
Ajmer Singh1*, Ravina Mukati2, Swati Joshi3, Sushane Hakhoo4
Department of Cardiac Anaesthesia, Institute of Critical Care and Anesthesiology, Medanta-The Medicity,
Sector-38, Gurugram Haryana.
*Corresponding authors: Ajmer Singh, Department of Cardiac Anaesthesia, Institute of Critical Care and Anesthesiology, Medanta-The Medicity, Sector-38, Gurugram Haryana.
Received Date: May 10, 2024
Accepted Date: June 15, 2024
Published Date: June 20, 2024
Citation: Ajmer Singh, Ravina Mukati, Swati Joshi, Sushane Hakhoo, (2024). “Asymptomatic Soft Tissue Cysticercosis and Cardiac Surgery”. Clinical Research and Clinical Case Reports, 5(2); DOI: 10.61148/2836-2667/CRCCR/80.
Copyright: © 2024 Ajmer Singh, This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cysticercosis, the most common parasitic infection, is caused by ingestion of Taenia solium eggs from contaminated food. Neurocysticercosis is the most common manifestation of this disease. Uncommonly, asymptomatic soft tissue cysticercosis may be seen in clinical practice. A thorough evaluation of all organ systems is essential to exclude the involvement of the brain, spinal cord, heart, eyes, skeletal muscles, etc. In this case report, we describe an asymptomatic cysticercosis patient who presented to us for cardiac surgery.
cysticercosis; soft tissue; asymptomatic; cardiac surgery
Introduction
Cysticercosis is a parasitic infestation caused by ingestion of the pork tapeworm Taenia solium eggs. With an estimated worldwide prevalence of more than 50 million infected persons, the disease is endemic in Mexico, Central and South America, and parts of Africa, Asia, and India.1 Cysticerci can lodge in the brain, spinal column, eyes, heart, skeletal muscle, and subcutaneous tissues with the brain being the most common organ affected. Asymptomatic soft tissue cysticercosis, however, is uncommon and usually involves the skeletal muscles of the limbs or subcutaneous planes.2 Here, we describe a case of asymptomatic soft tissue cysticercosis who presented to us for coronary artery bypass graft (CABG) surgery.
Case Report
A 72-year-old man, a farmer from the rural background of India was admitted to our institute for the treatment of coronary artery disease and unstable angina. All laboratory tests, electrocardiography, echocardiography, carotid Doppler scan, and peripheral vascular Doppler showed normal results. The chest radiograph, however, showed multiple “rice-grain” like ovoid calcified lesions in the chest wall, upper extremities, and neck giving it a “starry-sky” appearance (Figure 1).
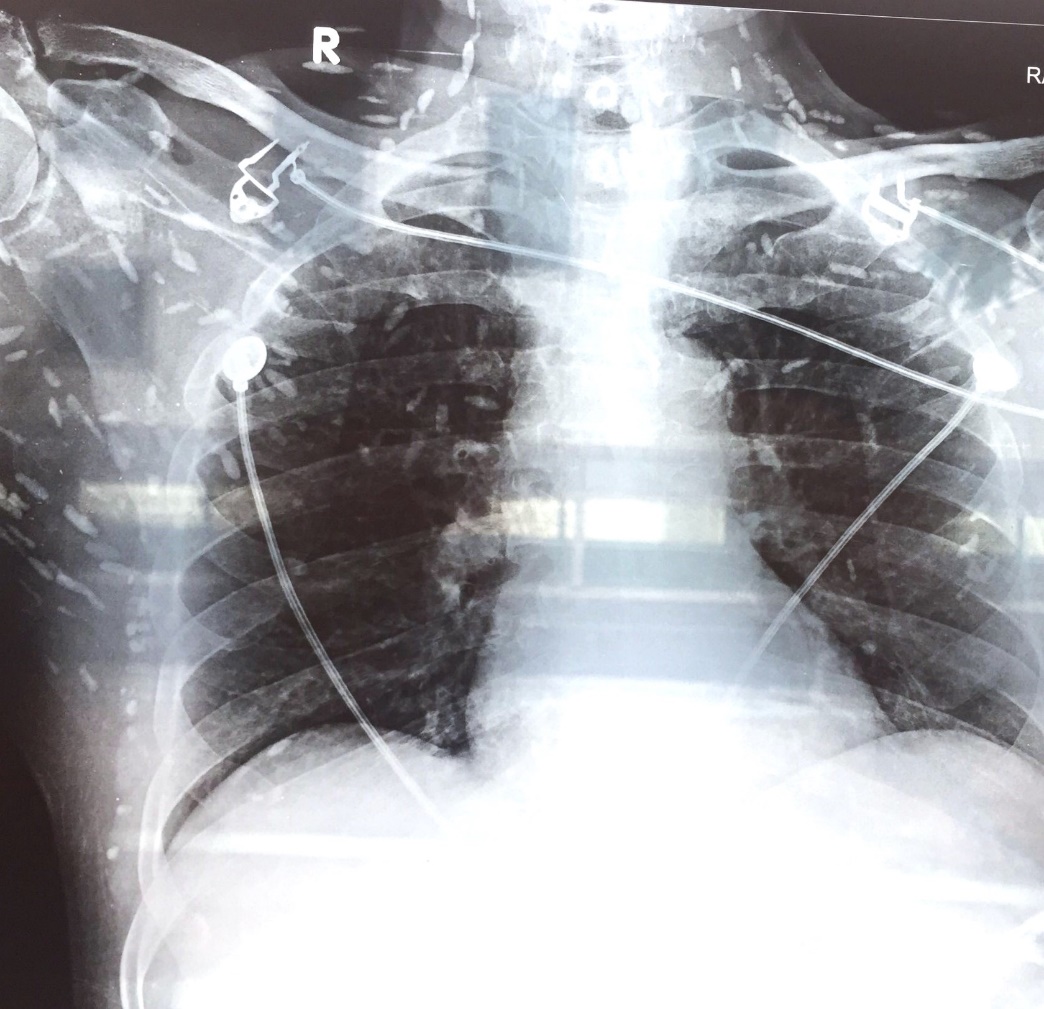
Figure 1: Chest radiograph showing multiple “rice-grain” like ovoid calcified lesions in the chest, upper extremities, and neck
During a detailed investigation, the patient described the presence of multiple, painless subcutaneous nodules in the chest and upper limbs for more than three decades. The patient did not undergo any investigation and denied any treatment taken as the nodules never troubled him. With a strong clinical suspicion of cysticercosis, a whole-body magnetic resonance imaging (MRI) was performed, which excluded the involvement of the brain, eyes, heart, spinal cord, and all other major organs. The patient underwent CABG surgery uneventfully with a smooth postoperative course. The diagnosis of cysticercosis was confirmed by the surgical excision biopsy from one of the lesions in the chest wall muscle. No antiparasitic treatment was offered to the patient given his asymptomatic status and non-involvement of other organs. A stringent follow-up was advised to exclude other organ involvement in the future.
Discussion
Cysticercosis is the most common parasitic infestation with humans as dead-end hosts after ingestion of Taenia solium eggs from contaminated food. The brain is affected in 60-90% of the cases, and neurocysticercosis can present with fever, headache, nausea, vomiting, altered mental status, and seizures. Cerebrovascular complications of cysticercosis include encephalitis, hydrocephalus, ischemic infarctions, or hemorrhage.3 Clinically, it can produce massive cerebral edema if treated with anthelmintics alone. Concomitant use of steroids is recommended to limit cerebral edema and to control seizures. Ocular manifestations, seen in 10-30% of patients, can be found in the subretinal space or vitreous humor and can threaten vision through inflammation of degenerating cysts or retinal detachment.4 Skeletal muscle or subcutaneous cysticercosis can cause localized pain and nodules. The most common location for soft-tissue cysticercosis is the skeletal muscles of the upper extremities.5 The differential diagnosis of soft tissue cysticercosis includes lipoma, epidermoid cyst, abscess, pyomyositis, tuberculous lymphadenitis, neuroma, neurofibroma, sarcoma, myxoma, ganglion, or fat necrosis.
History of travel to or emigration from an endemic area should raise the suspicion of cysticercosis. Computed tomography (CT) and MRI of the brain are the first-line modalities for the diagnosis of neurocysticercosis.6 MRI has the advantage of avoiding the hazards of radiation and intravenous contrast. In endemic areas, where disseminated cysticercosis is more common, a whole-body MRI can be a valuable tool to assess the entire burden of the disease and guide the therapy. CT and ultrasonography are highly sensitive for the detection of ocular and extraocular muscle involvement as they can demonstrate an eccentric echogenic scolex in the cysticercus.7 Serologic tests including enzyme-linked immunoblot assay and enzyme-linked immunosorbent assay can detect cysticercal antibodies depending on the cyst burden, location, and the phase of infection. Biopsy of the brain, skin, or muscle can provide a definitive diagnosis in an otherwise inconclusive clinical situation and may be the diagnostic method of choice for ocular, muscular, or subcutaneous cysts.1, 4
Cardiac cysticercosis is extremely rare and generally detected incidentally during cardiac surgery or autopsies. Inflammatory response of the myocardium can lead to myocarditis, granuloma formation, fibrosis, conduction abnormalities, or arrhythmias.8 Dung et al have recently reported a case of cysticercosis mass in the interventricular septum, protruding into the right ventricular chamber and requiring open-heart surgery.9 Spina et al have also reported myocarditis-like syndrome in a 24-year-old female, with transient left ventricular dysfunction due to cysticercosis.10 Other cardiac involvements reported in the literature include myocardial infarction, pericardial effusion, valvular pathology, atrioventricular block, atrial fibrillation, dilated cardiomyopathy, and heart failure. There is no consensus on the treatment of cysticercosis with cardiac involvement. Asymptomatic cardiac cysticercosis patients might not require anthelmintic therapy or intervention, given the benign nature of the disease. Surgical removal of the cyst may be required if there is compromised valvular apparatus, left/right ventricular outflow obstruction, or compression of epicardial coronary artery.
Treatment varies with the clinical presentation, and it must take into account multiple factors, including symptoms and the location, number, stage, and size of cysts. Parenchymal neurocysticercosis generally is treated with albendazole in conjunction with steroids to limit edema and with antiepileptic medications for seizure control. Ocular and extraocular muscle cysticercosis generally require surgical intervention. Skeletal muscle cysts are surgically removed only if painful.11 Because cysts can lodge in multiple locations, all patients with cysticercosis should have an ophthalmologic examination to rule out ocular involvement. Treatment of soft tissue and muscular cysticercosis depends on the symptoms and the location of the cysts. Isolated skeletal muscle or subcutaneous cysticercosis, such as described here, requires no specific treatment unless it is painful, and then simple excision may be required.11 The strategies to prevent and control cysticercosis include reduction in the spread of Taenia solium infection by decreasing pork-tapeworm carriers, eliminating exposure of pigs to human feces, and developing a vaccine against the parasite.12
In conclusion, asymptomatic soft tissue cysticercosis does not require any treatment unless it is painful. A regular follow-up is recommended to exclude the involvement of major, vital organs.