
Rahul Krishna Reddy1*, Arun Murari2, Ronal Kumar3, Akhtar Ali4, Livai Lutunaika5,
Yogeshni Devi Chandra6
1Surgical Registrar, Lautoka Aspen Hospital, Lautoka City, Fiji.
2 Associate Professor of Surgery/ Consultant, Lautoka Aspen Hospital, Lautoka City, Fiji.
3Consultant Surgeon, Lautoka Aspen Hospital, Lautoka City, Fiji.
4Consultant Surgeon, Lautoka Aspen Hospital, Lautoka City, Fiji.
5Consultant Surgeon, Lautoka Aspen Hospital, Lautoka City, Fiji.
6Consultant Internal Medicine, Lautoka Aspen Hospital, Lautoka City, Fiji.
*Corresponding authors: Rahul Krishna Reddy, Department of Surgical Registrar, Lautoka Aspen Hospital, Lautoka City, Fiji.
Received Date: February 20,2024
Accepted Date: February 26, 2024
Published Date: February 29 ,2024
Citation: Rahul K Reddy, Murari A, Kumar R, Ali A, Lutunaika L, Yogeshni D Chandra, (2024). “Characteristics and Outcomes of Acute Appendicitis at Lautoka Aspen Hospital, Fiji:An Observational Retrospective Study (09/22 – 09/23). Clinical Research and Clinical Case Reports, 5(1); DOI: http;//doi.org/08.2024/1.1076.
Copyright: © 2024 Rahul Krishna Reddy. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background:
Acute appendicitis is a surgical emergency characterized by symptoms due to the
inflammation of the vermiform appendix. Delay in treatment increases the incidence of complications.
Method:
An observational retrospective cohort study of all patients who had undergone open appendectomy with the diagnosis of appendicitis from 1st September 2022 till 1st September 2023.
Results:
Majority of the patients were in age range of 11 – 30 years of age (50.5%) with male predominance (56%). The mean duration of symptoms was more than 2 days. The most common presenting symptom was localized right quadrant pain (59%) while right lower quadrant direct tenderness was the most common sign (94%). Abdominal ultrasound was done for most patients (92%) with sensitivity and specificity of 81% and 33.3% respectively. Majority of patients had complicated appendicitis (60%) with negative appendectomy rate of 7%. The mean duration of hospitalization was 4.61 days. Complication rate of this study was 23.5% with surgical site infection being the most common (19%). The mortality rate for this study was 0%.
Conclusion:
Acute appendicitis was the most common cause of abdominal surgery with a high prevalence rate in young adults. Abdominal ultrasound was done in the majority of the patients as supplementary imaging for the diagnosis of acute appendicitis. Empirical antibiotic treatment was given to all patients. Complicated appendicitis was the most common intraoperative finding while the most common complication was surgical site infection.
acute appendicitis; complicated appendicitis; open appendectomy; Lautoka Hospital; clinical presentation; complications; outcomes
Background:
Acute appendicitis is an acute inflammation of the vermiform appendix, almost always due to obstruction of the lumen of the appendix (by fecalith, normal stool, infective agents, or lymphoid hyperplasia). (1) Appendicitis is the most common cause of acute abdomen surgery. Despite its commonness and the abundance of literature on the subject, its diagnosis remains challenging. Delay in intervention results in complications, leading to increased morbidity and mortality. (2)(1) Diagnosing acute appendicitis accurately and efficiently can reduce morbidity and mortality. Thorough history-taking and physical examination can aid in the diagnosis of acute appendicitis. Clinical presentations such as right lower quadrant pain, abdominal rigidity, and periumbilical pain radiating to the right lower quadrant, fever, anorexia, vomiting, nausea, guarding, rebound tenderness, a positive psoas sign, a positive obturator sign, and a positive rovsing sign are most reliable for diagnosing acute appendicitis. (3)(4) Appendicitis is traditionally a clinical diagnosis. However, laboratory measurements, including total leucocyte count, neutrophil percentage, and C-reactive protein (CRP) concentration, are usually, part of the diagnostic blood workup. (3) Imaging modalities such as abdominal ultrasonography and abdominal CT scan are used to proceed with the diagnostic steps, especially in cases of atypical presentation in children and females of reproductive age when clinical evaluation only may not be adequate to differentiate acute appendicitis from other abdominopelvic pathologies. (2) Although conservative management is described to be effective in some centers, the gold standard management for acute appendicitis remains appendectomy. (5) Laparoscopic appendectomy is superior to open appendectomy in terms of wound site infections and post-operative recovery. (6) (7) As an institution in a low-income country, our hospital is still developing a facility for laparoscopic appendectomy and hence all procedures included in this study were open procedures. The complications associated with appendicitis are increased in cases of delayed presentation.(8) The risk of appendiceal perforation within 36 hours ranges from 16% to 36%, with the risk of perforation increasing by 5% every 12 hours. This highlights the importance of timely diagnosis and treatment. (9) This study aimed to determine the characteristics and outcomes of acute appendicitis in Lautoka Aspen Hospital, in terms of socio-demographic data, clinical presentations, duration of symptoms, diagnostic investigations, empirical antibiotics treatment regimes, duration of hospitalization, intraoperative findings, histological findings, complications, and outcomes. This is the first retrospective cohort study done in Fiji on this subject.
Method:
Study Setting:
This study was conducted in Lautoka Aspen Hospital which is located in Lautoka city, in the Republic of Fiji Islands. This hospital was the first public hospital built in the western division. The 305-bed Lautoka Aspen Hospital serves more than 330000 people living in the western division. It also serves as a teaching hospital with affiliations to Fiji National University (college of Medicine, Nursing & Health Sciences) and The University of Fiji (Umanand Prasad School of Medicine & Health Sciences).
Study Design and Participants:
This is a retrospective observational study of patients diagnosed with acute appendicitis at Lautoka Aspen Hospital from 1st September 2022 to 1st September 2023. Patients were followed from the time of evaluation at the emergency department to the day of final assessment at the Surgical Clinic 6-8 weeks after discharge from the Hospital. Inclusion criteria included all patients diagnosed and operated on with the diagnosis of acute appendicitis. Patients with other pathological intraoperative findings and insufficient data were excluded from the study.
Data Collection Techniques and Instruments:l
Names and NHN of all patients who had open appendectomy from September 2022 to September 2023 were collected from Operation theatre registers. Data collected was then submitted to the records department and folders were retrieved. Each folder was thoroughly examined by the primary investigator and data including socio-demographic data, clinical presentations, duration of symptoms, diagnostic investigations, empirical antibiotics
treatment regimens used, intraoperative findings, histological findings, duration of hospitalization, complications, and outcomes were retrieved.
Data Analysis and Presentation:
Data was collected and analyzed in Microsoft Excel, and presented as both frequency and percentage for discrete variables. The presence of an association between several independent patient variables and the development of complications was assessed by a chi-square analysis considering a confidence interval of 95% and a P value of <0.05 was considered significant in all computations.
Results:
A total of 217 patients were evaluated at the Emergency Department of Lautoka Hospital with a diagnosis of acute appendicitis based on clinical, laboratory, and imaging parameters in the study period and all underwent surgery.
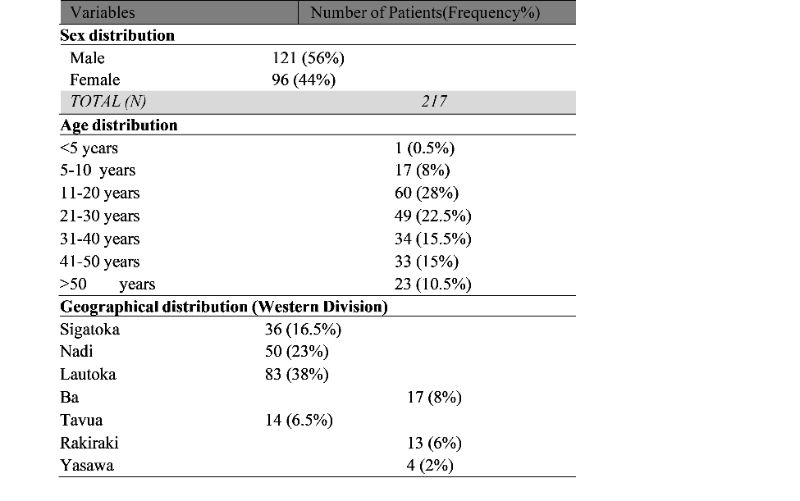
Socio-demographic Characteristics:
The gender distribution of the patients in our study was 56% male and 44% female with the male to female ratio of 1.27: 1. Majority of the patients belonged to the age group of 11-20 years. As for the geographical distribution, the majority of the patients (38%) came from
Lautoka City [Table 1]
Table 1: Sociodemographic Data:
Clinical Presentation:
Majority of the patients (37%) presented after 48 hours of duration of symptoms. The most common presenting symptom was localized right lower quadrant pain, 129 (59%), followed by vomiting, 97 (45%), and anorexia 96 (44%). The most common physical sign was direct tenderness, 204 (94%), followed by voluntary guarding, 153 (71%), and rebound tenderness, 132 (61%). During initial evaluation at primary health care facilities or during admission to the emergency department, 65 (30%) of the patients were tachycardic while, 97 (45%) were febrile [Table 2].
Investigation:
All patients had blood workups done during initial evaluation or admission. Leucocytosis was seen in 162 (75%) patients while 142 (65%) had neutrophil left shift. [Table 3] An abdominal ultrasound scan was done for 200 (92%), out of which 25 (12%) had other pathology. Among patients who had intraoperative findings of simple and complicated appendicitis, 33 (15%) were reported to have normal ultrasound, and 25 (20%) were reported to have other
pathology [ Table 3]. The sensitivity of abdominal ultrasound in this study was 81% while the specificity was 33.3%.
Table 2: Results of Clinical Findings:
|
Parameters |
Number of Patients (Frequency%) |
Symptoms
|
Migratory pain |
44 (20%) |
|
Localised right quadrant pain |
129 (59%) |
|
Localized peri-umbilical pain |
9 (4%) |
|
Generalized abdominal pain |
41 (19%) |
|
Anorexia |
96 (44%) |
|
Nausea |
66 (30%) |
|
Vomiting |
97 (45%) |
|
Loose bowel motion |
40 (18%) |
|
Dysuria |
21 (10%) |
Duration of Symptoms
|
24 hours |
72 (33%) |
|
48 hours |
65 (30%) |
|
>48 hours |
80 (37%) |
Physical Examination
|
Direct tenderness |
204 (94%) |
|
Rebound tenderness |
132 (61%) |
|
Voluntary guarding |
153 (71%) |
|
Rovsing sign |
86 (40%) |
|
Psoas sign |
26 (12%) |
|
Obturator sign |
9 (4%) |
Vitals
|
Heart rate >100 (Tachycardia) |
65 (30%) |
|
Febrile (T >37.3 degrees Celsius) |
97 (45%) |
Table 3: Investigations:
|
Variables |
Number of Patients (Frequency%) |
Lab - Bloods
|
Leucocytosis (white cell count >10000) |
162 (75%) |
|
Neutrophil shift >75% |
142 (65%) |
Radiology – Abdominal ultrasound
|
Definite Appendicitis |
66 (30%) |
|
Probable Appendicitis |
75 (35%) |
|
Normal Appendix |
34 (15.5%) |
|
Other Pathology |
25 (12%) |
|
Not done |
17 (7.5%) |
Antibiotic Treatment:
All patients in this study were started on intravenous antibiotics on initial evaluation at a primary health care facility or during admission at the emergency department in Lautoka Aspen Hospital. Patients continued intravenous antibiotics during the entire duration of hospitalization and switched to oral antibiotics upon discharge [Table 5].
Table 4: Distribution of Empirical Antibiotic treatment for Acute Appendicitis:
|
Antibiotics |
Number of Patients (Frequency%) |
|
Ampicillin + Gentamicin |
83 (38%) |
|
Cloxacillin + Gentamicin |
6 (3%) |
|
Chloramphenicol + Gentamicin |
3 (1%) |
|
Cloxacillin + Metronidazole |
5 (2%) |
|
Ampicillin + Metronidazole |
2 (0.5%) |
|
Ceftriaxone + Metronidazole |
10 (5%) |
|
Ampicillin + Ceftriaxone |
- |
|
Cloxacillin + Ceftriaxone |
2 (0.5%) |
|
Ampicillin + Gentamicin + Metronidazole |
77 (36%) |
|
Cloxacillin + Gentamicin + Metronidazole |
20 (10%) |
|
Ampicillin + Ceftriaxone + Metronidazole |
2 (1%) |
|
Cloxacillin + Ceftriaxone + Metronidazole |
3 (1%) |
Intraoperative Findings:
The most common abdominal incision used was Gridiron incision in 174 (80%) of the
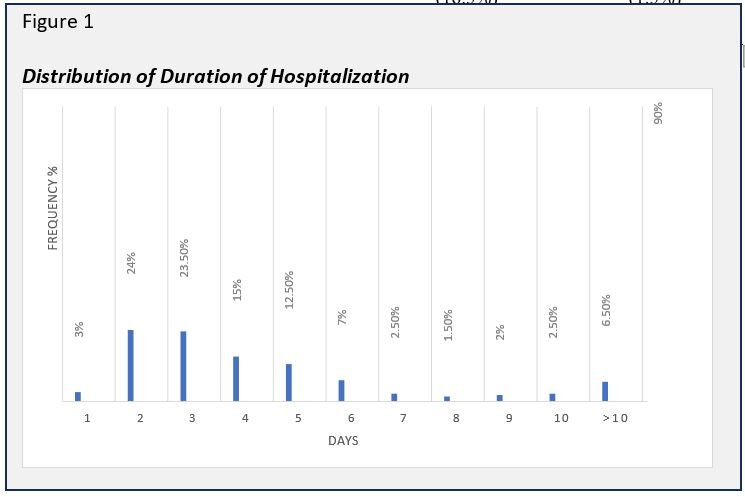
patients followed by midline incision, in 28 (13%), and Lanz incision in 15 (7%). The type of incision was determined by the operating surgeon based on clinical and radiological findings [Table 5].Simple appendicitis accounted for 81 (37.5%) while 131 (60%) were at the complicated stage. Five patients (2.5%) had normal appendix [Table 5]. Majority of patients, 103 (47.5%) who presented 24 hours after the onset of symptoms had complicated appendicitis [Table 6].Of all patients who had abdominal ultrasound done, 66 (30%) were reported to have definite appendicitis and, 74 (34%) were reported to have probable appendicitis [Table 7]. Patients with Alvarado scores of 7-10 had the highest number of complicated appendicitis 72 (33%) [Table 8].All appendectomies were done by general surgery registrars. All specimens were sent for histopathological analysis. The mean duration of hospitalization was 4.61 days [Figure 1].
Table 5: Results of Intra-operative Findings:
|
Variables |
Number of Patients (Frequency%) |
Types of Incision
|
Gridiron |
174 (80%) |
|
Lanz |
15 (7%) |
|
Midline |
28 (13%) |
Intra-operative stage of Appendicitis
|
Simple Appendicitis |
81 (37.5%) |
|
Complicated Appendicitis |
131 (60%) |
|
Normal Appendix |
5 (2.5%) |
Specimen
|
Pus Swab |
20 (9%) |
|
Appendix (histology) |
217 (100%) |
Table 6: Duration of symptoms vs. intra-operative stages of Appendicitis:
|
Duration of Symptoms (Hours) |
Complicated Appendicitis N (%) |
Simple Appendicitis N (%) |
Normal Appendix N (%) |
|
24 hours |
28 (13%) |
31 (14%) |
1 (0.5%) |
|
48 hours |
31 (14.5%) |
27 (12.5%) |
3 (1.5%) |
|
>48 hours |
72 (33%) |
23 (10.5%) |
1 (0.5%) |
Table 7: Investigations Vs Intra-operative Stages of Appendicitis:
|
Investigations |
Simple Appendicitis N (%) |
Complicated Appendicitis N (%) |
Normal Appendix N (%) |
Total |
Lab - Bloods
|
Leucocytosis (WCC >10000) |
56 (26%) |
106 (49%) |
- |
62(75%) |
|
Neutrophil shift >75% |
44 (20%) |
98 (45%) |
- |
142(65%) |
Radiology – Abdominal ultrasound
|
Definite Appendicitis |
17 (8%) |
49 (22%) |
- |
66 |
|
Probable Appendicitis |
32 (15%) |
41 (19%) |
2 (1%) |
75 |
|
Normal Appendix |
14 (6%) |
19 (9%) |
1 (0.5%) |
34 |
|
Other Pathology |
10 (5%) |
15 (7%) |
- |
25 |
|
Not done |
8 (3.5%) |
7 (3%) |
2 (1%) |
17 |
|
Total |
81 |
131 |
5 |
217 |
Table 8: Alvarado Score Vs Intra-operative stages of Appendicitis:
|
Alvarado Score |
Simple Appendicitis N (%) |
Complicated Appendicitis N (%) |
Normal Appendix N (%) |
|
1-4 |
23 (10.5%) |
23 (10.5) |
2 (1%) |
|
5-6 |
24 (11%) |
36 (16.5%) |
3 (1.5%) |
 Histological Findings:
Histological Findings:
Histology results showed acute appendicitis in 94 patients (43%), followed by necrotizing appendicitis in 23 patients (11%) and resolving appendicitis in 20 patients (9%). The negative appendectomy rate for this study was 7%.
Outcomes:
Post-operative complications developed in 51 (23.5%) of the patients, the commonest being surgical site infection in 41 (19%), followed by paralytic ileus in 7 (3%), Atelectasis in 2
(1%) and incisional hernia in 1 (0.5%). Readmission was required in 3 (1.5%) patients [Table 10]. Relaparotomy was required in 1 (0.5%) patient. One patient who was operated on for complicated appendicitis developed wound dehiscence and multiple debridement was required. The mortality rate in this study was 0%. All patients with surgical site infection had wound swabs taken. The most common organism cultured from the swabs was Escherichia coli (60%) followed by Acinetobacter baumanii (17%) [Table 11]. According to the frequency of organisms by their sensitivity test, Gentamicin was noted to be most effective, followed by Co-clotrimazole and Chloramphenicol [Figure 2].
Table 9: Distribution of Histological Findings:
|
Variables |
Number of Patients (Frequency%) |
|
Acute appendicitis |
94 (43%) |
|
Gangrenous appendicitis |
2 (1%) |
|
Necrotising appendicitis |
23 (11%) |
|
Perforated appendix |
7 (3%) |
|
Suppurative appendicitis |
23(11%) |
|
Appendiceal diverticulum |
1 (0.5%) |
|
Enterobius vermicularis infestation |
2 (1%) |
|
Fecolith |
14 (6%) |
|
Focal peri appendicitis |
8 (4%) |
|
Reactive lymphoid hyperplasia |
1 (0.5%) |
|
Appendiceal mass/abscess |
7(3%) |
|
Resolving appendicitis |
20 (9%) |
|
Normal appendix |
15 (7%) |
Table 10: Outcome post-Open Appendectomy:
|
Variables |
Number of Patients (Frequency%) |
|
ICU admission |
1 (0.5%) |
|
Mortality |
- |
Complications
|
Surgical site infection (SSI) |
41 (19%) |
|
Respiratory (Atelectasis) |
2 (1%) |
|
An abscess (pelvic) |
- |
|
Portal pyemia |
- |
|
Ileus (paralytic) |
7 (3%) |
|
Faecal fistula |
- |
|
Hernia (incisional) |
1 (0.5%) |
|
Obstruction |
- |
|
Thrombus (DVT) |
- |
Table 11: Microbiological Profile from Surgical Site Infection Post Appendectomy:
|
Variables |
Number of Patients (Frequency%) |
|
Escherichia coli (E. coli) |
18 (60%) |
|
Acinetobacter baumanii |
5 (17%) |
|
Pseudomonas aeruginosa |
2 (7%) |
|
Staph aureus |
1 (3%) |
|
Klebsiella pneumoniae |
3 (10%) |
|
Morganella morganii |
1 (3%) |
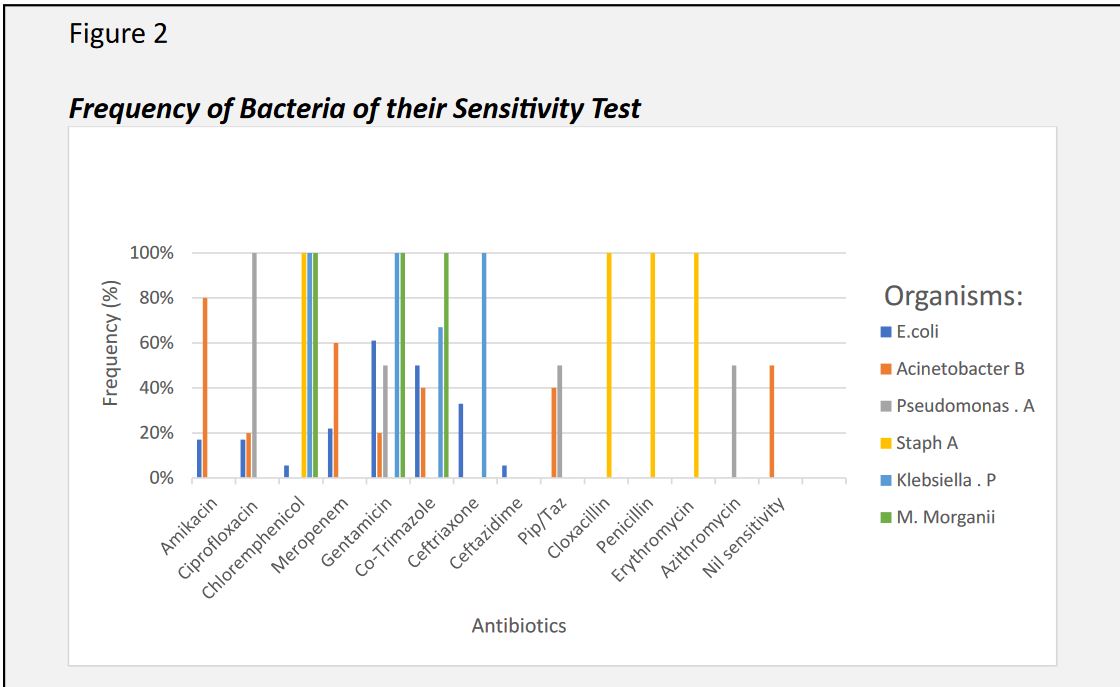
Figure 2: Frequency of Bacteria of their Sensitivity Test
Discussion:
This study aimed to understand the characteristics of acute appendicitis in the Fijian population and audit the outcomes. From 1st September 2022 to 1st September 2023, a total of 217 patients were operated on at Lautoka Aspen Hospital with the diagnosis of acute appendicitis. The most prevalent age ranges were between 11 – 20 years (28%) and 21- 30 years (22.5%) respectively. Male predominance was noted in the gender distribution of the study population, with a male-to-female ratio of 1.27:1. These findings were similar to studies done in other countries. (2)(9) The geographical distribution of patients is an important factor considering the logistics issues faced by patients which in turn contributes to delayed presentation. The mean duration of symptoms was more than 2 days in this study, association between the duration of symptoms and the presence of complicated appendicitis was found to be significant (p <0.05). Majority of the patients presented with localized right lower quadrant pain, 129 (59%) compared to the typical migratory type of abdominal pain as compared to other studies. (1)(2)(9) The most common physical finding was direct tenderness at the right lower quadrant, 204 (94%) which was also common in other studies. (2-4) Leucocytosis was seen in 75% of our patients while 65% had neutrophil left shift, which is similar when compared to other studies. (2)(3)(12) Although the diagnosis of appendicitis is mostly clinical, abdominal ultrasound was done in 200 (92%) of our patients. Supplementary imaging study is recommended by many studies as clinical evaluation may not be adequate to differentiate acute appendicitis from other abdominal pathologies. From our observation, majority of our patients had an abdominal ultrasound done in primary health care facilities as part of a diagnostic process before their referral to our hospital or upon arrival at the emergency department of our Lautoka Aspen Hospital. As more studies support the use of imaging modalities, physicians nowadays have made abdominal ultrasound part of their diagnosis process. This practice is encouraged as perioperative imaging has decreased negative appendectomy rates and also reduces misdiagnosis of appendicitis with other pathologies. (10)(11) Empirical antibiotic treatments were started in all patients diagnosed with acute appendicitis either at primary health care facilities or at the emergency department of our hospital. Although all patients were started on antibiotics, only 36% of patients received the recommended antibiotics (Ampicillin + Gentamicin and Flagyl) as per Fiji antibiotics guidelines. (15) The most common incision used for appendectomy in this study was Gridiron incision, in 174 (80%) patients. Complicated appendicitis was found in 60% of the patients which is higher in comparison to other studies. (2) The high rate of complicated appendicitis may reflect the lack of timely health-seeking behaviour of our local population. Normal-looking appendix was found in 2.5% of the patients based on the operating surgeon’s assessment. All specimens were sent for histopathological analysis. The negative appendectomy rate for this study was less than 10% which was similar when compared to other studies. (16)(17) The complication rate in this study was found to be 23.8%. The most common postoperative complication was surgical site infection, 19%. These findings were significantly higher when compared to similar studies. (1)(2)(3)(7) The high rates of surgical sites can be attributed to nosocomial infections due to non-compliance to infection prevention and control (IPC) measures in our hospital. The relaparotomy rate for this study was 0.5 % with a mortality rate of 0%, which was significantly lower compared to other studies. (1)(2)(3)(7) Microbiological profile and sensitivity of organisms cultured from infected surgical site wounds do suggest nosocomial infections of wounds and inappropriate use of antibiotics.
Recommendations:
The findings of this study suggest a high prevalence of appendicitis in young adults thus disease education and awareness would contribute greatly to instilling time health-seeking behaviour. A review of the current antibiotic guidelines for the treatment of acute appendicitis is highly recommended. The findings of this study show that Ampicillin recommended in the Fiji antibiotic guideline for the treatment of appendicitis have no sensitivity to the organisms found in infected surgical wounds which may be a contributing factor to increased Surgical site infection rate. This study also suggests that most organisms cultured from wound swabs are nosocomial bugs thus strict implementation and adherence to infection prevention and control (IPC) measures would help limit nosocomial infections.
Limitations:
This study was conducted retrospectively thus the problems faced included a lack of sufficient information on patients' files and less detailed records of patient’s investigations. Since this was a single-centre study, more studies are required to fully solidify the characteristics of acute appendicitis and its outcome on our population.
Conclusion:
Acute appendicitis was the most common cause of abdominal surgery. In our study, we found that appendicitis has a high prevalence rate in young adults predominantly males. Abdominal ultrasound was used for the majority of the patients for the diagnosis of acute appendicitis.
Empirical antibiotic treatment was given to all patients in this study. The majority of patients had complicated appendicitis as their intraoperative finding. The most common post-
operative complication was surgical site infection. The negative appendectomy rate of this study was less than 10%. The most common organism found in the wound swabs was noted to be E. coli. The mortality rate for this study was 0%.
Declarations:
Ethical Consideration:
Permission to conduct the study was received from the HCF Research Unit of Lautoka Hospital and the Fiji Human Health Research and Ethics Committee.
Consent of Participation:
No written consent was taken since the information used in this study does not include any identifying information from the patient.
Availability of Data and Materials : : Not applicable.
Competing Interests:
The authors declare that they have no competing interests.
Funding: No funding was received for this work
Authors Contribution:
RKR: conception, design, data collection, analysis and interpretation, manuscript preparation, and editing.
AM: supervision and review of manuscript RK: supervision and review of the manuscript AA: supervision and review of manuscript YC: review of manuscript
LL: review of manuscript
Final approval of the manuscript is done by all authors.