International Journal of Clinical Gynaecology and Obstetrics
OPEN ACCESS | Volume 3 - Issue 1 - 2025
ISSN No: 2836-0737 | Journal DOI: 10.61148/2836-0737/IJCGO
Walawe Nayaka Sanjaya
Post graduate institute of Medicine, University of Colombo, Sri Lanka.
*Corresponding Author: Walawe Nayaka Sanjaya, Post graduate institute of Medicine, University of Colombo, Sri Lanka.
Received date: October 25, 2023
Accepted date: November 06, 2023
Published date: November 10, 2023
Citation: Walawe Nayaka Sanjaya. (2023). “Large broad ligament serous cystadenoma presented with deep dyspareunia.”. International Journal of Interventional Radiology and Imaging, 1(1); DOI: 10.61148/IJIRI/005.
Copyright: © 2023 Walawe Nayaka Sanjaya. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Broad ligament is a double layered peritoneal fold which consist of various anatomical structures and cell types which gives rise to different types of lesions. Symptomatology and the ultrasonic appearance of a broad ligament cyst may be difficult to distinguish from an ovarian tumor. This is a case of serous cystadenoma of the broad ligament which presented with deep dyspareunia.
Introduction:
Broad ligament is a double layered peritoneal fold consist of mesothelial cells which drapes over the uterus and fallopian tubes. It connects uterus, fallopian tubes and ovaries with the lateral pelvic wall. The broad ligament contains smooth muscle fibers, blood vessels (uterine and ovarian vessels), uterosacral ligaments posteriorly, cardinal ligaments laterally, ovarian ligament medially and suspensory ligament of the ovary laterally, a portion of the ureters, round ligaments anteriorly and embryonic rests (such as mesonephric duct remnants, paramesonephric duct remnants, adrenocortical cell remnants and heterotopic hilar cell clusters) [1]. This can be divided into 3 parts (mesosalpinx, mesovarium and mesometrium commonly known as broad ligament).
Lesions of the broad ligament can be broadly classified as follows [2].
Fibroids are the commonest neoplasm in the broad ligament [3]. They may have originated from uterus and extended into the broad ligament or they may have originated from broad ligament without having any connection to the uterus. Very rarely this may be a part of Benign Metastasizing Leiomyoma [4]. Some times these fibroids may undergo cystic degeneration as well.
Most of the broad ligament cysts are from paramesonephric origin [5]. There may be cysts from mesonephric origin as well [2]. 10% of all adenexial cysts are broad ligament cysts [6]. These cysts may be benign, border line or malignant just like in epithelial ovarian tumors.]
Pain during and after the sexual intercourse is called dyspareunia [7]. The causes can be broadly classified as
Common causes for secondary dyspareunia in reproductive age women are endometriosis, Pelvic inflammatory disease, pelvic tumors, surgical adhesions and vulvar-vaginal lesions.
Case:
Previously healthy, 38-year old, mother of three children (delivered vaginally) presented with gradually developing dyspareunia during last six months. She didn’t have secondary dysmenorrhea and chronic pelvic pain which suggestive of endometriosis. She didn’t have any other features suggestive of pelvic inflammatory disease as well. She had regular menstrual cycles. She denied any history of vulvar-vaginal lesions and vaginal dryness. She had not undergone any abdominal surgeries. She never had cystic lesions in other organs of the body and she denied any similar family history as well.
Her abdominal examination revealed a non-tender abdomino-pelvic mass in left lower abdomen which compatible with 16 weeks size gravid uterus. Mobility of the mass was less and mild tenderness noted over the mass. Pelvic examination showed slightly deviated cervix towards the right with left adenexial tenderness. Ultra sound scan (USS) of the abdomen and pelvis showed bilocular cystic lesion measuring 15x10cm which located in left adenexia. There were no solid areas and ipsilateral ovary was not seen separately. Uterus was displaced towards right and otherwise appeared normal. Right ovary was normal and there was no free fluid in the peritoneal cavity. Her CA 125 level was 8 IU/ml. At the end of history, examination and investigation working diagnosis of “left ovarian benign tumor with possible adhesions to uterus” was made.
After careful counselling and consent taking she agreed for mini-laparotomy and cystectomy. Her mass was re examined after the general anesthesia and reduced mobility was re-confirmed. Supra-pubic transverse incision was made to enter into the peritoneal cavity which showed a large cystic left broad ligament cyst which displaced the uterus towards right. Her both tubes, ovaries and then Pouch of Douglas appear normal with out any adhesions or ascites (figure 1).
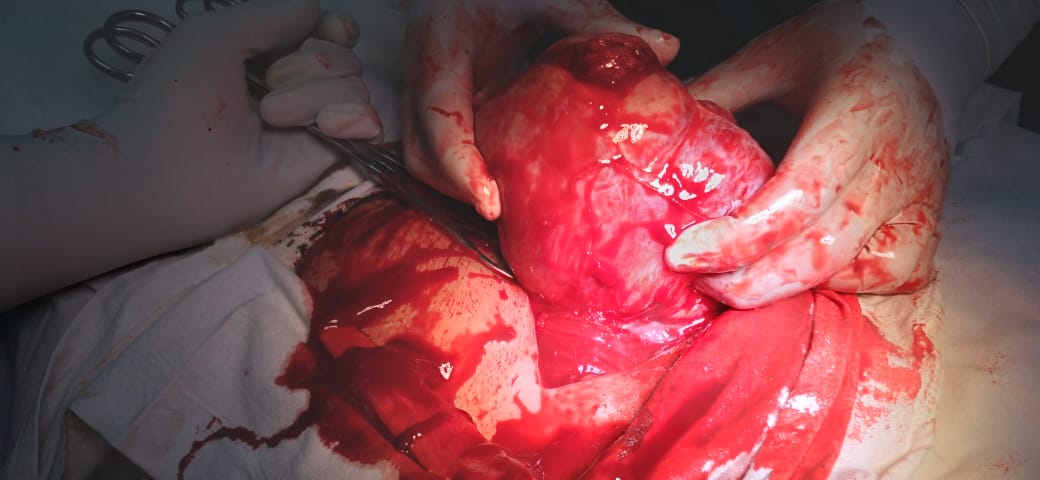
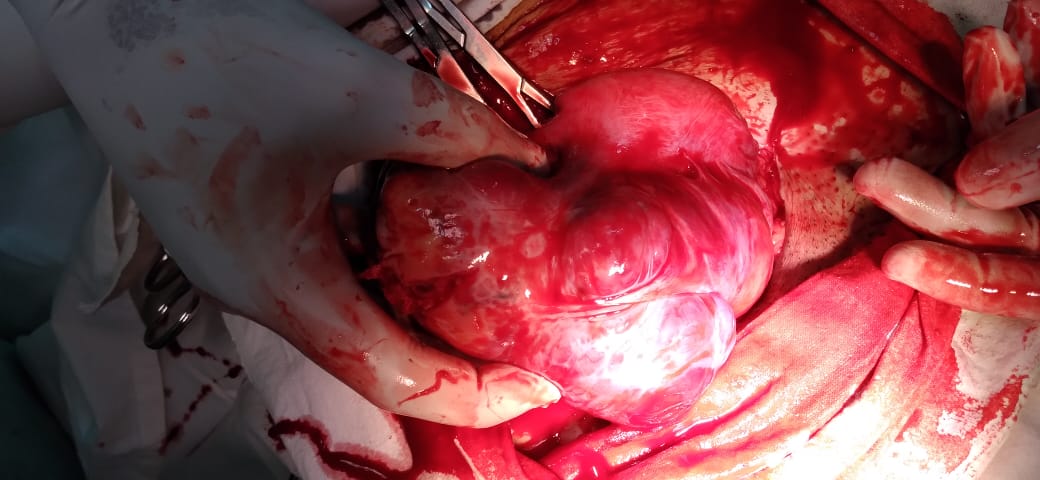
Figure 1: intra operative view of the broad ligament cyst (B) with the displaced uterus (A).
Stretched left round ligament was identified and dissected to enter into the space between two leaves of left broad ligament. Surgeons dominant hand’s fingers were inserted between broad ligament leaf and the cyst wall to enucleate the cyst. The cyst had been extended up to the deeper level of the pelvis. Careful digital enucleation of the cyst was done to prevent the damage of adjacent ureter. After the enucleation of the cyst (figure 2), oozing was noted in between the two broad ligament leaves which was managed with application of local compression for few minutes. She had an uneventful recovery. Her histology report came as serous cystadenoma of the left broad ligament.

Figure 2: left broad ligament cystadenoma after excision.
Discussion:
This patient was a previously healthy lady who didn’t have dyspareunia. So, there is a high probability of having intra abdomino-pelvic cause for the dyspareunia. Other than dyspareunia, as her history was not suggestive of having pelvic inflammatory disease or endometriosis, presence of pelvic mass should be born in physician’s mind. The mass detected during the abdominal examination was less mobile. This could be due to adhesions or due to mass in the broad ligament. Slightly deviated cervix away from the mass give a clue as well.
Best investigation to assess an adenexial cyst is ultra sound scan (USS) due to its diagnostic accuracy, availability and low cost. Both trans abdominal and trans vaginal route should be used in this patient as this lesion had come out from the pelvis into the abdomen. Due to non-visualization of the left ovary, diagnosis of left broad ligament had been missed even though it had not changed the management and patient outcome. Her risk of malignancy index (RMI) was 8. Absence of ascites, low CA 125 level, low RMI and her pre-menopausal age were directed the physician towards a benign cause. If there was a suspicious of non-epithelial ovarian tumor, another three tumor markers should be done as she is less than 40-year-old [8].
If there were any inconclusion in diagnosis, contrast enhanced computerized tomographic (CT) scan could have been done. But in this particular case there were no such requirement as there were no any high suspicion about a malignancy.
Surgical management is the best option for this kind of large lesion. The two routes of entry are laparoscopy and laparotomy. Both these methods have their own merits and demerits. Even though this is a relatively larger lesion, laparoscopic cystectomy could have been done with an expert hand in a well-developed laparoscopy center. Care should be taken to prevent the spillage of the cyst content even though it appeared benign. This can be achieved by using an endo-bag for the specimen retrieval procedure. Laparoscopy route will avoid a laparotomy which gives more post-operative pain. But laparotomy is still a good option in a low resource setting which gives a better idea of the lesion to the surgeon with both visual and tactile sensation. Same time it will reduce the possibility of spilling of the cyst content into the peritoneal cavity. Entry into the broad ligament to enucleate the cyst can be best achieved by dividing the round ligament. Sweeping movements of the surgeon’s fingers will easily enucleate the cyst if it goes in the correct tissue plane. As this method is a blind procedure, care should be taken to prevent the damage to ureter. The bleeding from the cyst bed can be easily managed with the combination of diathermy and applying local pressure. As this is a benign cyst she doesn’t need any further treatment and follow up. But if it was a papillary cystadenoma, possibility of von Hippel–Lindau disease should be excluded [9,10].
Conclusion:
Lesions of the broad ligament can be due to various reasons which need careful history, examination and investigations to come to a correct diagnosis and proper management in order to reduce the patient’s morbidity and mortality.
Declarations:
Acknowledgements: Not applicable.
Competing interest: None.
Sponsorship: None.
Funding source: None.
Ethical approval: As this is a case report which do not contain any patient identification details, ethical approval is not required.
Informed consent: Informed written consent was obtained from the patient
Author contribution: The author confirms sole responsibility for study conception and design, data collection, analysis and interpretation of results, and manuscript preparation.