International Journal of Medical Case Reports and Medical Research
OPEN ACCESS | Volume 5 - Issue 1 - 2026
ISSN No: 2994-6905 | Journal DOI: 10.61148/2994-6905/IJMCRMR
Ahmad Reza Shahraki 1*, Reza Abaee2 and Elham Shahraki3
1General surgeon, Assistant professor, Department of surgery, Zahedan medical faculty, Zahedan University of Medical Sciences and Health Services,Zahedan, Iran.
2General Physician, Medical Faculty , Tehran, Iran.
3Associated professor of nephrology, Department of Internal medicine, Nephrologist, Ali Ibne Abitaleb Hospital, Zahedan University of medical Sciences, Zahedan , I.R. Iran.
*Corresponding Author: Ahmad Reza Shahraki, General surgeon, Assistant professor, Department of surgery, Zahedan medical faculty, Zahedan University of Medical Sciences and Health Services,Zahedan, Iran.
Received Date: January 16, 2024
Accepted Date: January 24, 2024
Published Date: January 26, 2024
Citation: Ahmad Reza Shahraki, Reza Abaee and Elham Shahraki. (2024) “Buttock wounds, and sacral fracture with normal radiolodic procedure due to stab wound in a Covoid 19 positive patient: A case report.”, International Journal of Medical Case Reports and Medical Research, 2(1); DOI: 10.61148/2994-6905/IJMCRMR/021.
Copyright: © 2024. Ahmad Reza Shahraki. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
The sacrum bone is an integral part of the spinal column and pelvic ring. The Iumbosacral neurologic function is protected by the sacrum and it maintains spinal column and pelvic alignment. For this reason, injuries to the sacrum may result in deformity, chronic pain and loss of lower extremity, bowel, bladder and sexual function. Therefore, the treatment of sacral fractures requires optimizing both neurologic and structural outcome, while also implicating a comprehensive understanding of neural decompression and skeletal reconstruction techniques.
The majority of sacral fractures occur in combination with pelvic fractures and the rest of them, representing only a small percent, occur either isolated or in combination of noncontiguous Thoracolumbar fractures. Our case was a 22 years old male with positive PCR test for covoid 19 that referred to surgery part because of stab wound on his buttock. Treatment of sacral fractures should always take into consideration associated systemic or musculoskeletal injuries, osteoporosis, the presence of brain injury, obesity, the patient’s physiological age, and past medical history. Aggressive surgical treatment may lead to surgical blood loss and hemodynamic instability, cardiopulmonary compromise, soft tissue break down, and an increased infection risk in the metabolically challenged patient. Only a multidisciplinary approach between the trauma team and subspecialists will dictate the most appropriate management for these patients, and recent data has shown that best outcomes are obtained when these fractures are cared for at level 1 trauma centers.
Background:
The sacrum bone is an integral part of the spinal column and pelvic ring. The lumbosacral neurologic function is protected by the sacrum and it maintains spinal column and pelvic alignment. For this reason, injuries to the sacrum may result in deformity, chronic pain and loss of lower extremity, bowel, bladder and sexual function. Therefore, the treatment of sacral fractures requires optimizing both neurologic and structural outcome, while also implicating a comprehensive understanding of neural decompression and skeletal reconstruction techniques [1].
The severity of sacral fracture varies from insufficiency fracture in osteoporotic patients, to complex fracture pattern, resulted from high-energy trauma, such as motor vehicle accident or fall from height [1,2,3,4,5,6].
The majority of sacral fractures occur in combination with pelvic fractures and the rest of them, representing only a small percent, occur either isolated or in combination of noncontiguous thoracolumbar fractures. The incidence of sacral fracture, accompanied by pelvic fracture, ranges from 40% to 50% [1, 6,7,8,9,10]. Because of the close relationship of the sacrum and neurologic function of lower extremity and bowel, bladder and sexual function, diagnosis and treatment of sacral fracture is very important and is very challenging [6].
According to the literature, sacral fractures, in 30% of patients with neurologic deficit and in 50% of patients with normal neurologic examination, had been missed [5,6,8,9].
Therefore, comprehensive history taking and physical examination, in combination with using diagnostic modalities and high index of suspicion of physician are mandatory for the prevention of complications, which may accompany sacral fracture, in trauma patients [5]. Behind every stab wound is a new world must be discover and explore.
Case presentation:
Our case was a 22 years old male with positive PCR test for Covoid 19 that referred to surgery part because of stab wound on his buttock

Figure1: Stab wound on buttock.
CT and graphics show normal internal organs and integrated.
sacral bone. We prepare patient for surgery that announce us that his PCR test for cocoid19 is positive, but we start the surgery.
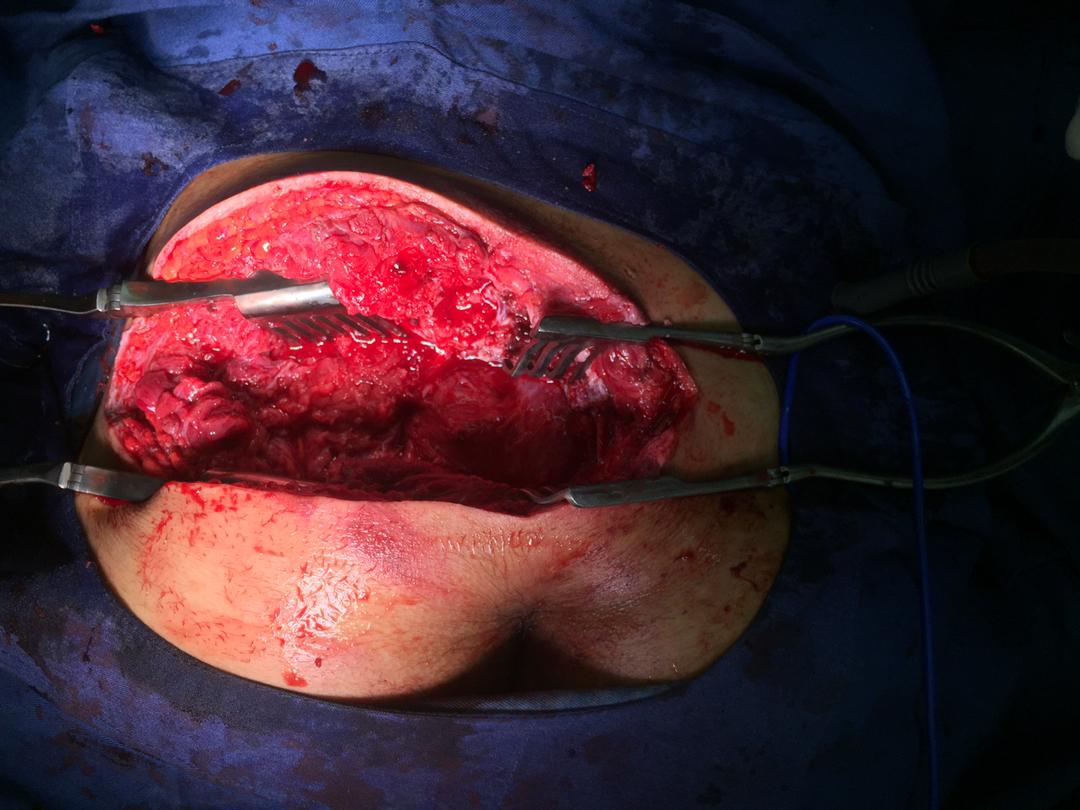
Figure 2: Exposure of injury.
We saw that with no evidence of neurologic signs his sacral bone fractured vertically.

Figure 3: Exposure of rectum.
We repair sacral with wire and covered rectum with a soft tissue flap and repair the laceration and start treatment of covoid19. After 1 months he can stand on his feet and walk with walker and we discharge him to continue physiotherapy.
Conclusion:
Sacral fractures are poorly recognized, because of difficulty in radiological evaluation and combined severe injuries, associated with these fractures [11]. The ideal treatment of sacral fracture remains unknown [7,12] Earlier studies demonstrated reasonable outcomes, with either non-operative or surgical methods. However, over the last 20 years, no constant treatment algorithm for these severe injuries has been introduced [7]. Penetrating trauma refers an injury to the soft tissues, muscle vessels, nerves, and organs in the penetrated area. It is an open injury with entrance and exit sites, usually accompanied by wounds to 1 or more tissues and organs. Because of the presence of complex anatomical structures in the injured area and the occurrence of random injuries, treatment and surgical procedures are difficult. [13].
The preoperative evaluation and imaging are crucial for dealing with penetrating wounds to the buttock. If there is no injury to large blood vessels, intestines, or the urinary system, satisfactory results can be obtained with the application surgery. [14]
Treatment of sacral fractures should always take into consideration associated systemic or musculoskeletal injuries, osteoporosis, the presence of brain injury, obesity, the patient’s physiological age, and past medical history. Aggressive surgical treatment may lead to surgical blood loss and hemodynamic instability, cardiopulmonary compromise, soft tissue breaks down, and an increased infection risk in the metabolically challenged patient. Only a multidisciplinary approach between the trauma team and subspecialists will dictate the most appropriate management for these patients, and recent data has shown that best outcomes are obtained when these fractures are cared for at level 1 trauma centers [15]. In conclusion, sacral fractures are complex and frequently overlooked [16]. Penetrating injuries to the buttock area should be treated as potentially life threatening. Algorithms exist to aid decision making and should be made available to clinicians.
►► A high index of suspicion for subtle findings should be
applied when examining radiological images for patients with
penetrating buttock trauma. The involvement of a vascular
radiologist is advised.
►► Patients re-presenting to hospital with ongoing bleeding from
buttock stab wounds should be considered for an urgent
digital subtraction angiogram with the view of embolisation [17].
Declarations:
Ethical Approval and Consent to participate:
The content of this manuscript is in accordance with the declaration of Helsinki for Ethics. No committee approval was required. Oral and written consent to participate was granted by families.
Consent for publication:
“Written informed consent was obtained from the patient's legal guardian for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.”
Availability of supporting data
It is available.
Competing interests:
The authors declare that they have no competing financial interests and nothing to disclose.
Funding: There is no funding.
Authors' contributions:
Ahmad Reza Shahraki is a surgeon of patient and writes this paper. Reza Abaee collects data and Elham Shahraki reviews the paper.
The author declares that they have no competing financial interests and nothing to disclose.
Acknowledgements
Only a multidisciplinary approach between the trauma team and subspecialists will dictate the most appropriate management for these patients, and recent data has shown that best outcomes are obtained when these fractures are cared for at level 1 trauma centers.