
Tunde Maiyaki Ibrahim1,2*, Pascal Ogeleka3, Priyani Apsara Deluwatte1
1Medicine Department, Goulburn Valley Health, Graham Street, Shepparton, Vic 3630, Australia.
2Shepparton Rural Clinical School, the University of Melbourne, Department of Rural Health, 49 Graham Street. Shepparton., Victoria 3630, Australia
3Cardiology Department, Peninsula Health, Frankston-Victoria, Australia.
*Corresponding author: Tunde Maiyaki Ibrahim. Consultant Physician, Goulburn Valley Health and Seconded Senior Lecture, Shepparton Rural Clinical School, University of Melbourne.
Received date: July 28, 2022
Accepted date: August 03, 2022
Published date: August 08, 2022
Citation: Tunde Maiyaki Ibrahim, Pascal Ogeleka, Priyani Apsara Deluwatte (2022) “The Yield of Computerized Tomography, Perfusion Computerized Tomography and Diffusion-Weighted Magnetic Resonance Image in Patients Presenting with Transient Ischemic Attack and Acute Ischaemic Stroke.” International J of Clinical Cardiology and Cardiovascular Interventions, 2(4); DOI: http;//doi.org/08.2021/1.1012.
Copyright: © 2022 Tunde Maiyaki Ibrahim. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background: A transient ischaemic attack (TIA) or acute ischaemic stroke (AIS) with transient symptoms can presage a debilitating acute ischaemic stroke and some stroke mimics can have undesired consequences if not diagnosed and treated promptly. The use of computerized tomography (CT), perfusion computerised tomography (P-CT) and diffusion weighted magnetic resonance imaging (DW-MRI) is critical in facilitating early diagnosis and subsequent management of patients with acute focal neurological dysfunctions.
Aim: This study investigated the yield of computerised tomography (CT), Perfusion-CT(P-CT), and Diffusion weighted-MRI(DW-MRI) scans in patients Diagnosed with TIA and AIS.
Methodology: This is a retrospective cohort study of 162 cases of TIA (55%) and acute ischaemic stroke (AIS), who presented to Goulburn Valley Hospital in Shepparton from January to December 2021. Microsoft EXCEL software was used for statistical analysis. The chi-square test with Yates' correction was used to compare propositions, and a p-value of < 0.05 is considered statistically significant.
Results: The male to female ratio was 1.5 to 1, with a mean age of 74 years. The initial CT brain was normal in all 89 TIA patients, while 69.8% of the 63 AIS patients had infarct. 95% of AIS (n=41) patients had perfusion abnormalities on P-CT compared to only 17% of TIA patients (n=71) (P<0.00001). Similarly, 94% of AIS (n=35) compared to 18% of TIA (n=55) patients had diffusion weighted abnormality on DW-MRI (p<0.00001).13.5% of the TIA case(n=5) and 100% of the AIS(n=5) with normal CT and P-CT had diffusion abnormality on DW-MRI. Among the 4 TIA cases that had DW-MRI after normal CT and positive P-CT only 20% (n=1) showed diffusion abnormality. On CT carotid and cerebral angiograms, 49% of TIA (n=37) compared to 76% of AIS (n=55) patients had significant stenosis of over 50% (p<0.01).
Conclusion: Normal initial CT brain is a valuable initial test for differentiating TIA from AIS in patients with acute focal neurologic dysfunctions. The addition of P-CT and DW-MRI imaging demonstrated abnormalities in most of those with AIS when compared with those with TIA. Although a small percentage of those with TIA had abnormalities on P-CT and DW-MRI these two modalities add value to investigation of TIA. Therefore, the use of P-CT and DW-MRI are pertinent when the initial CT brain is normal as they are more sensitive in demonstrating abnormalities than plain CT.
Background
Acute ischemic stroke (AIS) and transient ischemic attack (TIA) are major global public health issues. In Australia, three strokes occur every hour and more than twenty-seven thousand Australians had their first stroke in 2020. Stroke is one of Australia's leading causes of death- It claims more women's lives than breast cancer and more men's lives than prostate cancer [1]. TIA is an acute transient focal neurological dysfunction due to focal brain, spinal cord or retinal ischemia from arterial occlusion lasting for less than 24 hours without neuroimaging evidence of tissue infarct. It accounts for about 30% of all acute cerebrovascular disease [2-4]. A TIA portends a high risk of developing a major AIS which is a sudden focal neurological dysfunction due to arterial occlusion lasting over 24 hours with evidence of brain infarct on neuroimaging [2,5]. In the acute setting the clinical relevance of differentiating TIA from a subtype of AIS with transient symptoms lasting for less than 24 hours but, unlike TIA ,shows evidence of infarct on initial neuroimaging is still debatable. Because both have similar clinical characteristics and prognoses for survival and recurrent major stroke. However rapid and accurate diagnosis is required for timely treatment of these conditions to reduce the risk of future major stroke [2,6]. The second clinical scenario that is sometimes missed diagnosed as a subset of possible AIS is that of focal neurological symptoms that last for more than 24 hours with no evidence of tissue damage on neuroimaging. These are likely stroke mimics as there are no abnormalities on neuroimaging to suggest tissue damage and couldn’t be TIA in the sense that even with the absence of tissue damage on neuroimage the prolong duration is contradictory. To facilitate early diagnosis of TIA, AIS and stroke mimics, the perfusion computerized tomography (P-CT) and diffusion weighted magnetic resonance imaging (DW-MRI) have been employed to investigate for evidence of tissue perfusion and diffusion abnormalities. Therefore helping to differentiate TIA ,AIS and stroke mimics such as hemiplegic migraine and Todd paralysis [6-8].
Aim
The aim of this study is to examine the yield of computerized tomography (CT), P-CT, and DW-MRI scans in patients with acute focal neurological symptoms (TIA and AIS).
Materials and Methods
A retrospective cohort study of patients admitted with diagnoses of TIA and AIS to the Goulburn Valley Health in Shepparton - Victoria between January and December 2021. The Goulburn Valley Health Databases (CHARTVIEW and COLDFUSION) were used to obtain data for TIA and Ischemic stroke diagnoses, as well as neuroimaging reports. Every TIA and AIS diagnosis was matched with their radiological reports before the data was de-identified. All patients presenting with TIA (a transient focal neurological symptoms caused by arterial occlusion that last less than 24 hours and is not associated with new infarcts on neuroimaging), and AIS (a sudden focal neurological symptoms accompanied by new infarcts on neuroimaging) had CT brain and P-CT scans performed within a few hours of arriving at the emergency department, and the DW-MRI was completed within a few days of admission during the study period were included. Exclusion criteria included patients with haemorrhagic stroke, stroke mimics and those with non-focal neurologic symptoms. Microsoft EXCEL software was used for statistical analysis and chi-square (z-test) statistic with Yates' correction was used to compare propositions with a p-value of <0.05 considered statistically significant. The Goulburn Valley Health Ethics Committee granted ethical approval for this study and subsequent publication of the findings.
Results
A total of 257 cases were coded as TIA and AIS, with 162 meeting both TIA (n=89, 55%) and AIS (n=73, 45%) inclusion criteria, and 89 were excluded for not meeting the selection criteria. The average age of the 162 patients was 74 years, with a male to female ratio of 1.5 to 1. Of the 89 people who had TIA, 19 (21%) had definite TIA (had perfusion and/or DW-MRI abnormalities) and 70 (79%) had probable TIA (no neuroimaging abnormalities). Unilateral motor deficit was the most common presenting symptom, accounting for 61% (n=54) and 90% (n=66) of TIA and AIS presentations, respectively (z=18.4666, p=0.000017). Speech disruption was reported in 44% (n=39) of TIA patients and 41% (n=30) of AIS patients (z=0.0358, p-value =0.849907). Although focal visual defect was seen more in patients with TIA (19) than AIS (7) the difference was not statistically significant (z=3.2895, p=0.069724). The details of the clinical symptoms are shown in Figure 1.

All (n=89,100%) TIA patients had normal initial brain CT whereas majority (n=63,70%) of the AIS patients had infarcts. The P-CT scans demonstrated perfusion abnormalities in 17 % of those with TIA (n=71) compared to 95% of those with AIS (n=43), (z=66.249, p<0.00001). 94% of the cases of AIS (35) and 18% of the TIA patients(n=55) with normal initial CT brain showed diffusion weighted abnormality on DW-MRI (z=46.6468,p< 0.00001.).The details are depicted in Figure 2
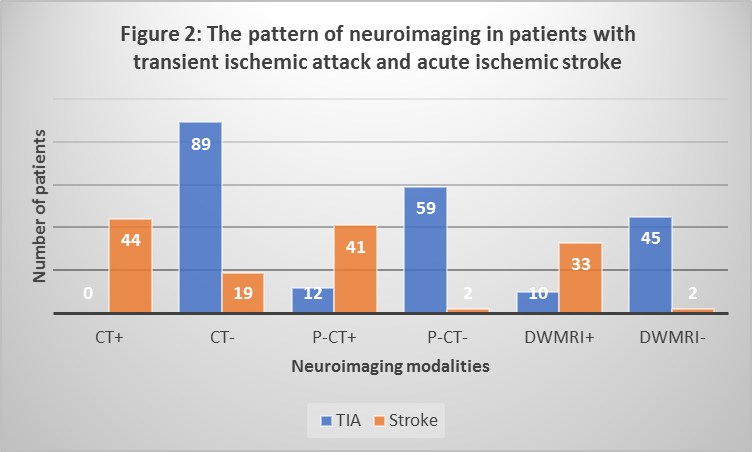
Table 1 showed the yield of the combination of various neuroimaging.13.5% of the TIA and 100% of those with AIS cases with normal CT and P-CT had diffusion abnormality on DW-MRI. While among the 4 TIA cases that had normal CT but positive P-CT only 20% (n=1) showed diffusion abnormality.
|
Table1: The yield of combining Subsets of neuroimaging in patients with transient ischemic attacks and ischemic strokes
TIA AIS |
||
|
Neuroimaging |
n=37(%) |
n=5(%) |
|
CT-/P-CT-/ DWMRI+ |
5(13.5) |
5(100) |
|
CT-/P-CT-/DWMRI- |
32(86.4) |
0 |
|
|
n=5(%) |
n=0(%) |
|
CT-/P-CT+ / DWMRI+ |
1(20) |
0 |
|
CT-/P-CT+/DWMRI- |
4(80) |
0 |
|
TIA=Transient ischemic attack |
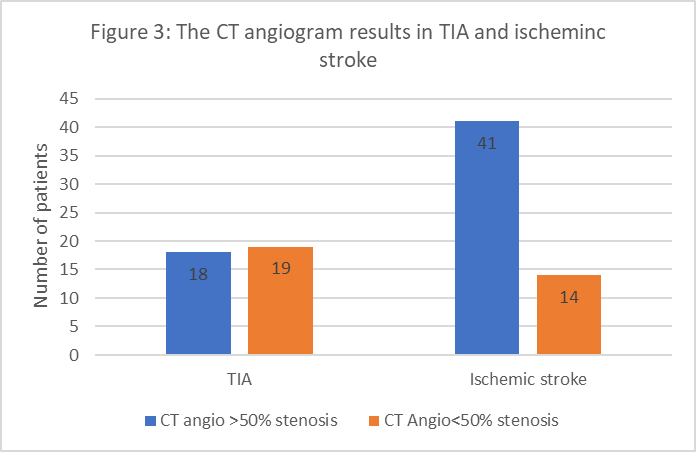
On CT carotid angiogram 49% of TIA (n=37) compared to 76% of AIS (n=55) patients had significant stenosis of over 50% (z=6.4488, p<0.01) detail is shown in figure 3.
Discussion
Unlike with AIS there is no clinical benefit in distinguishing between TIA and AIS with transient symptoms (AIS with symptoms lasting less than 24 hrs) in terms of survival and prognosis for recurrent major stroke [5]. Nonetheless, accurate and timely diagnosis clinically and radiologically is required for prompt treatment of these conditions to reduce the risk of future major stroke [6]. Motor deficit was the most common presentation in both TIA and AIS patients in this study, but it was significantly more common in AIS patients than TIA patients. Speech and visual disturbance were the next most common, but they were more common in those with TIA than in those with AIS. These clinical parameters can be used to differentiate AIS from TIA on clinical grounds before the neuroimaging result is available. These findings are consistent with those in previous research [3,4,7-10].
In this study, as in the one by Lu et al. [11], all the TIA patients had normal initial CT brain scans. On further investigation with P-CT and DW-MRI we described two groups of patients with TIA: definite TIA (21%) and probable TIA (78%) based on presence or absence of focal perfusion and diffusion abnormalities on P-CT and DW-MRI neuroimaging respectively. In contrast, 70% of AIS patients have infarcts on initial CT brain scan, and all have evidence of tissue damage in at least one neuroimaging study (CT, P-CT or DW-MRI). This finding supports the view that the presence of infarct (tissue damage) on neuroimage is confirmatory of AIS regardless of the duration of the acute focal neurological dysfunctions. On the other hand, normal initial CT is most likely to be seen in TIA [3,4,9,12]. On further evaluation with P-CT, 17% of TIA patients in our study had perfusion abnormality, which is similar to previous studies that found perfusion abnormality on P-CT or Perfusion-MRI in 14% to 34% of patients with TIA. Mlynash et-al, [9] reported that 33% of the TIA patients they studied had perfusion abnormalities on MRI. Similarly, Prabhakaran et al, [12] showed that approximately 34% of their TIA patients had perfusion abnormalities on P-CT. The studies by Mlynash et-al [9], Inatomi et-al [7], and Restrepo et-al [12], observed a rate of diffusion abnormality on DW-MRI in TIA cases of 35%, 52.1%, and 68% respectively much higher than the 18% we found in our TIA patients. This is much lower than the 94 % seen in the AIS patients who had diffusion abnormality. The difference between our study and earlier studies is likely due to smaller sample sizes in the earlier studies.
P-CT and DW-MRI are two sensitive neuroimaging techniques that have been shown to improve diagnostic yield in differentiating between TIA and stroke with transient symptoms among patients with acute transient focal neurologic symptoms [3,10,13,14]. In contrast to TIA, all our patients with AIS irrespective of duration of symptoms had abnormalities on either acute (initial < 6 hours) and/or subacute (< 9 days) neuroimaging. This supports the fact that tissue damage (infarct) on neuroimaging whether acute or subacute, in patients with acute transient focal neurological dysfunction is confirmatory of AIS [1-3,13]. This view has led to the clamour for a new definition of TIA, which is mainly based on the absence of tissue damage on neuroimaging rather than the duration of symptoms [4]. This definition appears more practical than the time definition as patients’ recollection of onset of symptoms may be unreliable in certain circumstances, especially in geriatric patients with cognitive issues. Although the current concept of TIA as an ischemic episode in which symptoms are transient and not associated with brain injury seem to be gaining ground recent evidence suggests that brain injury almost always occurs during TIA with diffusion abnormalities seen on DW-MRI in some TIA patients reported in this study and earlier ones [7,9,12,15]. Probable the time has come to change the nomenclature as suggested by Shubhakaran16 from TIA to acute ischemic stroke syndrome to accommodate for this observations on the new highly sensitive neuroimaging techniques.
The presence of diffusion abnormality does not only help in diagnosis but also in predicting the short and long-term stroke risk post TIA [12,17]. Prabhakaran et al, [12] found that the risk of stroke after DWI-positive TIA is as high as 30% in the first 90 days. Therefore, it is important to perform DW-MRI in all patients presenting with symptoms suggestive of TIA for both diagnostic and prognostic purposes.
Apart from perfusion and diffusion abnormalities carotid and cerebral angiogram was the other neuroimaging employed for investigation of our patients. In several studies, stenosis of greater than 50% and/or significant atheroma in carotid and /or cerebral arteries on CT angiography were associated with motor dysfunctions and an increased chance of abnormalities on P-CT and DW-MRI [10,12,14]. In consonance with these previous studies, we found more significant stenosis on CT carotid angiogram in patients with AIS (75%) than those with TIA (49%).Of all the neuroimaging techniques significant stenosis on CT carotid angiogram seems to be present in almost half of those with TIA. Therefore, TIA should be considered in patients with acute focal neurological dysfunction even in the absence of perfusion and diffusion abnormalities if they have significant stenosis and /or atheroma on the carotid angiogram. We didn’t, however, link the CT carotid angiogram to the types of symptoms as was done in other studies. Earlier studies report that TIA patients with motor symptoms were more likely to have significant atheroma and stenosis in the carotid and cerebral arteries [10-12].
Urgent CT brain performed in patient arriving in the emergency department has been the minimum standard for investigating patients with acute focal neurological dysfunction in most hospitals because it is readily available and accessible, as opposed to high resolution P-CT and MRI [9,13,18]. This enables the early differentiation of TIA from AIS and the provision of definitive therapy to prevent future major AIS in TIA patients and to mitigate the impact of major AIS [3,6,19]. Compared to DW-MRI, high-resolution P-CT has significant advantages. Firstly, P-CT techniques are widely used in both metropolitan and regional hospital settings, including ours and can be done simultaneously with the initial CT. In most health facilities the median time from onset of symptoms to P-CT (12 hours) is considerably shorter than in DW-MRI (24 hours) [13,14]. Secondly, P-CT is a rapid test with data acquisition lasting about 40 seconds and can be perfumed in sequence with, initial CT and CT carotid angiography without the use of extra dose of contrast. It also can be interpreted quantitatively and qualitatively. Finally, it can be used in patients who are unable to have an MRI due to claustrophobia, pacemakers, implantable cardioverters, or other metal implants. However, PCT has a significant disadvantage in terms of the volume of brain tissue that can be analysed [14]. In view of the advantages of P-CT and CT angiogram they should be performed during the initial CT where available and practicable as this will enhance the timely differentiation of TIA from AIS and these two from stroke mimics.
The potential limitation of this study is that it is a retrospective study therefore some conditions that mimic TIA (migraine, Todd paralysis and demyelinating disorder tumors), could have wrongly be coded as having TIA as only about a quarter had perfusion/diffusion abnormalities. We suggest that highly powered multi-centre prospective study is required to further evaluate the yield and pattern of neuroimaging techniques in TIA and AIS patients.
Conclusion:
Normal initial CT brain is a valuable initial test for differentiating TIA from AIS in patients with acute focal neurologic dysfunctions. The addition of P-CT and DW-MRI imaging demonstrated abnormalities in most of those with AIS when compared with those with TIA. Although a small percentage of those with TIA had abnormalities on P-CT and DW-MRI these two modalities add value to investigation of TIA. Therefore, the use of P-CT and DW-MRI are pertinent when the initial CT brain is normal as they are more sensitive in demonstrating abnormalities than plain CT.