
Ramna Shafique*, Muhammad Abdullah, Tooba Nasir, Sundas Salim and Sehrish Ahmed
Ramna Shafique, Final year Medical Student, Ziauddin Medical College, Karachi, Pakistan
*Corresponding Author: Ramna Shafique, Ramna Shafique, Final year Medical Student, Ziauddin Medical College, Karachi, Pakistan.
Received Date: June 01, 2024
Accepted Date: June 10, 2024
Published Date: June 14, 2024
Citation: Ramna Shafique, Muhammad Abdullah, Tooba Nasir, Sundas Salim and Sehrish Ahmed. (2024) “Awareness and Impact of Covid-19 on Diabetic Patients in Terms of Lifestyle and Behaviour Changes.”, International Journal of Medical Case Reports and Medical Research, 3(1); DOI: 10.61148/2994-6905/IJMCRMR/044.
Copyright: © 2024. Ramna Shafique. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background: Diabetes mellitus (DM) is a non-communicable, chronic health disease with a rising incidence worldwide, affecting around 422 million adults. COVID- 19 outbreaks have exacerbated the severity and fatality of comorbidities, including DM. Lifestyle changes, a lack of information, and poor adherence contribute to the rise of DM. Identifying knowledge, attitudes, and practises related to DM in the public provides insight into preventive strategies. Self-management skills are crucial for T2DM patients.
Methods: This descriptive cross-sectional study was conducted from February 2022 until June 2022 among Karachi residents, using non-probability consecutive sampling. Data were collected from 219 participants through an online and hardcopy questionnaire. SPSS version 24 analyzed data using mean, standard deviation, frequency, and percentages. Chi-square tested gender associations with a significant p-value of ≤0.05.
Result: 219 participants responded to the survey. There were 50.7% males and 49.3% females. The age group was divided into nine subgroups spanning from 10 to 60, with a mean and standard deviation of 4.291 ± 632. COVID-19 had no impact on the health of our 124 participants (56.6%). The great majority of our participants (91.3%) had undergone vaccination.
Conclusion:In conclusion, the COVID-19 pandemic poses a challenge for individuals with diabetes, but there is no evidence of high susceptibility to the coronavirus infection. Most participants were vaccinated without complications. Awareness of COVID-19 complications and preventive measures was high, but some did not take precautions. It is crucial to manage diabetes effectively and prevent the spread of COVID-19.
coronavirus; medical care; lockdown; pandemic; worries; medication
Introduction:
Globally, diabetes mellitus (DM) is a prevalent and devastating chronic non-communicable disease, with an incidence rising dramatically and reaching epidemic proportions [1]. According to the World Health Organization (WHO), diabetes affects approximately 285 million people and causes 3.2 million deaths annually, or 8,700 people every day [2]. The International Diabetes Federation (IDF) forecasts that the number of adults with DM worldwide will increase from 382 million in 2013 to 592 million by 2035 [4]. Approximately 422 million people worldwide are expected to have DM [3]. According to recent predictions, by 2040, there might be up to 642 million cases of DM worldwide [5]. In Pakistan, diabetes is on the rise, with severe consequences leading to a high rate of mortality [6].
Globally, COVID-19 outbreaks have severely impacted the population, including those in Pakistan [7]. The coronavirus (COVID-19) is a public health emergency worldwide that has imposed a significant burden on the world, particularly in impoverished nations [8]. As a result, the Pakistani authorities originally implemented a complete lockdown to combat the virus's spread [9]. Research has shown that COVID-19 is more severe and lethal in the elderly or in people with underlying comorbidities such as diabetes, cancer, heart disease, lung, or kidney illness [10]. Diabetes mellitus is a chronic illness that can occur in both rural and urban locations, affecting people of all ages and genders [11].
Non-communicable diseases, including diabetes, have been on the rise due to significant lifestyle changes that coincide with economic transformation, industrialization, urbanization, and globalization [12]. Physical inactivity, obesity, and unhealthy diets, along with a genetic predisposition, are significant risk factors for type 2 diabetes (T2DM) [13].
Lack of information, poor adherence, and resistance greatly affect patients’ wellness and lifestyle changes, which is a problem that both patients and healthcare professionals must deal with [14]. The lack of literacy, the use of other forms of therapy, inadequate diabetes awareness, and polypharmacy are all potential causes of nonadherence to medication [15].
Improving the knowledge, attitude, and practice of T2DM patients and the general population is vital to controlling the disease [16]. Greater efforts must be made to investigate other factors affecting glycemic control among T2DM patients in Pakistan [17]. Public awareness campaigns along with targeted counseling from healthcare professionals have been proposed as ways to improve the practices of people with diabetes mellitus [18]. With the increasing complexity of medical procedures and therapy regimens, elderly individuals need special attention in today's healthcare system. Reflecting their age and sometimes low health literacy, older people are more likely to experience problems with medication adherence, lower self-management, and higher rates of hospitalization [19].
Although previous literature has focused on knowledge and health perspectives on diabetes among diabetic patients, the data is insufficient regarding community-level awareness and understanding of diabetes risk [20]. Evidence suggests that the dissemination of educational resources regarding diabetes to the general population has been effective in enhancing people's knowledge about the disease [21].
The global prevalence of type 2 diabetes mellitus is quickly rising, along with increases in obesity, less physical activity, and dietary shifts towards unhealthy eating behaviors [22]. In terms of treatment for diabetes, the majority of respondents said that prescribed medications were the best option, followed by insulin, a balanced diet, regular exercise, and weight control [23].
The majority of type 2 diabetic patients were already disengaged from lifestyle therapy, which meant they were less motivated to comprehend the nutritional value of meals, and they did not apply these competencies during insulin administration [24].
Methodology:
A descriptive cross-sectional study was conducted from February 2022 until June 2022 among Karachi residents. At least six months prior the COVID-19 outbreak, the participants had diagnosed with diabetes. A self-reported, semi-structured e-questionnaire was created using prior research. The study included adult patients aged 10 to 90 years who were able to read and write Urdu, the native language of Pakistan, and who had a confirmed diagnosis of Type 1 or Type 2 diabetes at least six months before the COVID-19 epidemic. Pregnant women, non-diabetic individuals, and people with psychiatric illnesses will be excluded from this study.
Questionnaires were filled out using Google Forms and forwarded through WhatsApp. Some Google Forms were filled out on the spot by our researcher, and manually filled-out forms were also provided to the participants after getting their informed consent. The questionnaire is divided into four sections, with three sections of closed-ended questions and one section of open-ended questions. Descriptive statistics were computed for each of the five categories. Inferential statistics included chi-square to analyse the interdependence of COVID-19-specific diabetes worries in terms of demographics, impact of COVID/diabetes worries, lifestyle and behavioural changes, and awareness of COVID in diabetic patients. P values were considered statistically significant if their significance levels were less than 0.05. All statistical calculations were carried out using IBM SPSS version 24.
Result:
Demographic:
The survey received responses from 219 people. There were (n = 111, 50.7%) men and (n = 108, 49.3%) women. The age group was divided into nine subgroups ranging from 10 to 60, with a mean & standard deviation of 4.291 ± 632. The oldest respondents (n = 66, 30.1%) were over 60, while the youngest (n = 18, 8.2%) were aged 10 to 20. Currently, (n = 24; 11%) of respondents are smokers, (n = 30; 13.7%) are ex-smokers, and (n = 165; 75.3%) are non-smokers.
Our participants were classified into five primary ethnic groups, with the majority speaking Urdu (n = 73, 33.3%), Sindhi (n = 64, 29.2%), Punjabi (n = 37, 16.9%), Pathan (n = 19, 8.7%), Balochi (n = 6, 2.7%), and others (n = 20, 9.1%). About (n=72, 32.9%) were employed, (n=39, 17.8%) were unemployed, (n=44, 20.1%) were retired, (n=27, 12.3%) were housewives, and (n=37, 16.9%) were students. In addition, the majority of individuals with diabetes use oral medicines (n = 117, 54.3%), insulin (n = 59, 26.9%), and diet and lifestyle changes (n = 43, 19.6%). The great majority of our participants (n = 200, 91.3%) had undergone vaccination.
Impact of COVID-19:
The health of our 124 participants (56.6%) was unaffected by COVID-19. Approximately n = 147 (67.1%) participants believe that there have been no changes in the quality of diabetic care as an outcome of COVID-19; n = 135 (61.6%) have no concerns about not receiving adequate treatment or diabetic care; and n = 123 (56.1%) have no worries about managing their diabetes if they were infected with COVID-19 with a prevalence of 0.05. Some participants were concerned about being unable to get diabetes equipment: males n = 24 (11%); females n = 33 (15.1%). They all had no trouble seeking medical attention and a consultation (p < 0.05). (Table 1).
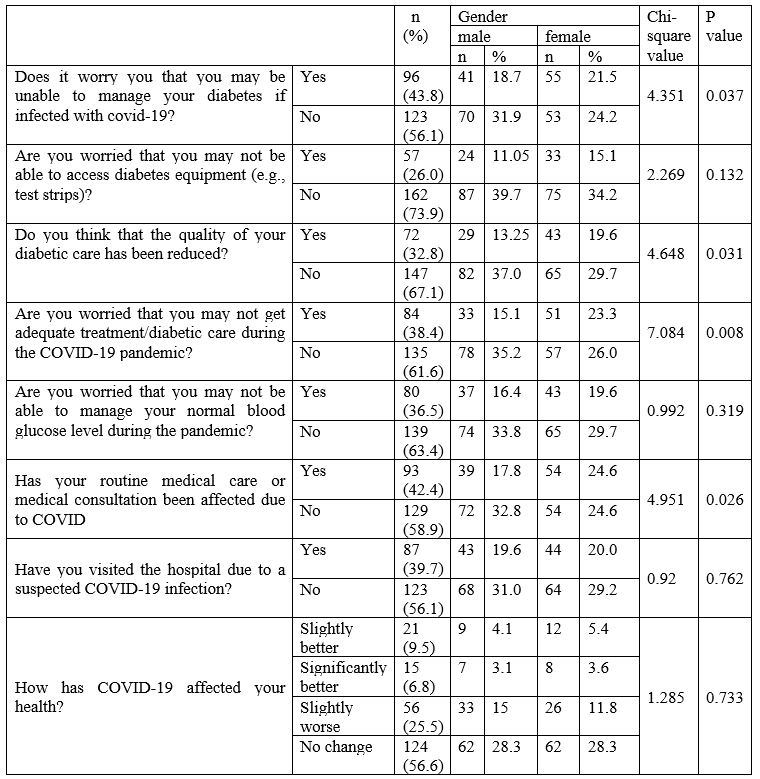
Table 1: Impact of Covid/ Diabetes Worries
Behavioural and lifestyle changes due to COVID-19:
During lockdown, behavioural and lifestyle changes in diabetic patients did not show any significant association with respect to gender. On average, 50.7% (n = 11) of participants (males n = 52, 23.7%, and females n = 58, 26.5%) were taking medicine more regularly and carefully during the COVID-19 outbreak. 72.6% (n = 159) of them were measuring their blood glucose levels less frequently than usual, although 12.3% (n = 27) checked their blood glucose level every day to keep it maintained. The physical exercise routine was less than before in 53% (n = 116) of the participants, 24.2% (n = 53) physical exercise was more during lockdown, and 22.8% (n = 50) did not alter their exercise routine. The eating habits of 31.5% (n = 69) were found to be more than before, 44.7% (n = 98) were eating less than before, and 23.7% (n = 52) eating habits were not affected at all (p = 0.04). 50 About 70.8% (n = 115) of participants received sufficient support from their family members, friends, and relatives to maintain their diabetes during the COVID-19 lockdown or quarantine, and 53.4% (n = 117) were getting sufficient care from their healthcare team (such as doctors, nurses, etc.) in the COVID-19 situation. (table 2).
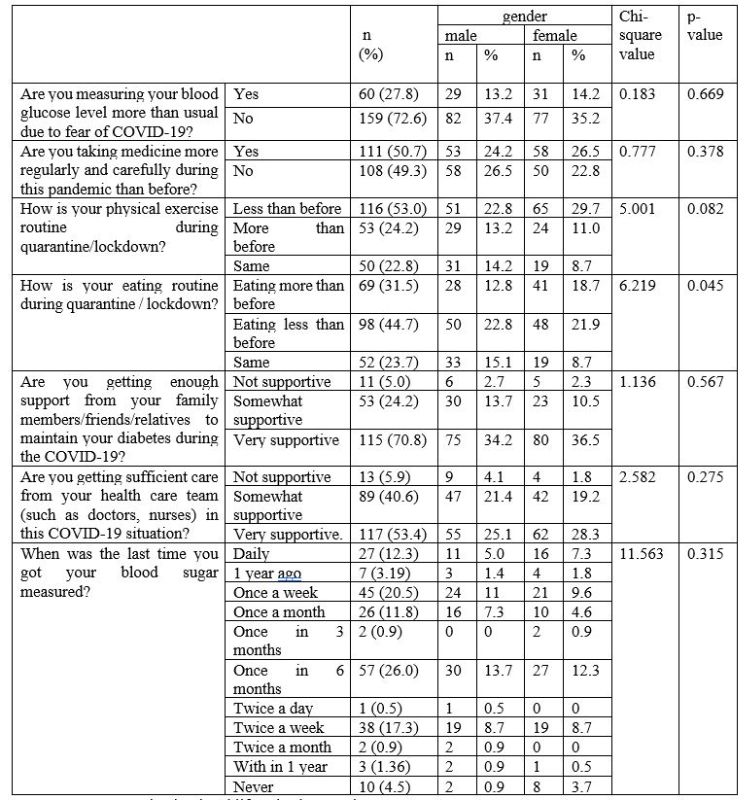
Table 2: Behavioral and lifestyle changes due to COVID 19.
Awareness of COVID-19 in diabetic patients:
For our participants, we asked two open-ended questions. Are you aware of the means of preventing COVID-19? The majority of our participants don’t know n = 40 (18.2%) any preventive measures to be taken for COVID-19; about n = 166 (76%) knew about SOPS, like wearing a mask while going out, washing hands for 20 seconds before and after using something, using sanitizer, maintaining social distancing at least 6 feet apart in public places, avoiding unnecessary social gathering, isolating ourselves if we feel any COVID symptoms, and most importantly, getting vaccinated n = 13 (5.9) with a prevalence of 0.086.
We questioned them about any other risks associated with COVID-19 in diabetes mellitus. significance of p-value < 0.0001, n = 149 (68%) said no. About n = 70 (32%) known additional risks such as kidney problems, cardiovascular disease, paralysis, foot infection and complications, eye disease, back pain, arthritis, diabetic ketoacidosis, respiratory problems, low immunity, stress, wound healing issues, infection, acute hyperglycaemia, and inflammation of skin and bone.
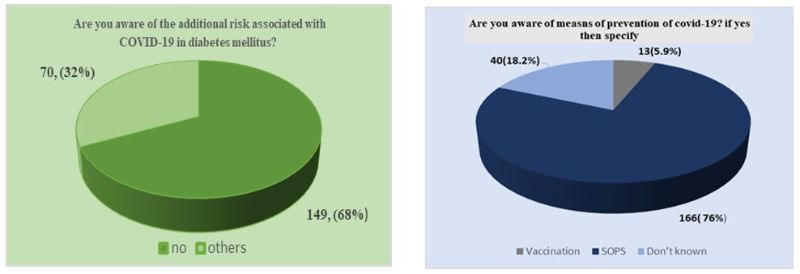
Figure 1: about 70 (32%) of our respondents were aware of additional risk associated with COVID-19 in diabetes mellitus,
Figure 02: about 13(5.9%) were vaccinated and 166 (76%) were following SOPS during COVID-19 break out.
Discussion:
Our study aimed to raise awareness of COVID-19 and how it has impacts on diabetic patients' lifestyles and behavioural changes. Because, throughout this time, the inhabitants of the country underwent changes in their daily routines in a variety of activities, including personal habits [25]. In our study, there were no particular changes felt in the participants' lifestyle and behaviour during lockdown, the main reason being that people with DM must be educated about this and take the all-necessary precautions to protect themselves [26]. The physical routine of our participants was not up-to-date during the pandemic because of their lack of mobility. As mentioned in the study by Sankar, Prasanth, et al. [27], the physical activity of individuals was expected to be limited. The participants were eating more, considering eating more is healthy, which can be related to the study, where participants' eating patterns were affected by the lockdowns [28] and [29] their appetite increased. The majority of individuals had no difficulty receiving insulin or [30] oral medications. For the majority, the frequency of measuring their blood glucose level was the same as compared to the study in which individuals mentioned elevated levels of blood glucose based on self-monitored capillary blood glucose values [31].
The majority of them had full access to diabetic care equipment, and the assistance of paramedic staff as well as family, friends, and relatives was assisting them in maintaining their diabetes and making them less concerned about adequate treatment and care.
Although people with diabetes mellitus (DM) are not at a higher risk of infection with COVID-19 compared with people in general, the presence of underlying DM presages a poor prognosis in patients with COVID-19 in terms of severe disease, ARDS, and increased mortality [32], but our participants have been aware of the additional risks associated with COVID-19 in diabetes mellitus.
The limitation of the study includes not measuring HbA1c, which is an important factor and can show a link [33], who had an “unhealthy diet pattern” and less physical activity. Not inquiring about socioeconomic situation and educational level, which can assist us in learning about COVID-19 awareness.
Despite these limitations, the results of this study suggest that maintaining good disease control and well-being is achievable despite the extensive application of techniques for infection control and lockdown [34].
Conclusion:
In conclusion, according to our findings, the COVID-19 pandemic poses a challenge for individuals with diabetes, but there is no evidence of high susceptibility to the coronavirus infection. Moreover, participants physical routines were affected, resulting in less mobility and changes in eating habits, which can be changed by working on them for a better health outcome. Most participants were vaccinated without complications. Awareness of COVID-19 complications and preventive measures was high, but some did not take precautions. It is crucial to manage diabetes effectively and prevent the spread of COVID-19