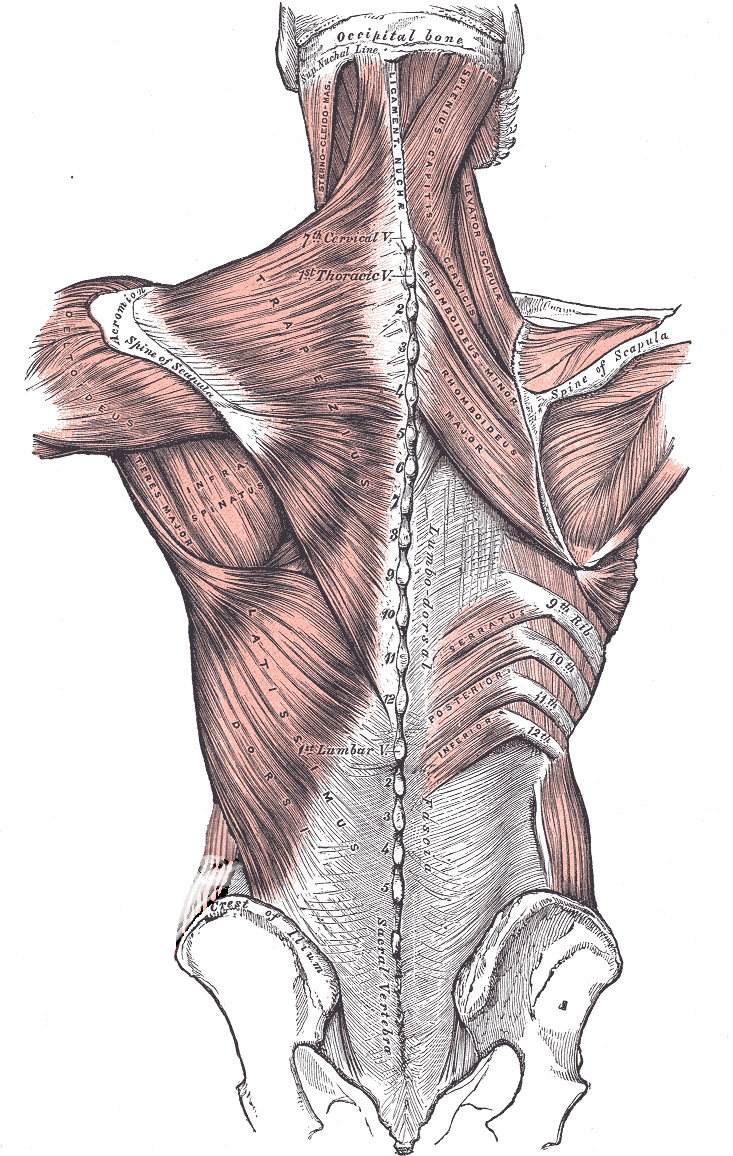
Figure 3: An illustration of ThoracoLumbar Fascia attachments.
Discussion:
Other authors claim that Diffuse Idiopathic Skeletal Hyperostosis (DISH) is the cause of LBP [15]. Other authors claim that the cause of LBP is the anterior dysfunction of the sacroiliac joint [16]. Scoliosis in young patients was considered another reason for LBP [17]. Others claim that vitamin D deficiency is the cause of LBP [18]. Another paper claims that the cause of LBP is postural muscle fatigue [19]. Other authors claim that age plays a major role in LBP [20]. DISH was tested and found to not be a factor that can cause LBP [21]. Many authors claim that LBP is psychological or has to do with socioeconomic status, but this paper is more focused on the biological causes of idiopathic LBP.
Conclusion:
Idiopathic LBP could have many factors that contribute to having non-explained LBP. Further investigation using ultrasound to assess the TLF might help. As well, EMG assessments of postural muscles might show fatigue in these muscles. A straight vertebral column on a lateral X-ray with extended knees indicates stiff TLF. Better imaging modalities with high sensitivity and specificity for imaging spinal nerve branches might show these nerves and any pressure on them by the iliolumbar ligament.