International Journal of Clinical Gynaecology and Obstetrics
OPEN ACCESS | Volume 3 - Issue 1 - 2025
ISSN No: 2836-0737 | Journal DOI: 10.61148/2836-0737/IJCGO
Dereje Tegene1*, Solomon Kabtamu2
1Assistant Prophesier of Obstetrics and Gynecology, Department of Obstetrics and Gynecology, Adama Hospital Medical College, Adama, Ethiopia.
2Obstetrician and Gynecologist, Department of Obstetrics and Gynecology, Adola Wayo, General Hospital, Guji, Ethiopia.
*Corresponding Author: Dereje Tegene, Assistant Prophesier of Obstetrics and Gynecology, Department of Obstetrics and Gynecology, Adama Hospital Medical College, Adama, Ethiopia.
Received date: July 24, 2023
Accepted date: August 01, 2023
Published date: August 10, 2023
Citation: Dereje Tegene, Solomon Kabtamu. (2023). “Intra-operatively Diagnosed Spontaneous Unilateral Broad ligament Triplet Ectopic pregnancy”. International J of Clinical Gynaecology and Obstetrics, 3(1); DOI: http;//doi.org/08.2023/1.1023.
Copyright: © 2023 Dereje Tegene. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background: Broad ligament pregnancy is an infrequent and life-threatening form of abdominal ectopic pregnancy. Unilateral multiple ectopic gestations are a rare form of ectopic pregnancy and are usually associated with in vitro fertilization. The diagnosis of ectopic pregnancy in the broad ligament is often missed preoperatively and commonly diagnosed intra-operatively. Management involves exploratory laparotomy along with adnexectomy and removal of the ectopic mass.
Case presentation: This is a 25 years old Gravid -2, Para-1 (alive by vaginal delivery) lady who doesn’t recall the first day of her last normal menstrual period, but she had amenorrhea of 3 months duration, presented with lower abdominal pain of 4 days duration. She failed to conceive for the past 10 years despite having regular sexual intercourse. She had no history of infertility treatment. Up on physical examination; she was tachycardic, had pale conjunctive, and had remarkable abdominal tenderness with guarding and rigidity. Pelvic ultrasound shows; an empty uterus, and two gestational sacs beside the lower part of the uterus each of them had a fetal pool, fetal heartbeat was negative for both and fluid collection in the peritoneal cavity. Her hemoglobin was 5.1g/dl. With the assessment of; Acute abdomen secondary to ruptured twin ectopic pregnancy + severe anemia secondary to blood loss, she was taken to the operation theater. Under general anesthesia, exploratory laparotomy and right-side adnexectomy were done. Intra-operatively three gestational sacs with well-formed embryos were found. She was transfused with four units of cross-matched blood and had a smooth postoperative course.
Conclusion: Spontaneous unilateral broad ligament triplet ectopic pregnancy is a very rare form of ectopic pregnancy. The rarity of the case and nonspecific clinical manifestation made a preoperative diagnosis difficulty, which may increase the rate of complications. A high index of suspicion is needed for earlier diagnosis and intervention.
Introduction:
Pregnancy in the broad ligament is rarest form of abdominal ectopic pregnancy [1]. Broad ligament ectopic pregnancy occurs either due to intra-abdominal fertilization of sperm and ovum, with primary implantation of the zygote on the broad ligament or occurs as a result of early tubal abortion or rupture with secondary implantation of the pregnancy into the broad ligament [2]. Unilateral multiple ectopic gestations are infrequent form of ectopic pregnancy, and commonly associated with in vitro fertilization [3-5]. Unilateral twin ectopic gestation occurs in about 1 in 200 ectopic gestations, and unilateral triplet ectopic gestation is even more rare [6]. Like abdominal ectopic pregnancy on the other sites, diagnosis of ectopic pregnancy in the broad ligament is challenging, since it has nonspecific sign and symptoms. The diagnosis is often missed preoperatively and commonly diagnosed intra-operatively [7]. Abdominal pain is a common clinical presentation. Ultrasound is helpful to reach to the diagnosis. In a patient with ruptured broad ligament ectopic pregnancy, emergency exploratory laparotomy with adnexectomy is mandatory [7].
We reported a case of intra- operatively diagnosed, broad ligament triplet ectopic pregnancy in a 25 years old Gravida -2, Para-1 lady who was presented with lower abdominal pain of 4 days duration. It emphasizes the rare occurrence of spontaneous broad ligament triplet ectopic pregnancy and its diagnostic challenge. She was managed by exploratory laparotomy plus adnexectomy. Relevant literatures were also reviewed.
Case presentation:
This is a 25 years old Gravida -2, Para-1 (alive by vaginal delivery) lady who doesn’t recall her first day of last normal menstrual period (LNMP), but she had amenorrhea of 3 months duration. Her menses was regular and she was not on contraceptive. Her current pregnancy was confirmed by urine pregnancy test, two months back at health center. Since there was no ultrasound service at that health center, she had no ultrasound scanning. Since 4 days she started to have continuous lower abdominal pain. For the above compliant she was taken to primary hospital, from where she was referred to our hospital with the diagnosis of missed abortion after ultrasound scanning. Her abdominal pain was associated with palpitation, easy fatigability, nausea, and vomiting. She has no vaginal bleeding. She failed to conceive for the past 10 years despite having regular sexual intercourse, but she didn’t receive any treatment for that and the current pregnancy was spontaneous. She had previous history of treatment for pelvic infection. She had no history of exposure to ovulation induction drugs or use of assisted reproductive technology. She had no previous history of gynecologic procedures. She had no history of chronic medical or surgical illnesses. The pregnancy was planned, wanted, and supported.
Up on physical examination; she was acutely seek looking and in pain, her vital signs were; Blood Pressure=90/60 mmHg, Pulse Rate=120bpm, Respiratory Rate =26 breath per minute, and Temperature = afebrile to touch. She had pale conjunctive and non-icteric sclera. The chest was clear and resonant. S1 and S2 well heard, had S3 gallop, but no murmur. On Abdomen: the abdomen was distended and moves with respiration, signs of fluid collection were postive; there was a remarkable abdominal tenderness with guarding and rigidity. Genito-urinary system (GUS) – she had normal external female genitalia, she had no active vaginal bleeding, the cervix was closed, there was cervical motion and adnexal tenderness, and the cul-de-sac was bulged. She was investigated with pelvic ultrasound and shows; the uterus was empty and normal in size measuring 8cm*11cm, there was two gestational sacs beside the lower part of uterus each of them had a fetal pool, fetal heart beat was negative for both, and crown rump length was 10+2 weeks and 11 +1 weeks. In addition there was fluid collection within the pelvic peritoneum on ultrasound (figure-1a and 1b). Her laboratory investigation reveals: White blood cell = 10,000 /mm3; Hemoglobin = 5.1 g/dl; Platelet count = 240 x 103 /ml. Blood group and Rh = AB +.

Figure 1a

Figure 1b
Figure 1a and 1b: Pelvic ultrasound showing empty uterus and two gestational sacs beside the lower part of the uterus.
With the assessment of; Acute abdomen secondary to ruptured twin ectopic pregnancy + severe anemia secondary to acute blood loss. The plan was to inform the women and prepare her for emergency laparotomy. After informed written consent was taken from the patient and four units of cross matched blood were prepared, the patient was taken to the operation theater. Under general anesthesia the abdomen was entered through the midline incision. Intra-operative findings were: there was a significant hemo-peritoneum, there was adhesion between the uterus, bowel, and adnexal mass, after releasing the adhesion we identified an intact, non-gravid sized uterus, bilateral fallopian tube and ovary. There was adnexal mass with active bleeding and up on dissection of adnexal mass, there was three gestational sacs with well-formed embryo was taken out (figure-2a and 2b).
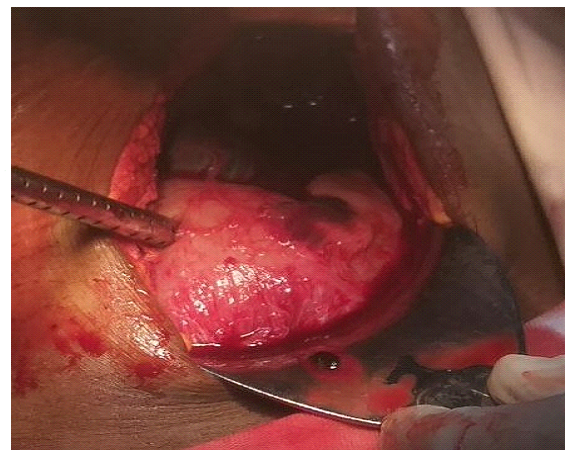
Figure 2a

Figure 2b
Figure 2a and 2b: Intra-operative findings showing empty uterus, and three well-formed embryo taken from gestational sac in the broad ligament.
What was done was; around 2500ml of hemo-peritoneum was sucked out and after trans-peritoneal identification the ureter, right side adnexectomy was done. The patient was transferred to the ward with stable vital sign and post-operative orders. Post-operatively the patient was on maintenance fluid, parenteral antibiotics and standing dose of analgesia. She was transfused with a total of 4 unit of cross matched blood. She had smooth post-operative course and her post-op hemoglobin was 9.6g/dl. She was discharged on her 3rd post-operative day with therapeutic dose of ferrous fumerate and appointed after 1 week. She was seen at outpatient clinic and she had no new compliant.
Ectopic pregnancy is defined implantation of a fertilized ovum outside the endometrial cavity [8]. It occurs in 2% of all spontaneous pregnancies [9]. About 95% of extrauterine implantations occur in the fallopian tube and less often ectopic implantations occurs in the ovary, the cervix, and the peritoneal cavity [8]. Ectopic pregnancy is the leading cause of maternal mortality in the first trimester of pregnancy and is responsible for about 4 % of all pregnancy-related deaths [10].
Broad ligament pregnancy is also called intera-ligamentous pregnancy, which is infrequent and life-threatening form of abdominal ectopic pregnancy, this is mainly because of increased risk of massive hemorrhage [1]. The anatomic location of the broad ligament is close to the major pelvic vessels, ureter and bowel, so ectopic implantation of the pregnancy can lead to massive hemorrhage and increased risk of injury to the adjacent structures, which in turn increases the maternal morbidity and mortality [7]. Risk factors for abdominal pregnancy are similar to those for tubal ectopic pregnancy which includes, previous history of ectopic pregnancy, pelvic inflammatory disease, tubal surgery, history of infertility, multiparity, use of assisted reproductive technologies and endometriosis [11]. Multiparity, previous history of infertility and pelvic inflammatory disease were identified risk factors for ectopic pregnancy in our index case.
Broad ligament ectopic pregnancy occurs either due to intra-abdominal fertilization of sperm and ovum, with primary implantation of the zygote on the broad ligament or occurs as a result of early tubal abortion or rupture with secondary implantation of the pregnancy into the broad ligament [2]. Broad ligament pregnancy can also develop if there is a fistula formation between the endometrial cavity and the leaves of the broad ligament due to various reasons. In addition weakness and separation in a prior cesarean scar or a uterine perforation after an abortion can also result in secondary broad ligament implantation [12,13]. We didn’t identify any risk factors that cause weakness and separation of uterine myometrium in the index case. She had no previous history of gynecologic procedures.
Unilateral multiple ectopic gestations are rare form of ectopic pregnancy, and commonly associated with in vitro fertilization [3-5]. Unilateral twin ectopic gestation occurs in about 1 in 200 ectopic gestations, and unilateral triplet ectopic gestation is even more rare [6]. Although very rare, unilateral interstitial triplet ectopic gestation has been reported by Berkes, et al. in a 26-year-old infertile woman with a history of right salpingectomy and hyperprolactinemia following in vitro fertilization and embryo transfer [14]. Spontaneous unilateral triplet interstitial ectopic gestation was reported by Oriji .P.C, et al, in 41 years old gravida -9 mother who was presented with abdominal pain and managed with cornual wedge resection [6]. Two cases of tubal triplet ectopic pregnancy were also reported literature by Sanger’s and Krusen [15]. Intra-operatively we found, three gestational sacs with well-formed embryo from a broad ligament mass, which is suggestive of unilateral broad ligament triplet ectopic pregnancy.
The diagnosis of broad ligament ectopic pregnancy is often missed preoperatively because of the rarity of the case and its nonspecific clinical manifestation and commonly diagnosed intraoperatively [7]. Dull lower abdominal pain due to the placental separation, tearing of broad ligament and small peritoneal haemorrhage during early gestation is a common clinical presentation of a women with broad ligament ectopic pregnancy [16]. Vaginal bleeding due to breakdown of decidual casts is also a common feature reported in up to half of the patients [17]. In general the diagnosis of ectopic gestation requires a high index of suspicion based on risk factors, clinical presentation, and a positive pregnancy test [18]. Our patient had amenorrhea of 3 months and lower abdominal pain associated with sign and symptoms of anemia; otherwise she had no vaginal bleeding. In general the diagnosis of ectopic pregnancy was not suspected at the primary hospital, despite having clinical triads of ectopic pregnancy (amenorrhea, abdominal pain and vaginal bleeding).
Ultrasound is the first line imaging modality used to evaluate a patients suspected to have ectopic pregnancy. Strongly suggestive ultrasound features of broad ligament ectopic pregnancy were; the presence of an empty uterus and ectopic gestational sac beside the lower part of the uterus [19]. The ultrasound finding of our index case goes with broad ligament pregnancy, which includes empty uterus and gestational sac on the lower aspect of the uterus, but the triplet was missed on ultrasound. Magnetic resonance imaging (MRI) provides additional information to confirm the diagnosis and may also help in surgical planning by distinguishing anatomic relationships and potential vascular connections with the surrounding structures [19].
The management options for patients with ectopic pregnancy were expectant management, medical management, and surgical managements [6]. The choice of one option from the other depends on whether the ectopic pregnancy is ruptured or unruptured, clinical condition of the patient, site of the ectopic pregnancy, the fertility desire of the patient and availability of management option in the facility [6]. Patients with broad ligament pregnancies should be counseled preoperatively regarding the increased morbidity associated with the proximity of the pregnancy to the pelvic sidewall and pelvic anatomic structures. The ureters traverse the broad ligament and there might be a need for the repair or removal of the organs damaged by the vascular invasion [7].
If the patients are hemodynamically unstable in case of ruptured broad ligament ectopic pregnancy, emergency exploratory laparotomy to control bleeding is mandatory. The surgical management reported on different literatures involves adnexectomy after trans-peritoneal identification of the ureteral path with the removal of broad ligament ectopic pregnancy. Two cases of broad ligament ectopic pregnancy reported by Sharma el, al, was managed by laparotomy with excision of the mass along with salpingo-opherectomy [2]. Laparoscopy is reserved for stable patients with unruptured and small broad ligament ectopic pregnancy [7]. Conservative management or medical management is not recommended for broad ligament ectopic pregnancy if the diagnosis is certain (2). Since our patient had acute abdomen and sign and symptoms of intra-abdominal bleeding, emergency exploratory laparotomy along with right side adnexectomy was done.
This is a broad ligament triplet ectopic pregnancy in 25 years old Gravida-2, Para-1 woman who conceived spontaneously after 10 years of infertility. It is a rare form of extra-uterine pregnancy. The rarity of the case contributes for delay in the diagnosis, which increase the risk of rupture leading to massive hemorrhage. High index of suspicion is needed for earlier diagnosis and intervention. Emergency exploratory laparotomy to control the bleeding along with adnexectomy is recommended for a patient with ruptured broad ligament pregnancy.
Ethical approval and consent to participate:
Informed written consent to participate in this case report was obtained from the patient. Ethical clearance was obtained from the Institutional Ethics Review Board of Adama Hospital Medical College.
Consent for publication:
Informed written consent was taken from the patient for the publication the case and accompanying images.
Availability of data and materials:
The data used to prepare this case report can be obtained from the corresponding author with formal request. The submitted manuscript contains all data set used in the preparation of the document.
Competing interests:
Both authors declare that they have no competing interests.
Funding:
Not applicable.
Authors’ contributions:
Conceptualization and initiation of writing this case report was made by the corresponding author. DT and SK were involved in the diagnosis, management and follow up of the patient. On the preparation of the document both authors were involved in the literature review and critically reviewing the article. Both authors read and gave final approval of the submitted manuscript.
Acknowledgements:
Not applicable.