International Journal of Medical Case Reports and Medical Research
OPEN ACCESS | Volume 5 - Issue 1 - 2026
ISSN No: 2994-6905 | Journal DOI: 10.61148/2994-6905/IJMCRMR
Rabia Malik 1, Nazish Najeeb 2, Lal Muhammad 3, Sana Chaudhary 4, Kanza Ahmed 5 and Yasir Ahmed 6*
1Department of Internal Medicine United Health Services Hospitals, Johnson City, NY.
2Department of Internal Medicine Capital Health Medical Center Pennington NJ.
3Department of Internal Medicine United Health Services Hospitals, Johnson City, NY.
4Department of Internal Medicine United Health Services Hospitals, Johnson City, NY.
5Department of Internal Medicine United Health Services Hospitals, Johnson City, NY.
*6Faculty Internal Medicine United Health Services Hospitals, Binghamton NY.
*Corresponding Author: Yasir Ahmed. Faculty Internal Medicine United Health Services Hospitals, Binghamton NY.
Received Date: September 19, 2023
Accepted Date: September 25, 2023
Published Date: October 02, 2023
Citation: Rabia Malik, Nazish Najeeb, Lal Muhammad, Kanza Ahmed and Yasir Ahmed. (2023) “Paget’s Disease of the Bone in a Patient with Recurrent Falls. A Case Report.”, International Journal of Medical Case Reports and Medical Research, 1(2); DOI: 10.61148/2994-6905/IJMCRMR/013
Copyright: © 2023. Yasir Ahmed. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Paget's disease of the bone (PDB) is a rare metabolic bone disease that is estimated to affect 1-2% of the general population in the United States, resulting in deformity and high disability. The disease is commonly misdiagnosed due to a diverse range of signs and symptoms. This case report summarizes a case of a 75-year-old man with multiple comorbidities and history of falls, was found to have multiple old and new fractures of the spine on imaging. Incidental radiologic findings were the first clue to the diagnosis. The patient was given zoledronic acid, which improved symptoms. Difficulty in ambulation, falls and subsequent fractures can easily be attributed to frailty and comorbid conditions. This case highlights the importance of keeping PDB on the list of differentials in an elderly patient presenting with recurrent falls and fractures.
Introduction:
Paget's disease of bone (PDB) was first discovered by the British surgeon James Paget in 1876, and was termed it as “osteitis deformans” [1]. Hyperactive bone remodeling and high-speed trabecular osteolysis are seen with PBD, leading to decreased bone quality and mechanical strength [2]. The chronic bone damage caused by PDB can be monostotic or polyostotic, and almost any bone can be affected, but the pelvis, spine, femur, tibia, skull, humerus, and scapula are involved more frequently [3]. We are reporting a case of an elderly patient who had recurrent falls with fracture attributed to his comorbidities and general weakness, and was diagnosed after incidental findings on imaging.
Case presentation:
A 75-year-old male with chronic obstructive pulmonary disease (COPD), idiopathic peripheral neuropathy, history of multiple falls, and age-related dementia was seen in the emergency department for generalized weakness and failure to thrive. He reported severe foot pain, gradual decline in ambulatory status to the point where he was unable to go from his bed to the bathroom over 2-3 months. Prior to that, he used a walker to ambulate. On examination, vitals were stable, and no bone deformities were noticed but both legs below the knee were painful to touch. Laboratory workup showed an elevated serum alkaline phosphatase (ALP) level of 201 (38 – 126 U/L), and mild hypokalemia.
The patient had been admitted to the hospital several times followed by multiple short-term physical rehabilitation. On the current hospital stay, a computed topography scan (CT) scan of the lumbar and thoracic spine showed L3 age-indeterminate compression fractures and chronic appearing compression fractures of L4 and L5. Acute L3-L4 compression fracture was seen on magnetic resonance imaging (MRI) of thoracic and lumbar spine. It was actually the CT scan of the chest and abdomen with intravenous (IV) contrast that demonstrated lesions with coarse loculations, expansile-like appearance within the lumbar spine, sacrum and bony pelvis most likely related to Paget's disease. X-ray and CT head without contrast showed a pagetoid skull (figure 1 and 2). Nuclear medicine (NM) three-phase study of the bone showed findings of cortical thickening and increased cortical activity in the skull (occipital bones), the proximal humeri, the pelvis and the proximal femurs (figure 3). These findings on imaging studies along with patient’s presentation was consistent with Paget's disease. The patient received IV zoledronic acid upon the recommendation of rheumatologist. Physical and occupational therapies were continued in-house. The patient was placed in a nursing home once symptoms had improved and deemed suitable for discharge.

Figure 1: A skull radiograph showing findings of slight expansion and ground-glass appearance of the occipital bone (blue arrow) related to Paget’s disease.
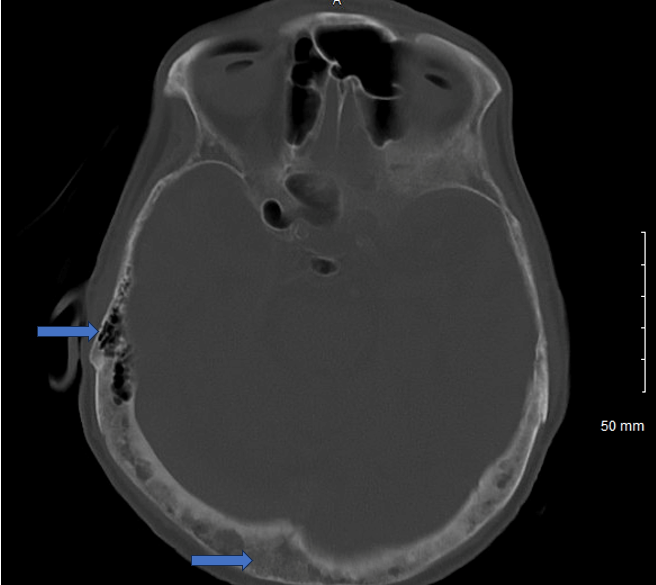
Figure 2: A CT of the head without contrast (although there was some remnant contrast from previous imaging studies) showing abnormal mineralization of the skull base and calvarium (blue arrows).
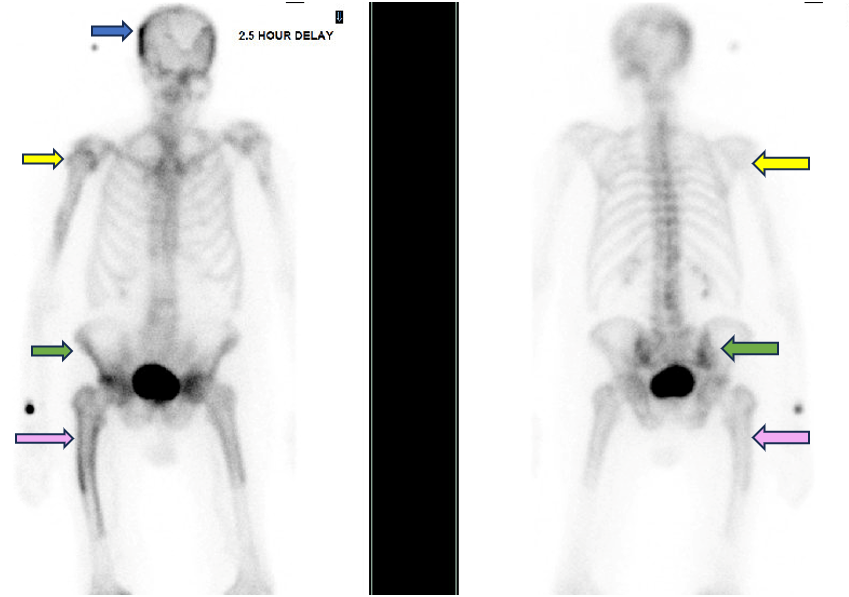
Figure 3: A radionuclide bone scan showing increased cortical thickening and abnormal uptake in the base of the skull (blue arrow), in the upper third of humerus bilaterally (yellow arrows), iliac bones on both sides (green arrows), proximal femur bilaterally (purple arrows).
Discussion:
Paget's disease (PD), also known as Paget's disease of bone, is a chronic bone disorder characterized by abnormal and excessive bone remodeling and is the most common metabolic bone disorder after osteoporosis [4]. It results in the affected bones becoming larger, weaker, and more prone to deformities. The disease is relatively uncommon, and its prevalence varies in different populations. The prevalence of Paget's disease is estimated to be around 1% in individuals over the age of 55 in the United States and Europe. However, the prevalence can be higher in specific regions, such as in the United Kingdom, where it is estimated to be around 2-3% in individuals over 55 years old [5].
There are abundant large osteoclasts found in pagetic lesion of the bone [6] that has increased receptor activator of nuclear kappa B ligand (RANKL) activity and secretion of high level of cytokines such as interleukin-6 [2]. Increased osteoclastic number and activity is followed by rapidly increased osteoblastic activity, laying down new bone structure that is disordered with abnormal architecture and sclerotic features. Despite the increased bone formation, the quality of the micro-architecture is poor [2].
Paget disease may be asymptomatic, but the common presenting symptoms are bone pain, deformity, and even fracture [7], joint stiffness, hearing loss if skull bones are involved, and neurologic symptoms if nerve compression occurs [8], and less commonly, increased cardiac output and excessive blood loss during surgery [2]. It also increases the risk of various types of fractures in the affected bones, including “chalk-stick” fractures – complete transverse fractures of the weight bearing bones [2].
An unintentional descent from a higher level to a lower level is referred to as a “fall”, often resulting in the person landing on the ground or another surface, resulting in injuries that could be fatal [9]. Falls represent a significant challenge in the elderly as it can reduce life expectancy [10] and affect morbidity, mortality, loss of functional capacity, and institutionalization [11]. Paget's disease is seldom given due consideration as a potential differential diagnosis when assessing an elderly patient for a fracture after a fall. This oversight could potentially lead to missed opportunities for early detection and appropriate management of Paget's disease in older individuals who are at risk for falls.
In the evaluation process, it is particularly important to consider the interaction and the synergism between multiple causes of falls, as the etiology is indeed multifactorial [12]. The subsequent factors might potentially amplify the likelihood of falls among those afflicted:
X-rays are usually the initial imaging modality used to assess suspected cases of Paget's disease. The features that suggest a diagnosis of PD include osteolytic areas, cortical thickening, loss of distinction between cortex and medulla, trabeculae thickening, and osteosclerosis [13]. The diagnosis of PD is considered when ALP elevation or incidental findings are noticed on X-rays. Bone-specific alkaline phosphatase (BSAP) may be considered if concomitant hepatic disease is present. Plain X-ray of the whole body – i.e., skull and facial bones, abdomen, and lower extremities – is recommended [14]. A radionuclide bone scan of the skeleton is considered the standard of care to determine any additional lesions, and general X-ray survey of the body is an acceptable alternative if radionuclide bone is not available. Further imaging with CT, MRI, and positive emission topography (PET) scan is not required unless there is a concern for complications such as compression of the spinal cord or basilar investigation [2].
The treatment of PD typically involves the use of medications to regulate bone turnover (suppress osteoclasts) and reduce bone pain. The use of bisphosphonates has not changed as the primary therapy, and the only significant randomized clinical trials in PD are with bisphosphonates. The therapy of choice is a single 5 mg dose of zoledronic acid. Zoledronic acid when compared to other bisphosphonates, have shown superiority in normalization of ALP, and suppression of bone turn over markers [15]. Although fracture reduction is one of the main goals of therapy, there is lack of strong evidence that bisphosphonates therapy prevents fractures, either at the disease-affected sites or elsewhere. Also, there are no large studies powered to ascertain event driven end-points for symptoms including osteoarthritis, joint replacement, hearing loss, blood loss during orthopedic surgery, and neoplastic transformation [2]. There is a general perception that bisphosphonates are either neutral or beneficial on these measures based on expert opinions, case reports and extrapolation of general data. In our case, an elevated ALP and incidental finding on imaging gave a clue to the diagnosis, and the patient was given IV zoledronic acid which improved symptoms. ALP can be monitored in 3 months after administration of zoledronic acid and other markers for bone turnover can also be measured [2]. The majority of the patients who respond to IV zoledronic acid do not have a relapse, as it has a long-lasting effect suppressing bone turnover for at least 5 years [16].
Conclusion:
Falls leading to fracture in the elderly can easily be attributed to weakness and deconditioning in the setting of multiple comorbidities. Significant pain, findings on physical examination and elevated ALP can be a clue to the diagnosis of PD. Early diagnosis and treatment with a single dose of IV zoledronic can improve symptoms and potentially improve future outcomes.