
Asli Ucyigit1*, James Goadsby2 and Ranzelle Fernandes2
1Consultant Obstetrician & Gynaecologist, Epsom and St Helier University Hospitals Trust, England, United Kingdom.
2Registrars in Obstetrics & Gynaecology, King’s College Hospital, London, England, United Kingdom.
*Corresponding Author: Asli Ucyigit, Consultant Obstetrician & Gynaecologist, Epsom and St Helier University Hospitals Trust, England, United Kingdom.
Received date: February 22, 2024
Accepted date: March 04, 2024
Published date: March 25, 2024
Citation: Asli Ucyigit, James Goadsby and Ranzelle Fernandes. (2024). “Isolated Torsion of the Fallopian Tube; A Rare Gynaecological Emergency.”. International J of Clinical Gynaecology and Obstetrics, 4(1); DOI: 10.61148/2836-0737/IJCGO/032.
Copyright: © 2024 Asli Ucyigit. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Isolated torsion of the fallopian tube is a rare gynaecological emergency. Although many gynaecologists will not encounter this condition in their careers, it must be considered as a differential diagnosis in pre-menopausal women presenting with acute onset unilateral pelvic pain in order to prevent delayed treatment and tubal loss.
Our case is of a 21-year-old nulliparous woman who presented acutely with severe, unilateral lower abdominal pain and vomiting. A transvaginal ultrasound scan revealed fallopian tubal cyst torsion and surgical management was expedited. De-torsion, cystectomy and tubal salvage was achieved; the patient made an uncomplicated recovery.
Our case highlights that there is at present no recognised guideline or consensus statement regarding the management of isolated tubal torsion. In view of this, we propose that current guidance for the management of ovarian torsion is extrapolated, aiding the decision on whether tubal de-torsion (and subsequent preservation of tubal function) or salpingectomy is performed.
fallopian tube; torsion; gynaecological emergency
Introduction:
The use of transvaginal ultrasound scanning is a crucial adjunct to clinical examination when evaluating a patient for suspected acute gynaecological pathology. This report describes the assessment and management of a young woman with a rare gynaecological emergency necessitating immediate surgical intervention.
Isolated torsion of the fallopian has multiple aetiologies including tubal cysts, previous surgical ligation of the tube and pre-existing hydro- or haematosalpinx. [1] It is a rare condition, the prevalence of which has been estimated at 1 in 1,500,000 women [2], and many gynaecologists may not encounter such a case during their careers. If diagnosis and treatment should be delayed, resultant ischaemia of the tube may lead to irreversible necrosis and loss of tubal function with implications for future fertility in the pre-menopausal patient.
We report a case of unilateral isolated tubal torsion secondary to a large para-fimbrial cyst, diagnosed only through the application of an urgent out-of-hours transvaginal ultrasound scan. The rapid diagnosis facilitated prompt surgical intervention, where de-torsion of the tube was possible, with concomitant preservation of tubal function. As such we emphasise the crucial part transvaginal ultrasound plays when assessing women with non-specific gynaecological signs and symptoms, and the possibility of organ preservation when confronted with adnexal torsion.
Case presentation:
The patient, a student in her early twenties, presented to the Accident and Emergency Department by ambulance in the early hours of the morning with a 12-hour history of acute onset left iliac fossa pain. The pain was described as ‘twisting’ in nature, intermittent (‘wave-like’) radiating upwards and posteriorly to the left renal angle. Associated with this were multiple episodes of vomiting with anorexia; importantly, no urinary or bowel symptoms were present, making a diagnosis of renal colic or viral gastroenteritis unlikely. The pain score was 10 out of 10, preventing sleep, despite the use of analgesics prior to presentation.
The patient’s last menstrual period was one week previously and was normal in nature, on a background of a regular menstrual cycle (suggesting a complication of early pregnancy was unlikely). This was further supported by the history of a single partner with whom the patient was currently practising abstinence. There was no medical or surgical history of note, and no previous pregnancies.
On arrival in the emergency department the patient’s observations were all within normal range, with no recorded tachycardia, tachypnoea, abnormal blood pressure or pyrexia. The administration of oral morphine provided significant relief and facilitated examination. Abdominal palpation revealed a soft, non-distended abdomen however involuntary guarding and tenderness were evident in the left iliac fossa. There was no renal angle tenderness, again making the diagnosis of renal pathology unlikely. Bimanual examination of the vagina did not reveal any pelvic abnormality; there were no palpable masses within the left adnexa nor was any tenderness elicited.
Investigations and differential diagnoses:
Urinanalysis revealed a ketonuria of ‘5+’, consistent with the history of vomiting and acute anorexia. Importantly, both the urinary and serum pregnancy tests were negative, rendering ureteric pathology or a ruptured ectopic pregnancy extremely unlikely. The serum leucocyte count was marginally elevated at 11.8, however all other serum parameters (urea and electrolytes, liver function and C-reactive protein) were normal. As the clinical history and examination findings were highly suggestive of ovarian/adnexal torsion, an immediate out-of-hours transvaginal ultrasound scan was undertaken to help elucidate the diagnosis. This revealed a normal uterus with a thin normal endometrium, consistent with the stage of the menstrual cycle. Of note, both ovaries were seen clearly and were normal in size and morphology. Medial and adjacent to the left ovary, situated in the midline of the pelvis was a unilocular, thick-walled cystic structure, measuring 54mm in its maximum diameter. (Figure 1) The structure was avascular with low level internal echogenicity. There were no incomplete internal septations suggestive of a hydrosalpinx, however the left fallopian tube could not be seen separately to this structure. There was a small amount of low-level echogenic fluid in the pouch of Douglas, the appearances of which were consistent with haematoperitoneum. There was significant tenderness in the left adnexa during the scan. A diagnosis of suspected fallopian tubal torsion secondary to a para-fimbrial cyst was made, and surgical management expedited.
Although isolated tubal torsion secondary to a tubal cyst was the most likely diagnosis based on the ultrasound scan findings, the presence of haematoperitoneum cast doubt on this theory. A possible differential was a ruptured haemorrhagic adnexal cyst, however the appearances of the cyst itself (absence of overtly haemorrhagic content) did not support this diagnosis.
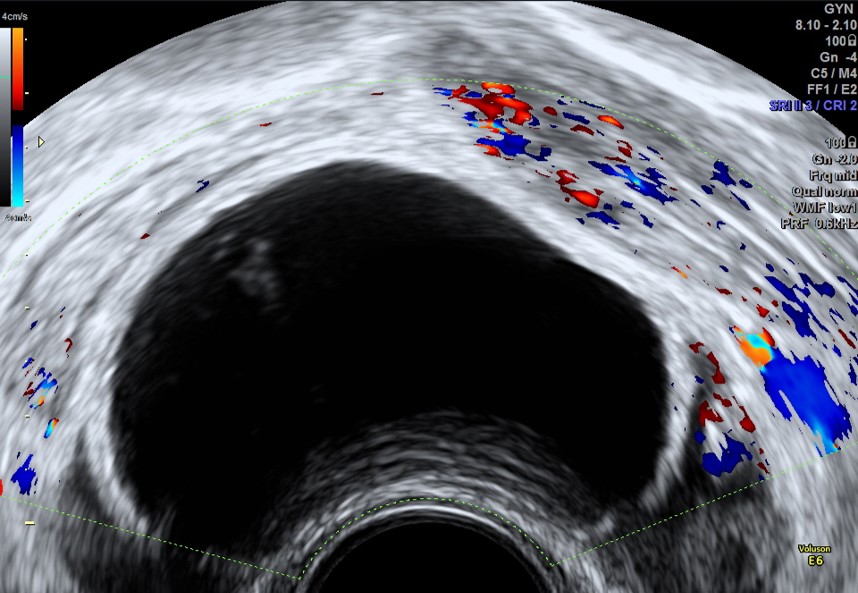
Figure 1: Transvaginal ultrasound scan image in the sagittal plane showing a unilocular thick walled cyst located in the pouch of Douglas, with low level echogenic content and no vascularity on colour Doppler.
Treatment & outcome:
An emergency laparoscopy confirmed the presence of a 6cm left para-fimbrial cyst, with associated torsion of the fallopian tube three times around its pedicle. (Figure 2) The tube appeared dusky and was partially covered in haemorrhagic material, explaining the small volume of blood identified in the pouch of Douglas at the time of scan. A laparoscopic de-torsion of the left fallopian tube and para-fimbrial cystectomy were performed; the fallopian tube regained its normal colour indicating reperfusion and successful preservation of the tube. The specimen was sent for histological analysis.
The patient made an uncomplicated recovery and was discharged home the following day. The possibility of tubal damage and future ectopic pregnancy was explained. A follow-up telephone consultation six weeks post-operatively established there had been no late complications of surgery. The histology report confirmed the presence of a collapsed cyst, with a single layer of flattened cuboidal cells (in parts containing a haemorrhagic and congested fibrous wall) in keeping with a torsion of a benign para-fimbrial fallopian tube cyst.
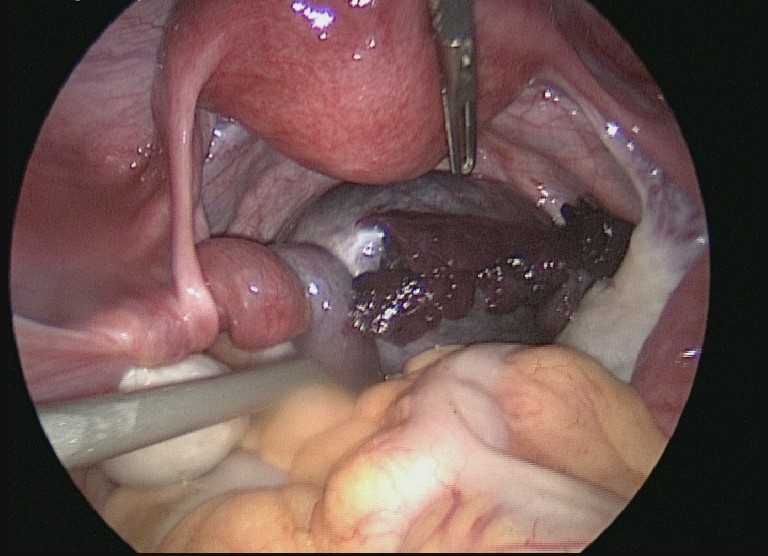
Figure 2: Laparoscopic view revealing a left para-fimbrial tubal cyst occupying the pouch of Douglas with torsion of the tube three times at its proximal end. Haemorrhagic content can be seen covering the external surface of the cyst and the distal end of tube appears ‘dusky’ in colour, suggesting ischaemic change.
Discussion:
Isolated torsion of the fallopian tube is a rare clinical occurrence, with a reported prevalence of 1 in 1,500,000 women [2]. There have been approximately 400 cases reported in the literature since the first descriptions by Bland-Sutton in 1890 [3] and Deblet in 1892 [4]. The diagnosis of fallopian tube torsion is challenging as the clinical symptoms and biochemical signs are non-specific [5]. The most common complaint is of severe abdominal pain, often localised to one of the iliac fossa [1]. Nausea and vomiting may also be present [6]. Our case is a key example of the non-specific symptoms and clinical findings associated with isolated unilateral tubal torsion, and emphasises the need for prompt imaging to confirm the diagnosis. Unlike this case, the majority of reported cases are of right sided torsion, possibly due to the fixation of the left tube by the sigmoid mesocolon [7]. There is only one known report of a bilateral tubal torsion [8].
The aetiology of tubal torsion is multiple. Suggested systems of classification include intrinsic (tubal) factors; tortuosity, excessive length of tube, hydrosalpinx, haematosalpinx, tubal ligation or incomplete distal mesosalpinx, and, extrinsic (mechanical/pelvic) factors; ovarian or para-ovarian masses, enlargement of uterus due to pregnancy and tubal adhesions [1]. These various aetiologies may all result in tubal torsion by impairing venous return from the fallopian tubes and ovaries with subsequent vasodilation, oedema and increase in the mass of the fimbrial end of the tube. The tube then torts around this point [9].
The occurrence of this emergency is less common is pre-menarchal and postmenopausal patients [2]. The patient may exhibit a leucocytosis as was in this case, however this is not reliably present [1,9]. The difficulty in diagnosis is of concern as if torsion is present, prompt recognition and treatment with laparoscopic detorsion is required within the first 24 hours of symptom onset in order to preserve tubular function [10]. It is important however to also maintain an awareness of the differential diagnoses of tubal torsion, which include; acute appendicitis, torted ovarian cyst, ectopic pregnancy, ruptured ovarian follicle/cyst, pelvic inflammatory disease, endometriosis and renal colic [5].
Isolated tubal torsion is rarely diagnosed pre-operatively [5] however modern imaging techniques have been reported to improve pre-operative diagnostic accuracy. Ultrasonography is often the first line investigation employed to assess pelvic pain and suspected gynaecological masses [11]. A common ultrasound finding is of a thick-walled cystic mass on grey scale ultrasound [12]; the use of colour Doppler techniques may identify areas of high impedance flow with reversed diastolic flow or absent blood flow secondary to torsion [11,13]. The utility of ultrasound as a diagnostic adjunct to clinical examination is supported by case series, which report between 60-100% of cases can be confirmed with ultrasound [10,14,15]. Other common ultrasound findings are dilated tubular structures in the adnexa, and (complex or non-complex) mid-line cystic masses, such as in the case we report [11].
Definitive management is surgical through laparoscopic or open tubal detorsion with the aim of preserving tubular function and fertility (16). Our case highlighted to us that there is at present no recognised guideline or consensus statement regarding the management of isolated tubal torsion. In view of this, we suggest that current guidance for the management of ovarian torsion is extrapolated to aid the decision on whether tubal detorsion or salpingectomy is performed [17]. Factors that must therefore be considered prior to selecting a management strategy are in keeping with those for ovarian torsion, (where de-torsion is favoured over oophorectomy). These are: the macroscopic appearance of the adnexa and whether tubal necrosis has ensued; menopausal status/age; pre-existing tubal pathology and the desire to preserve fertility [17].
Our case demonstrates that even in the absence of specific guidance, a generic approach to the management of adnexal torsion, with prompt diagnosis and surgical intervention can reverse organ ischaemia and prevent organ loss, with resultant preservation of (in this case tubal) organ function. An important and distinguishing point to note however when comparing detorsion and cystectomy of a fallopian tube to that of an ovary is that the potential intrinsic tubal damage from the torsion and surgical cystectomy must be emphasised to the patient, as there is a possible increased future risk of tubal ectopic pregnancy in those of childbearing age.
The patient’s perspective:
‘Before my partner rang emergency services, I experienced symptoms of hot and cold sweats, quick uncontrollable breaths that I couldn’t pace, passing out/fainting, vomiting, vision darkening, inability to concentrate or talk. The pain was constant and agonising, I experienced extreme restlessness, sitting still only worsened the pain. Prior to this around 4pm in the afternoon I felt a pain in the left abdominal/hip area that I understood it to be a dietary intolerance after doing a quick symptom search, it went away after around 10 minutes. I felt this pain on and off for a number of months but it always went away after a short period of time, only ever lasting a maximum of 10 minutes. I believed it was diet related and tried cutting out a number of foods trying to isolate the cause. After the operation I felt instant relief, I can’t thank Dr Aslı Üçyiğit and the whole team at Princess Royal Hospital enough. I’m forever grateful.’
The authors confirm that the patient gave their informed consent prior to the writing of this article.