
Tunde Maiyaki Ibrahim1,2*, Priyani Deluwatte1, Pascal Ogeleka1
1Medicine Department, Goulburn Valley Health, Graham Street, Shepparton.Vic 3630, Australia.
2Shepparton Rural Clinical School, The University of Melbourne, Department of Rural Health, 49 Graham Street. Shepparton.Vic 3630.Australia
*Corresponding Author: Tunde Maiyaki Ibrahim,Consultant physician Goulburn Valley Health and Seconded Senior lecture Shepparton Rural Clinical School, University of Melbourne.
Received date: January 27, 2022
Accepted date: February 03, 2022
Published date: February 07, 2022
Citation: Tunde Maiyaki Ibrahim, Priyani Deluwatte, Pascal Ogeleka (2022) “The Pattern of Intracranial Bleed, A Real-World Experience of The Impact of Falls and Use of Antiplatelets and Anticoagulants on The Outcome.” International J of Clinical Cardiology and Cardiovascular Interventions, 2(4); DOI: http;//doi.org/04.2021/1.1009.
Copyright: © 2022 Tunde Maiyaki Ibrahim. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background: Intracerebral bleed (ICB) is prevalent in geriatric patients, particularly among those on antiplatelet (ATPs) or anticoagulant medications (ACs). In stroke-prone patients, ACs use accounts for about 1 to 2% of ICB annually and similarly, ATPs use is associated with increased risk of ICB, especially in patients with head trauma. About 42% of the patients on ATPs with head trauma may have ICB. The commonest types of ICB are intracerebral haemorrhage (46-86%), subdural (13-45%), and subarachnoid haemorrhage (1-8%). The fatality from ICB is worsened using ACs/or ATPs.
Methodology: This is a retrospective observational cohort study of patients who presented with ICB to Goulburn Valley Health Shepparton, Australia from January 2019 to December 2019. The de-identified data for the diagnosis of ICB, ATPs/OACs, falls and demographic characteristics of patients were obtained from the Goulburn Valley Health Database (CHARTVIEW).
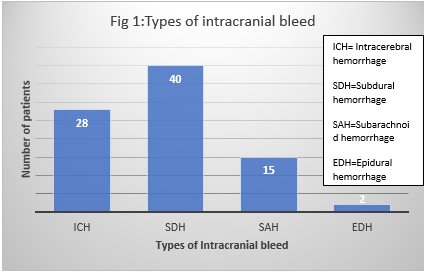
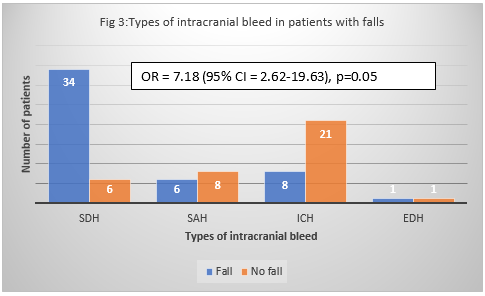
Results: There were 85 patients admitted with ICB of various types between January and December 2019. The male to female ratio was 1.2 to 1 and the mean age was 76.1 years (21-98 years). 82% were ≥ 61 years and 18% were ≤ 60 years old. Most of the patients had extra cerebral ICB (65.7% vs 73.3%, z=0.0713, p=0.78 ). The most common ICB in descending order included SDH (47%), ICH ( 33%), SAH (18%), and EDH (2%). 80% of the patients with SDH were ≥ 61 years old while only 20% were ≤ 60 years old. Similarly, 86% and 87% of those with SAH and ICH, respectively, were ≥ 61 years old. Of the 85 cases of ICB, 58% were precipitated by falls, while 42% had no fall. 73% of extracerebral ICBs (SDH, SAH & EDH) were also associated with falls, compared to 27% of the intracerebral (ICH) ICBs. Extracerebral ICBs have about 7 times odd of developing than ICH in patients with falls (OR = 7.18, 95% CI = 2.62- 19.63). Among patients with falls, 67.5% with ICB received ATPs/or ACs compared to 32.5% who did not take ATPs/or ACs. Of the patients with ICB without a history of falls, 56% received no ATPs/Or ACs. The odd of ICB from a fall is 2.6 times higher in those who took ATPs/ACS than in those who did not receive these medications (95% CI = 1.06-6.27, p = 0.05). Even though there were more patients treated with ATPs (n = 30) than with ACs (n = 16), there was no statistically significant difference in the likelihood of developing extracerebral ICB compared to ICH ICB between both groups OR=0.79 (95% CI = 0.22- 2.86).
Extracerebral ICB is the most common ICB independent of ATPs/ACs (Z = 0.135, p = 0.7). The case-fatality rate (CFR) of ICBs was 24%, which was statistically highest in patients with ICH (41%), and followed by SAH (36%) and SDH (12.5%), (p =0.0189). The odds of dying from ICH ICB was statistically significantly higher than that of extracerebral ICB, with an OR = 3.25(95% CI 1.19-8.89, p = 0.0369). The likelihood of dying from ICB is higher with ATPS/or ACs, with OR = 2.74 (95% CI = 0.89 – 8.41, p = 0.05), whereas falls alone did not raise the odds of dying from ICB, with OR = 0.67 (95% CI = 0.24-183).
Conclusion: ICBs are prevalent in our community, with most cases in the elderly people on ATPs/ACs and with history of falls. Additionally, the combination of APT/or ACs with falls, rather than falls alone, increased the odds of dying from ICBs. Considering the small sample size of this study, we recommend more studies that utilize a larger sample size and multivariate analysis to answer this question more affirmatively.
Introduction
Intracerebral bleed (ICB) is prevalent in geriatric patients, particularly among those on antiplatelet (ATPs) or anticoagulant medications (ACs). In stroke-prone patients, ACs use accounts for about 1 to 2% of ICB annually.1-3 Similarly, ATPs use was associated with increased risk of ICB, especially in patients with head trauma. According to Alter et al, 4 42% of the patients on ATPs with head trauma had ICB. Among patients on oral anticoagulants who developed ICB, 46% to 86%, 13% to 45% and 1% to 8% were intracerebral haemorrhage (ICH), subdural (SDH), and subarachnoid haemorrhage (EDH), respectively5,6. Additionally, there is a complex interaction between OACs/ATPs use, falls, neurodegenerative diseases and ICB. Most patients on OACs and ATPs are elderly and more prone to cerebral vessels diseases (amyloid angiopathy), neurodegenerative diseases and falls. Amyloid angiopathy a common pathology in neurodegenerative diseases is a recognised risk factor for spontaneous ICB. Similarly neurodegenerative diseases increase the likelihood of ICB because of falls.
In Australia, falls are a leading cause of hospitalisation (42%), and death by injury (40%).7 There have been opposing views on the benefits and risks of prescribing anticoagulants to patients at high risk of falls because of the increase likelihood of precipitating ICB. While some earlier studies4-6 showed that patients on ATPs/ or OACs are at increased risk of ICB, Ganetsky et al 2017,8 found that ground level falls in patients on ATPs/or ACs did not significantly increase their risk of ICB. The goal of this study is to find out the odd of developing and dying from ICB in patients on ATPs and ACs who had falls.
Aim: This study was conducted to investigate the real-world odds of developing and dying from ICB in patients who had falls while on ATPs /or ACs.
Methods
This is a retrospective observational cohort study of patients who presented with ICB to Goulburn Valley Health Shepparton, Australia from January 2019 to December 2019. The de-identified data for the diagnosis of ICB, ATPs/OACs, falls and demographic characteristics of patients were obtained from the Goulburn Valley Health Database (CHARTVIEW). The propositions were compared using the chi square(z-test) statistic with Yates’s correction and a p-value of < 0.05 is statistically significant. The odd ratio (OR) and 95% confidence interval (CI)was calculated for the causal relationship between ATPs/OACs, the odds of fatality and ICB. Ethical approval for this assessment and subsequent publication of the findings was obtained from the Goulburn Valley Health Ethics Committee.
Results
This study enrolled 85 patients admitted with ICB of various types at Goulburn Valley Health, Shepparton, between January and December 2019. The ratio of men (n = 47) to women (n = 38) was 1.2 to 1 and the mean age was 76.1 years (21-98 years). 82% (n = 70) were ≥ 61 years old and 18% (n = 15) were ≤ 60 years old. The most common ICB in descending order included SDH (n = 40, 47%), ICH (n = 28, 33%), SAH (n = 15, 18%), and EDH (n = 2, 2%), the details are shown in Figure 1.
Most of the patients whether ≥ 61 years or ≤ 60 years had extra cerebral ICB (65.7% vs 73.3%, z=0.0713, p=0.78).80% of the patients with SDH were ≥ 61 years old while only 20% were ≤ 60 years old. Similarly, 86% and 87% of those with SAH and ICH, respectively, were ≥ 61 years old (Figure 2).

Of the 85 cases of ICB, 58% (n = 49) were precipitated by falls, while 42% (n = 36) had no documented history of a fall. The majority of extracerebral ICBs (SDH, SAH & EDH) (n = 56, 73%) were also associated with falls, compared to 27% of the intracerebral (ICH) ICBs. Extracerebral ICBs have about 7 times odd developing than ICH from falls (OR = 7.18, 95% CI = 2.62- 19.63), as shown in Figure 3.
Among patients with falls, 67.5% (n = 33) who sustained ICB received ATPs/or ACs (n = 49) compared to 32.5% (n = 16) who did not take ATPs/or ACs. Of the patients with ICB without a history of falls, 56% received no ATPs/Or ACs. The odd of ICB from a fall is 2.6 times higher in those who took ATPs/ACS than in those who did not receive these medications (95% CI = 1.06-6.27, p = 0.05) as illustrated in Figure 4.

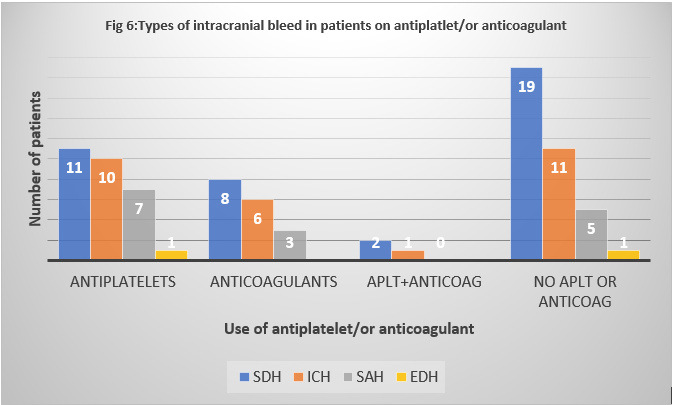
Even though there were more patients treated with ATPs (n = 30) than with ACs (n = 16), there was no statistically significant difference in the likelihood of developing extracerebral ICB compared to ICH ICB between both groups, with an odd ratio of 0.79 (95% CI = 0.22- 2.86). As shown in Figure 5, extracerebral ICB is the most common ICB independent of ATPs/ACs (Z = 0.135, p = 0.7).
SDH is the most prevalent extracerebral ICB in patients using ATPs and ACs, followed by SAH. Figure 6 shows a similar pattern in those who used neither ATPs nor ACs, with 69% having extracerebral ICH, of which 75% are SDH.

The most common antiplatelet and anticoagulant used were aspirin (n=43,70% ) and apixaban (n=19, 39%), respectively specifics are shown in Table 1.
Table 1: Characteristics of the patients with intracranial bleed.
|
Characteristics |
Total n=85 |
|
Mean Age Male: Female ratio Fall
Antiplatelet Anticoagulant No antiplatelet/anticoagulant Anticoagulant + Antiplatelets Dual antiplatelets Types of Antiplatelets Aspirin Clopidogrel Dipyridamole Dipyridamole+Aspirin combination Types of anticoagulants Apixaban Rivaroxaban Dabigatran Warfarin Enoxaparin
Case fatality rate (CFR) Outcome of patients with ICB & fall
Survived Died
Outcome on Antiplatelets /or Anticoagulant Died Survived
|
76.1yrs (21-98 yrs) 1.2:1 (M = 47. F = 38) Yes= 49 (57.6%) No=36(42.4%)
n =85(%) 32 (35.3) 19 (22.4) 36 (42.4) 3 (3.5) 6 (7.1) n = 40,(%) 30 (75.0) 5 (12.5) 1 (2.5) 4 (10.0)
n=19,(%) 7 (36.8) 5 (26.3) 2 (10.5) 3 (15.8) 2 (10.5)
23.5% (20/85) Fall Yes = 49(57.6%) No= 36(42.4%) 39 26 10 10 OR = 0.67(95% CI = 0.24-1.83)
Antiplatelet/Anticoagulant use Yes.n = 49(%) No = 36(%) 15(30.6) 5(13.9) 34(69.8) 31(86.1) OR = 2.74(95% CI = 0.89-8.41) |
In this study, the case-fatality rate (CFR) of ICBs was 24%, which was statistically highest in patients with ICH (41%), and followed by SAH (36%) and SDH (12.5%), (p = 0.0189). Table 2 shows that the odds of dying from ICH ICB was statistically significantly higher than that of extracerebral ICB, with an OR = 3.25(95% CI 1.19-8.89, p = 0.0369). The likelihood of dying from ICB is higher with ATPS/or ACs, with OR = 2.74(95% CI = 0.89 - 8.41, p = 0.05), whereas falls alone did not raise the odds of dying from ICB, with OR = 0.67 (95% CI = 0.24-183).(table 1).
|
Table 2: The case fatality rate among the types of intracranial bleed |
|
|
|
|
Types of Intracranial bleed |
Survived(n) |
Died(n) |
Case fatality rate(%) |
|
Subdural haematoma |
35 |
5 |
12.50 |
|
Subarachnoid haematoma |
9 |
5 |
35.70 |
|
Intracerebral haematoma |
17 |
12 |
41.40 |
|
Epidural haematoma |
2 |
0 |
|
|
Z = 7.9306, p = 0.018962 (excluding epidural haematoma) |
|||
|
Extracerebral haematoma |
46 |
10 |
21.74 |
|
Intracerebral haematoma |
17 |
12 |
41.38 |
|
OR = 3.25(95% CI = 1.19-8.89), z = 4.3526. p = 0.036952 |
Discussion
This is a 12-month retrospective observational study that examined 85 documented cases of ICB who presented to the Goulburn Valley Health. The mean age of the study population is 73.1 years (age range 21 to 93), with majority of them being over 61 years of age. The age of our patients is comparable to that reported in previous studies. 4-9 Elderly patients are prone to falls, including head and neck trauma, which increases the risk of ICB. 7
Extracerebral ICBs account for the majority of ICBs in this study (80%), with SDH making up almost half of all ICBs (47%). This is like a study by Hart et al 5. who reported that extracranial ICBs (55%) were the most prevalent form of ICBs but differs from other prior studies by Hankey et al 6. and Nilsson et al 10. who found that ICH ICBs were the most common type of ICBs. The plausible reason for the above discrepancy could be related to the higher rate of falls (73%) in the extracranial ICBs group compared to the ICH ICBs category (27%), as shown in our study. Consistent with several other studies,4-6,11 our study found that falls are associated with an increased risk of ICBs, but contradict the finding by Ganetsky et al 8, who found not statistically significant increased risk of ICB in their patients on ATPs and ACs from ground level falls.
Although this study showed an increased risk of ICBs in patients who had a fall while on ATPs and ACs, there was no difference in the risk of developing extracerebral ICBs compared to ICH ICBs between the ATPs and ACs subsets. In contrast to our findings, Ganetsky et al 8. reported no significant risk of ICBs from floor level falls in patients receiving various ATPs/or ACs. Given the overwhelming evidence from the 1960s to the 1980s that low dose aspirin reduced the risk of cardiovascular disease, aspirin is widely used by people with cardiovascular disease.s 12 A meta-analysis by van den Brand et al 13, showed that ATPs use can nearly double the likelihood of ICBs. Several previous studies showed a wide variability in ICH rates (4-67%) in patients on ATPs who had head trauma.13-15 The use of ACs has been associated with an increased risk of ICBs regardless of head trauma. Although the RE-LY5 and ROCKET-AF 6 studies found that the use of OACs reduced the risk of ischemic stroke, it also raised the risk of ICBs. While the mechanism of spontaneous ICBs in those on antithrombotic agents is not well understood, some of the proposed mechanisms include OACs-induced vasculopathy and the loss of an innate haemostatic process that normally seals a leaky vessel thus prevent severe ICB.5
The chances of dying from ICBs was higher in patients with ICH ICBs compared to those with extracerebral ICBs. These findings are consistent with those of other studies. 1,2,5,6 Although both Hart et al 5, and our study reported highest mortality rate and CFR respectively in patient with ICH ICBs respectively, there were some variations in the findings. While Hart and colleagues 5 found the second and third highest death rates in patients diagnosed with SDH and SAH, respectively, SAH accounted for the second highest CFR in our study. Patients on ATPs/ACs with falls are more likely to die with the odds of these patients dying from ICBs after a fall increased by about 26%. This is probably because the ATPs/or ACs increase the rate of ICB expansion, and therefore the size, and subsequently intracranial pressure, leading to death.16 Therefore, we recommend the fall prevention strategies in patients on ATPs/ACs to reduce the risk of ICB and its fatality. Furthermore, patients’ stratification before antithrombotic initiation using a brain CT/MRI scan to exclude those with intracranial small vessel disease- a known risk for ICB- can result in reducing the risk of ICB while on ATPs and ACs 5.
In conclusion, ICBs are prevalent in our community, with most cases in the elderly people on ATPs/ACs and with history of falls. Additionally, the combination of APT/or ACs with falls, rather than falls alone, increased the odds of dying from ICBs. Considering the small sample size of this study, we recommend more studies that utilize a larger sample size and multivariate analysis to answer this question more affirmatively.