International Journal of Clinical Gynaecology and Obstetrics
OPEN ACCESS | Volume 3 - Issue 1 - 2025
ISSN No: 2836-0737 | Journal DOI: 10.61148/2836-0737/IJCGO
José Fernando De Los Ríos1, Claudia Cristina López1, Carolina Cifuentes1, Sandra Milena Gómez2*, Andrea Arias3, José Bareño4.
1 Department of Gynecologic Endoscopy, Clínica del Prado, Medellín, Colombia.
2 Fellow in Minimally Invasive Gynecologic Surgery AAGL-Colombia.
3 Department of Gynecology, CES University, Medellín, Colombia.
4 Department of Epidemiology, CES University, Medellín, Colombia.
*Corresponding author: Sandra Milena Gómez, Fellow in Minimally Invasive Gynecologic Surgery AAGL-Colombia
Received: March14, 2021
Accepted: March 22, 2021
Published: March 24, 2021
Citation: José Fernando De Los Ríos, Claudia Cristina López, Carolina Cifuentes, Sandra Milena Gómez, Andrea Arias, José Bareño. “What Matters Most To Women Undergoing Hysterectomy?”. International Journal of Clinical Gynaecology and Obstetrics, 2(1); DOI: http;//doi.org/03.2021/1.10010.
Copyright: © 2021 Sandra Milena Gómez. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
Study objective: to gain an understanding of patient preferences regarding choice of surgical approach to hysterectomy.
Design: Cross-sectional, analytical study.
Setting: Tertiary hospital, referral center for gynecologic surgery in Medellin, Colombia
Patients: A total of 300 women, 150 who were scheduled for hysterectomy and 150 women who were not undergoing any surgical procedure.
Interventions: A questionnaire listing advantages of laparoscopic, vaginal, and abdominal hysterectomy was designed and applied to all participating women, who were then asked to rank in order of relevance the surveyed items. Answers and demographic variables were collected.
Measurements and Main results: Average scores were calculated for each of the listed variables, and the difference of medians between groups (women scheduled to undergo hysterectomy and women who were not undergoing surgery) was analyzed. Difference of medians was also analyzed by grouping participants based on educational level. Participating women ranked as most important: safety, pain, duration of sick leave, scars, operative time, duration of surgical training, and cost. Altogether, women preferred advantages offered by laparoscopic hysterectomy over those provided by vaginal or abdominal approaches.
Conclusion: Patient preferences should be taken into account upon deciding the surgical approach to hysterectomy, as they may differ from those of the physician.
INTRODUCTION
Hysterectomy is the most frequently performed gynecologic surgery worldwide (1). In the United States, approximately 450,000 hysterectomies are performed annually (2). Currently, surgical approaches to hysterectomy include laparoscopic, vaginal, and abdominal routes. Advantages and disadvantages of each of these techniques have been analyzed in meta-analysis and systematic reviews (3-7).
Based on those reviews, scientific societies have issued guidelines and recommendations in order to choose the appropriate surgical approach for each patient (8,9). While the most recent recommendations by the American College of Obstetricians and Gynecologists (ACOG) emphasize that the choice of surgical approach to hysterectomy should take into account the patient, her values and preferences, the final decision may be biased by the surgeon’s preferences (10).
For instance, the Entwistle study showed that less than half of women undergoing hysterectomy had been informed of the advantages and disadvantages of the different types of hysterectomies, and 26% to 65% considered that they had been given little information about the procedure. (11) Strikingly, one in every 5 patients underwent surgery not knowing the type of surgical approach (12). The Skea study, 76% of patients attending the medical appointment to schedule their hysterectomy expected a shared decision-making regarding the surgical approach (13)
Currently, few studies have reported on patient preferences regarding surgical approach to hysterectomy (14). Therefore, this study was designed to identify variables that women perceive as being most important when it comes to deciding type of surgical approach to hysterectomy, and thus identify the technique that best accommodates to their preferences.
MATERIALS AND METHODS
This was an analytical cross-sectional study of 150 women undergoing hysterectomy, and 150 women who were not undergoing surgery between July 2016 and July 2017 at Clinica del Prado Medellin, Colombia. Data were collected by applying the questionnaire designed by the authors, and described below.
Questionnaire elaboration
Demographic data were collected, which included ID number, address, age, parity, and educational level. After performing a literature search and review of surgical approaches to hysterectomy, a three-part instrument was developed (Supplementary annex 1).
In the first question, patients were asked to rank according to their preferences from most to least important a total of 12 characteristics of hysterectomy, being 1 the most important and 12 the least relevant issue in their opinion. These characteristics were chosen based on the reviewed literature, and consisted of 6 advantages of laparoscopic over abdominal hysterectomy (AH), and 6 advantages of abdominal over laparoscopic hysterectomy (LH), as listed below:
Advantages of laparoscopic over abdominal hysterectomy:
1. Lower complication rates (7)
2. Faster return to daily activities (3)
3. Less postoperative pain (3)
4. Smaller scar area (15)
5. Shorter hospital stay (3)
6. Complete visualization of the abdominal cavity (16)
Advantages of abdominal over laparoscopic hysterectomy:
1. Shorter operative times (3)
2. Most commonly used technique worldwide (1)
3. Most available technique at all levels of care (17)
4. Steeper learning curve for surgeons (18)
5. Lower cost (3)
6. Does not necessarily require general anesthesia (19)
Similarly, the second question of the instrument was designed by listing 10 statements, 5 of which were the advantages of vaginal hysterectomy (VH) when compared with laparoscopic hysterectomy (LH), and 5 items stating the advantages of LH over VH as listed below:
Advantages of VH over LH:
1. Lower cost (3)
2. No visible scars (15)
3. Shorter operative time (3)
4. Less training time for surgeons (20)
5. Does not necessarily require general anesthesia (21)
Advantages of LH over VH
1. Less pain (6)
2. Shorter hospital stay (6, 22)
3. Less bleeding (23)
4. Faster return to daily activities
5. Complete visualization of the abdominopelvic cavity (5)
Once again, study participants were asked to rank according to their preferences from most to least important these 10 statements, being 1 the most important and 10 the least relevant issue in their opinion.
A similar methodology was used for the third question of the survey, in which the listed items were selected by the authors as being the most relevant, independently of the surgical technique they represented:
1. Pain
2. Recovery time
3. Safe surgery
4. Cost of procedure
5. Number and size of scars
6. Operative time
7. Duration of surgical training required to safely perform procedure
As above, participants were asked to rank from most to least important all items, being 1 the most important and 7 the least relevant issue in their opinion.
Sample size
A total sample size of 300 women was achieved by convenience sampling, and consisted of a group of 150 women that attended our institution to schedule their hysterectomy, and another group of 150 women who were were not undergoing any procedure. The latter was included as we were interested in determining whether the imminence of the procedure would affect patients’ preferences regarding hysterectomy.
Data collection
Data were collected by one of the authors, who by means of personal interview approached patients, explained the study’s objective, obtained informed consent to participate, explained the three sections of the instrument, and directly filled out the questionnaires in order to avoid participant cognitive bias, and ensuring the correct completion of each section. Data were collected and organized in an Excel spreadsheet, Scoring of questionnaires
A scoring system that allowed ordinal and numerical ranking of each of the tested items in each of the sections was generated using the following formula:
Score = (N+1) – X
Where N is the number of statements in a given section, and X is the rank given by the patient to the corresponding item. In this way, the statement rated by the participant as most important will have the highest score in its section (according to the number of statements in each section), and the item ranked as least important will have the lowest score.
To determine the order of importance obtained by each item in each section, the average score was used, which was obtained by adding all the points and dividing it by 300 (total number of questionnaires).
Data analysis
Data analysis was performed in two phases; a descriptive and an analytical phase. In the former, qualitative variables were classified and represented as absolute frequency (n) and percentages (%), while quantitative variables were represented by measures of central tendency and dispersion.
During the analytical phase, statistical significance of the association between dependent variables (imminent hysterectomy and educational level) and independent variables was determined, as well as the quantitative difference into a qualitative dichotomic, i.e. median difference between groups. A p-value < 0.05 was considered as statistically significant.
RESULTS
A total of 300 women participated in this study. Of those, 150 were patients that presented at our institution during an administrative or a medical appointment (admission, preoperative evaluation for gynecologic surgery, or preoperative preparation) prior to undergoing scheduled hysterectomy. The remaining 150 participants were women that were approached and interviewed at our institution (companion or passerby), agreed to participate, and were not undergoing a surgical procedure. All interviews were included in the analysis. Demographic data of study participants are shown in Table 1 (Sociodemographic characteristics of the study population ).
|
Variable |
N=300 AF (%) |
|
AGE years. average (range) |
40 (16-68) |
|
EDUCATIONAL LEVEL n (%) |
|
|
53 (17.7) 119 (39.6) 68 (22.6) 47 (15.7) 13 (4.3) |
|
NUMBER OF CHILDREN |
|
|
2.0 (1 -3) 0 - 8 |
AF: absolute frequency; IQR: interquartile range
Table 1. Sociodemographic characteristics of the study population
In the first section of the interview, participants ranked -based on their preferences- from most to least important 12 items; 6 considered as advantages of AH, and 6 items considered as advantages of LH. As shown in Figure 1 (Advantages of abdominal and laparoscopic hysterectomy ranked and scored by all participants ), the three most relevant variables for all interviewed participants were: experiencing less pain, lower complication rate, and use of a surgical technique that allows proper visualization of the abdominopelvic cavity. On the other hand, the least important items were: required training time for surgeons to safely perform a given technique, cost of procedure, and the fact that the procedure could be performed using conductive anesthesia.
In the second section of the questionnaire, a total of 10 items –5 advantages of LH, and 5 of VH- were ranked by each participant. As shown in Figure 2 (Advantages of vaginal and laparoscopic hysterectomy ranked and scored by all participants), the three most relevant items for all interviewed women were: less pain, less bleeding, and proper visualization of the abdominopelvic cavity during the procedure. On the other hand, the least important items were: less training time for surgeons, cost of procedure, and that the technique does not necessarily require general anesthesia.
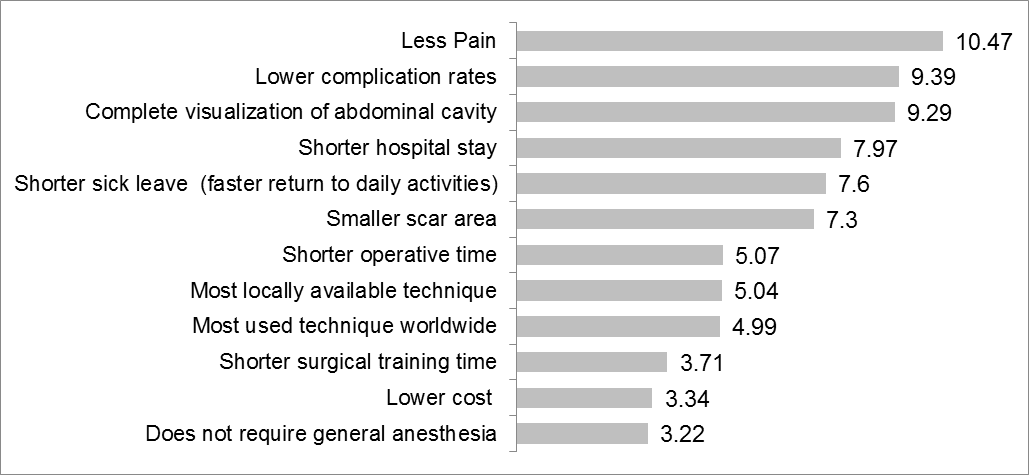
Figure 1. Advantages of abdominal and laparoscopic hysterectomy ranked and scored by all participants (question 1)
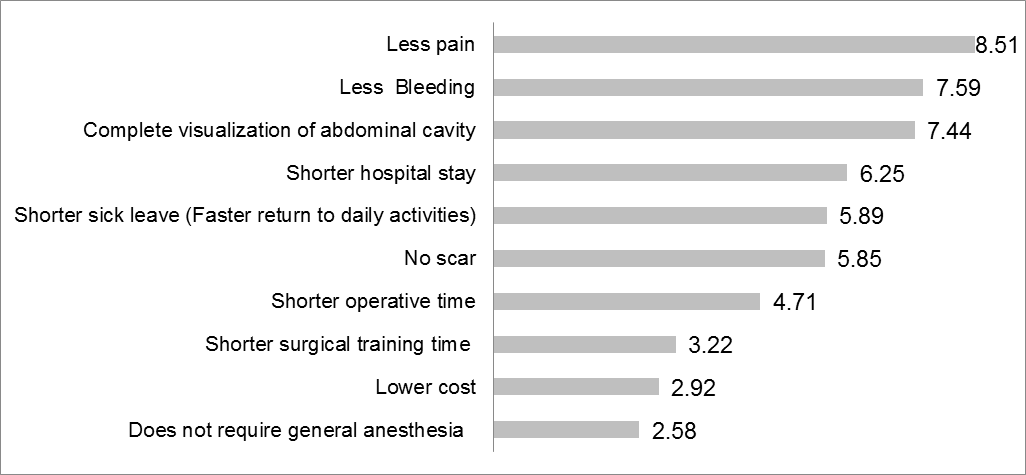
Figure 2. Advantages of vaginal and laparoscopic hysterectomy ranked and scored by all participants (question 2)
Results of the third question of our survey, which listed 7 items that were selected by the authors as being the most relevant, independently of the surgical technique they represented, are shown in Figure 3 (Most relevant factors, selected by physicians, ranked and scored by all participants).
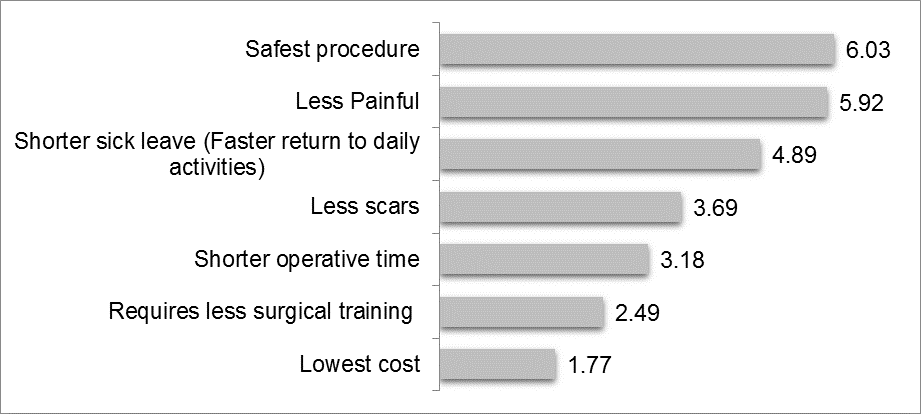
Figure 3. Most relevant factors, selected by physicians, ranked and scored by all participants (question 3)
Data collected from the group of women undergoing hysterectomy (n=150) were analyzed and compared with those from the control group – women who were not undergoing any surgical procedure ( Table 2.Comparison of scores according to imminence of hysterectomy). A median test showed a statistically significant difference (p < .05) in age of participants between groups. Participants scheduled to undergo hysterectomy were older, with a mean age of 43 years (SD 6.9), while participants of the control group exhibited a mean age of 35 years (SD 10.2). For the younger group, the size of the scar was ranked as the most important item in question 1 (p = .002) and question 3 (p = .01). On the other hand, for patients undergoing hysterectomy the fact that the abdominopelvic cavity could be properly visualized during the procedure was ranked as most important (p=.008).
|
VARIABLE |
Imminent hysterectomy |
p-value |
||
|
YES (n=150) Median (IQR) |
NO (n=150) Median (IQR) |
|
||
|
Age in years average (SD) |
43,91 (6,95) |
35,25 (10,22) |
0,0001 |
|
|
Number of children (median (IQR) |
2 (2) |
1,55 (2) |
|
|
|
Question 1 (Advantages of AH and LH) |
||||
|
Less pain |
11 (2) |
11 (2) |
0,952 |
|
|
Lower complication rates |
10 (3) |
10 (3) |
0,407 |
|
|
Complete visualization of abdominal cavity |
10 (4) |
9 (4) |
0,008* |
|
|
Shorter hospital stay |
9 (2) |
8 (3) |
0,685 |
|
|
Shorter sick leave (Faster return to daily activities) |
8 (4) |
8 (3) |
0,604 |
|
|
Smaller scar area |
7 (5) |
9 (4) |
0,002* |
|
|
Shorter operative time |
6 (3) |
5,50 (4) |
0,817 |
|
|
Most locally available technique |
5 (3) |
5 (2) |
0,544 |
|
|
Most used worldwide |
5 (2) |
5 (2) |
0,533 |
|
|
Shorter surgical training time |
3 (3) |
3 (3) |
0,474 |
|
|
Lower cost |
3 (3) |
3 (2) |
0,452 |
|
|
Does not require general anesthesia |
2 (4) |
2 (3) |
0,208 |
|
|
Question 2 (Advantages of VH and LH) |
||||
|
Less pain |
9 (2) |
9 (2) |
0,881 |
|
|
Less bleeding |
8 (3) |
8 (3) |
0.458 |
|
|
Complete visualization of abdominal cavity |
7 (4) |
8 (4) |
0.186 |
|
|
Shorter hospital stay |
7 (3) |
6,50 (3) |
0,936 |
|
|
No scar |
6 (4) |
6,50 (4) |
0,061 |
|
|
Shorter sick leave (Faster return to daily activities) |
6 (4) |
6 (2) |
0.903 |
|
|
Shorter operative time |
5 (3) |
4 (2) |
0,809 |
|
|
Lower costs |
3 (3) |
2 (3) |
0,573 |
|
|
Shorter surgical training time |
3 (2) |
3 (2) |
0,715 |
|
|
Does not require general anesthesia |
2 (2) |
2 (2) |
0,254 |
|
|
Question 3 (most relevant features selected by physicians) |
||||
|
Safest procedure |
6 (2) |
6,50 (2) |
0,643 |
|
|
Less painful procedure |
6 (2) |
6 (2) |
0,825 |
|
|
Shorter disability |
5 (2) |
5 (2) |
0,06 |
|
|
Less scars |
3,50 (2) |
4 (2) |
0,01* |
|
|
Sorter operative time |
3 (1) |
3 (2) |
0,355 |
|
|
Requires less surgical training |
2 (2) |
2 (2) |
0,657 |
|
|
Lowest cost |
1 (1) |
1 (1) |
0,255 |
|
Table 2. Comparison of scores according to imminence of hysterectomy
SD: Standard deviation; IQR: interquartile range
Participants were grouped by educational level into two groups: secondary education or below, and those with technical education or above (Table 3 . Comparison of scores according to participant educational level ). Our results show that, when comparing AH with LH, women with higher education ranked as most important a technique that resulted in lower complication rates (p=.006), while participants with lower educational level ranked as most important a faster return to daily activities (shorter sick leave) (p=.045), a lower cost (p=.037), and being the most available technique at all levels of care (p=.001).
Regarding advantages of VH and LH, our results show that for women with lower educational level the lower cost of the procedure (p=.026) was the most important item.
|
Variable |
Educational level |
p-value |
|
|
Secondary or lower (n=172) Median (IQR) |
Technical or higher (n=128) Median (IQR) |
||
|
Variable |
|||
|
Question 1 (Advantages of AH and LH) |
|||
|
Less pain |
11 (2) |
11 (2) |
0.230 |
|
Lower complication rates |
10 (3) |
11 (4) |
0.006* |
|
Complete visualization of abdominal cavity |
10 (4) |
10 (4) |
0.290 |
|
Shorter hospital stay |
9 (3) |
8 (2) |
0.778 |
|
Shorter sick leave |
8 (4) |
8(3) |
0.045* |
|
Smaller scar area |
8 (6) |
8 (4) |
0.344 |
|
Shorter operative time |
5 (3) |
6(4) |
0.117 |
|
Most locally available technique |
5 (3) |
4 (3) |
0.0001* |
|
Most used worldwide |
5 (3) |
5(2) |
0.504 |
|
Shorter surgical training time |
3 (3) |
3 (3) |
0.069 |
|
Lower cost |
3 (3) |
2 (3) |
0.037* |
|
Does not require general anesthesia |
2 (3) |
3 (3) |
0.007* |
|
Question 2 (advantages of VH and LH) |
|||
|
Less pain |
9 (2) |
9 (2) |
0.855 |
|
Less bleeding |
8 (3) |
8 (2) |
0.151 |
|
Complete visualization of abdominal cavity |
7 (4) |
8 (4) |
0.465 |
|
Shorter hospital stay |
7 (3) |
6.50 (3) |
0.778 |
|
No scar |
6 (5) |
6 (4) |
0.399 |
|
Shorter sick leave |
6 (3) |
6 (3) |
0.128 |
|
Shorter operative time |
3 (3) |
3 (3) |
0.069 |
|
Lower costs |
3 (2) |
3 (1) |
0.758 |
|
Shorter surgical training time |
3 (3) |
2 (2) |
0.026* |
|
Does not require general anesthesia |
2 (2) |
2 (3) |
0.003* |
|
Question 3 (most relevant features selected by physicians) |
|||
|
Safest procedure |
6 (2) |
7 (1) |
0.005* |
|
Less painful procedure |
9 (2) |
9 (2) |
0.855 |
|
Shorter sick leave (Faster return to daily activities) |
5 (2) |
5 (1) |
0.005* |
|
Less scars |
4 (2) |
4 (1) |
0.684 |
|
Sorter operative time |
4 (3) |
5 (2) |
0.758 |
|
Requires less surgical training |
2 (2) |
2 (1) |
0.631 |
|
Lowest cost |
1 (1) |
1 (1) |
0.019 |
Table 3. Comparison of scores according to participant educational level
* Statistically significant; SD: Standard deviation; IQR: interquartile range
In regards to question 3, women with higher educational level considered most important procedure safety (p=.005), while participants with a lower educational level ranked a faster recovery time as most important (p=.005).
DISCUSSION
When selecting the surgical approach to hysterectomy, many variables must be taken into account. However, these variables may be valued differently by the patient, health care provider performing the procedure, and healthcare systems. For example, the latter may consider procedure cost, technique availability at a locoregional level, faster recovery time, or difficulty of surgical training for adequate technique performance as most important variables (24). On the other hand, physicians may consider more important variables such as required operative time, received professional fees for performing a given technique, as well as their own personal training among others. For hospitals, variables such as operative time, cost or duration of hospital stay, may be of greater importance (25). Thus, in this study we aimed to better understand which variables are perceived as most important by women when choosing a surgical approach to hysterectomy. Our results indicate that for patients undergoing hysterectomy variables such as operative time, cost of procedure, or training time required by surgeon to properly perform each technique are of less relevance.
In fact, recommendations by the Cochrane metanalysis in 2015 indicated that vaginal hysterectomy should be the first choice of surgical approach to hysterectomy, since based on the analyzed studies they were able to show that it requires shorter operative time, has lower risk of urinary tract injury, and a faster return to daily activities (3). Nonetheless, the former two statements are arguable since graphical data of that same study does not show clear differences, and the presented confidence intervals lack statistical significance for both outcomes (3). More recently, the Sandberg metanalysis (6), which includes a greater number and newer studies, reported that the only disadvantage of LH compared with VH is a longer operative time, a variable that in our study was ranked as being of low importance to our participants.
In 2017, based on the Cochrane systematic review and meta-analysis, the ACOG recommendations indicated VH as first choice since it requires shorter operative time and is less expensive. In our study, the variable of procedure cost was ranked as second-to-last in importance in questions 1 and 2, and in last place in question 3 , this taking into account that all patients in Colombia have access to covered care. Furthermore, in the Sandberg meta-analysis, no significant difference in procedure cost was found between vaginal and laparoscopic hysterectomies (6). Altogether our results indicate that variables considered as relevant by physicians, which the ones currently used to issue recommendations, are not necessarily the most important to patients undergoing hysterectomy.
Upon deciding surgical approach to hysterectomy, participants in our study ranked lower complication rates as one of the most important aspects influencing their choice. In this regard, the ACOG and two recent meta-analyses were unable to find significant differences in rates of total, minor, or major complications between VH and LH, thus indicating that this may not be a criterion on which to base selection of surgical approach to hysterectomy (5-6,10). In fact, given these data, the most recent guideline of the Society of Obstetricians and Gynecologists of Canada recommends that, for benign indications, hysterectomy should be preferably approached by vaginal or laparoscopic approaches since these techniques present lower rates of complications than the abdominal approach (9)
In our study, participants experiencing less pain as the most important aspect influencing their choice of surgical approach to hysterectomy in questions 1 and 2, and the second most important in question 3. While the Cochrane review did not find significant differences in postoperative pain between vaginal and laparoscopic hysterectomy, a more recent meta-analysis shows that, compared with vaginal hysterectomy, laparoscopic hysterectomy was associated with lower pain score and required less analgesia (6).
Complete visualization of abdominopelvic cavity is a unique feature of laparoscopic surgery that has been widely highlighted as it allows the evaluation, identification, and treatment of pelvic and abdominal diseases (16). Interestingly, in our study the complete visualization of abdominopelvic cavity was ranked by participants as one of the most important items in questions 1 and 2, particularly by the group of 150 women who were about to undergo hysterectomy.
Regarding sick leave, previous meta-analyses (3,5) were unable to find significant differences in its duration and return to normal daily activities between laparoscopic and vaginal hysterectomy, suggesting that this may not be a feature to choose one over the other. Nonetheless, in our study, shorter sick leave was the third most valued feature in question 3 of our survey.
In this study, we found that a shorter hospital stay was ranked as 4th (of 12) most important feature in question 1, and section 2 of our questionnaire. Since 2007, our group has performed outpatient management in over 95% of patients undergoing total laparoscopic hysterectomy, and have not evidenced complications attributed to this approach to date. In agreement with this, the Dedden systematic review showed that outpatient management can be a safe approach for both vaginal and laparoscopic hysterectomy (26).
Six advantages of each laparoscopic and abdominal hysterectomies were listed in question 1, and interestingly, and participants ranked 6 of the 6 advantages of laparoscopic hysterectomy as their top 6 preferred items, strongly suggesting that women in our study would choose to undergo a laparoscopic hysterectomy rather than an abdominal one. In agreement with our findings, in the Kluivers study, after thoroughly explaining the advantages and disadvantages of abdominal and laparoscopic hysterectomy to a group of patients and a to a group of nurses, participants were asked to choose the surgical approach of their preference which showed that 84% of patients and 74% of nurses chose the laparoscopic approach (26). Furthermore, the Janda study reported that after thoroughly explaining all three surgical approaches, the majority of women preferred laparoscopic hysterectomy (40%), followed by vaginal (17%), and abdominal hysterectomy (5%) (14).
Because of the relevance that aesthetics may have for some women, and based on the Yeung study (15), we thus decided to include scar size and/or presence or absence among the most important variables to be evaluated in section 3 of our questionnaire. While scores obtained for this variable were usually in the middle range, thus not being the most nor the least important, we did find it to be statistically significant for younger women who were not undergoing hysterectomy.
LIMITATION
In this study, bias may have been introduced in question 3, since the most important aspects of hysterectomy listed in that section were randomly selected based on our professional opinion, which may differ from other researchers or populations.
The fact that there are currently no validated questionnaires addressing patient preference regarding approach to hysterectomy is what led us to design this study, even though this may also be perceived as a weakness of our study.
CONCLUSION
Our study suggests that certain aspects of hysterectomy that are considered as relevant by health care providers may not correspond to those valued by patients. Thus, our study provides a wake-up-call for physicians to transition from a model of medical paternalism towards an environment in which patients are more actively involved in the decision-making process regarding surgical approach to hysterectomy.
Thus, future studies carried out at additional locations are required to determine whether similar preferences are observed in patients around the world, or whether our results are specific to the Colombian population.
Disclosure statement:
The authors declare that they have no conflicts of interest and nothing to disclose.
Statement of prior presentation or publications and/or abstract/poster presentation
This article has not been previously submitted in presentation or publications and abstract/poster presentation
Contribution to Authorship
JFD: He participated in the conception, planification and creation of the research, participated in the development of the surveys, data analysis and the writing of the article
CCL: She participated in the conception and creation of the research, data analysis and the writing of the article
CC: She participated in the research planning, data analysis and the writing of the article
SMG: I participated in the conception and creation of the research, participated in the development of the surveys, data analysis and the writing of the article
AA: She participated in the conception and creation of the research, participated in the development of the surveys.
JB: He participated in the research planning , data analysis and the writing of the article
Details of Ethics Approval:
This research received ethics committee/IRB approval by The Research and Innovation Ethics Committee of the Faculty of Medicine of CES University Medellin, colombia . Date of approval was July 25 of 2019 and reference number is 219Proy001 .
Source of funding
This article has no source of funding