Clinical Research and Clinical Case Reports
OPEN ACCESS | Volume 7 - Issue 1 - 2026
ISSN No: 2836-2667 | Journal DOI: 10.61148/2836-2667/CRCCR
Gabriela Alacarini Farina 1, Karen Dantur Batista Chaves 2, Maria Cristina Munerato 3*
1Stomatology Residence Service, Hospital de Clínicas de Porto Alegre (HCPA), Porto Alegre/RS, Brazil.
2Conservative Dentistry Department, Dentistry College, Universidade Federal do Rio Grande do Sul (UFRGS), Porto Alegre/RS, CEP 90035-003, Brazil.
3Conservative Dentistry Department, Dentistry College, Universidade Federal do Rio Grande do Sul (UFRGS), Porto Alegre/RS, CEP 90035-003, Brazil.
*Corresponding authors: Maria Cristina Munerato, Conservative Dentistry Department, Dentistry College, Universidade Federal Do Rio Grande Do Sul (UFRGS), Porto Alegre/RS, CEP 90035-003, Brazil.
Received: November 24, 2021
Accepted: December 06, 2021
Published: December 10, 2021
Citation: Gabriela Alacarini Farina, Karen Dantur Batista Chaves, Maria Cristina Munerato (2021) “Giant Papillae Tongue Disorder: Case Report with Six Years of Follow-Up”. Clinical Research and Clinical Case Reports, 2(4); DOI: http;//doi.org/12.2021/1.1044
Copyright: © 2021 Maria Cristina Munerato. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background:
Patients submitted to liver transplant in childhood present prolonged survival, which allows identifying oral health changes associated with immunosuppression and immunosuppressant therapy. In due course, patients that are prescribed tacrolimus present oral cavity changes that, by exclusion, were considered adverse effects of the drug. The giant papillae tongue disorder (GPTD) comprises a set of alterations in the buccal mucosa that may develop in organ-transplanted infants who chronically use the drug tacrolimus.
Case Summary:
A 10-year-old male patient was referred to the Stomatology Unit of HPCA presenting fissured tongue that had started six months prior to the consultation. Medical records of the patient included two liver transplants. The immunosuppression protocol, including tacrolimus, was maintained from the first transplant at 14 months of age until the patient was 15 years old, when tacrolimus was replaced by sirolimus. The intraoral examination revealed the presence of polypoid hyperplasia across the dorsum of the tongue, as well as other alterations in the oral cavity. This clinical picture progressed over three years. The anatomo-pathological results showed chronic inflammation. These results led us to conclude that the lesions observed resulted from the chronic use of tacrolimus. Five months after the discontinuation of tacrolimus perioral lesions improved partly. Currently, the patient remains under follow-up.
Conclusion:
Dentists should be part of a transdisciplinary team in organ transplantation. The role played by a dentist starts already before surgery in the effort to prevent any odontogenic infection soon after transplantation. After the procedure and during the prescription of immunosuppressant therapy, dental follow-up should be carried out aiming at preventing problems. Since the lesions induced by tacrolimus emerged late into the process, the dentist has to examine the oral cavity periodically in the search for GPDT characteristic lesions.
Core tip:
Giant papillae tongue disorder (GPTD) is characterized by granulomatous formations on the dorsum of the tongue associated with alterations in the buccal mucosa. GPTD manifests in liver-transplanted children who receive a tacrolimus-based immunosuppressive protocol. Oral lesions arise after some years of chronic use of this medication. Diagnosis is established through the exclusion of other oral granulomatous lesions. GPTD regresses with the replacement of tacrolimus by another immunosuppressant. The dentist, as part of the multidisciplinary team that manages transplanted patients, will make the diagnosis of oral lesions and the oral infections prevention that may put the health of the transplanted patient at risk.
Introduction:
Patients submitted to organ transplantation today benefit from prolonged survival due to technical advancements and the existence of medication used to prevent rejection [1]. Survival with no rejection is longer in patients taking tacrolimus when compared with that of patients prescribed cyclosporine as an immunosuppressant [1]. With longer survival rate, these patients exhibit changes in the oral cavity that have been associated with the state of permanent immunosuppression as well as the adverse side effects of the immunosuppressant therapy. The oral health in children who underwent any type of solid organ as well as allogeneic bone marrow transplantation, is affected by constant immunosuppression when both odontogenic and opportunistic infections may manifest if proper dental follow-up is not provided [2,3]. Concomitantly, immunosuppressants may eventually induce morphological changes across the whole oral mucosa. Changes in the oral mucosa such as cyclosporine A- and calcium channel blockers-induced gingival overgrowth have been extensively described in the literature [4,5]. However, few studies have addressed the effects caused by tacrolimus.
Oral cavity lesions caused by the chronic use of tacrolimus were described by Saalman et al. [6] Polypoid lesions on the dorsum of the tongue were the most ubiquitous, being present in all but one of the patients included in the study. The authors also observed the presence of fissures on the tongue and lips in addition to cobblestone appearance of the mucosa, angular cheilitis, lip edema, and dysgeusia. The period of time from the transplantation to the emergence of the first lesions varied between one and four years. Bouts of food allergies also coincided with the use of tacrolimus in these patients [6]. The literature review published by Petti et al. [7] described the occurrence of orofacial granulomatosis-like lesions (OGLL) as a new, rare nosologic entity observed in children who underwent liver or kidney transplantation and were given tacrolimus as immunosuppressant therapy. The description of these lesions was similar to that published by Saalman et al. [6]. Nevertheless, the mechanism through which tacrolimus induces these changes in oral mucosa remains unclarified [7]. This group of lesions has been described in patients who did not undergo transplantation and in individuals with Crohn’s disease (CD) or orofacial granulomatosis (OFG). The etiology and pathology of these diseases have been associated with inflammatory or immunologic factors, suggesting the predominance of Th1 cells (T helper (Th) lymphocytes produce cytokines mainly related to phagocytosis-mediated defense against intracellular infectious agents such as Interferon-gamma (INF-γ), IL-2 and Tumor Necrosis Factor-alpha (TNF-α)) [8,9].
This study describes the case of a pediatric patient with liver transplant who was diagnosed with Giant Papillae Tongue Disorder (GPTD) and used tacrolimus for 14 years. The patient was followed up for six years after the first consultation with a Stomatologist, and the use of the imunosupressant tacrolimus was discontinued in the last year after the diagnosis of GPTD. A literature review about GPTD was carried out in the PubMed databases using the keywords oral manifestation, hepatic transplant in children, tacrolimus, immunosuppressant, oral granulomatosis-like lesions, and giant papillae tongue disorder. This study was approved by the Committee for Ethics in Research of the Hospital de Clínicas de Porto Alegre (HPCA), Porto Alegre, Rio Grande do Sul, Brazil (permission number 160129). The custodian of the patient signed an informed consent form.
Case Report:
Chief Complaints and History of Present Illness:
A 10-year-old male patient was referred to the Stomatology Unit of HPCA presenting fissured tongue that had started six months prior to the consultation at the Stomatology Unit.
History of Past Illness:
Medical records of the patient included two liver transplants. The first transplant was carried out when he was 14 months of age and the second one when he was 3 years old. The immunosuppressant therapy included tacrolimus, prednisone, cyclosporine, and mycophenolate mofetil. The immunosuppression protocol was maintained from the first transplant at 14 months of age until the patient was 15 years old, when tracolimus was replaced by sirolimus.
Physical Examination:
The intraoral examination revealed the presence of polypoid hyperplasia across the dorsum of the tongue (Fig. 1a). Angular cheilitis and dry vermillion presenting scaling were noticed across the perioral skin region (Fig. 1b). The patient exhibited papillomatous hyperplasia across the mucosa of the hard palate (Fig. 1c) and cobblestoning appearance of the mucous membrane (Fig. 1d, e, f, g, h). These lip fissures were similar to those observed in lip licker’s dermatitis. This clinical picture progressed over three years. The first signs of changes in the tongue were observed at the age of four (one year after the second transplant), though the patient visited a Stomatologist only at the age of 10. Upon the first examination, the lesions on the oral mucosa were already present. The other manifestations, which included lip licker’s dermatitis that spread to the perioral region and angular cheilitis, had evolved during the follow-up conducted by the Stomatologist in the following three years. The diagnosis hypotheses were granulomatous disease and lesions caused by the chronic use of tacrolimus. Despite the morphological changes in the dorsum of the tongue, the patient did not report dysgeusia.
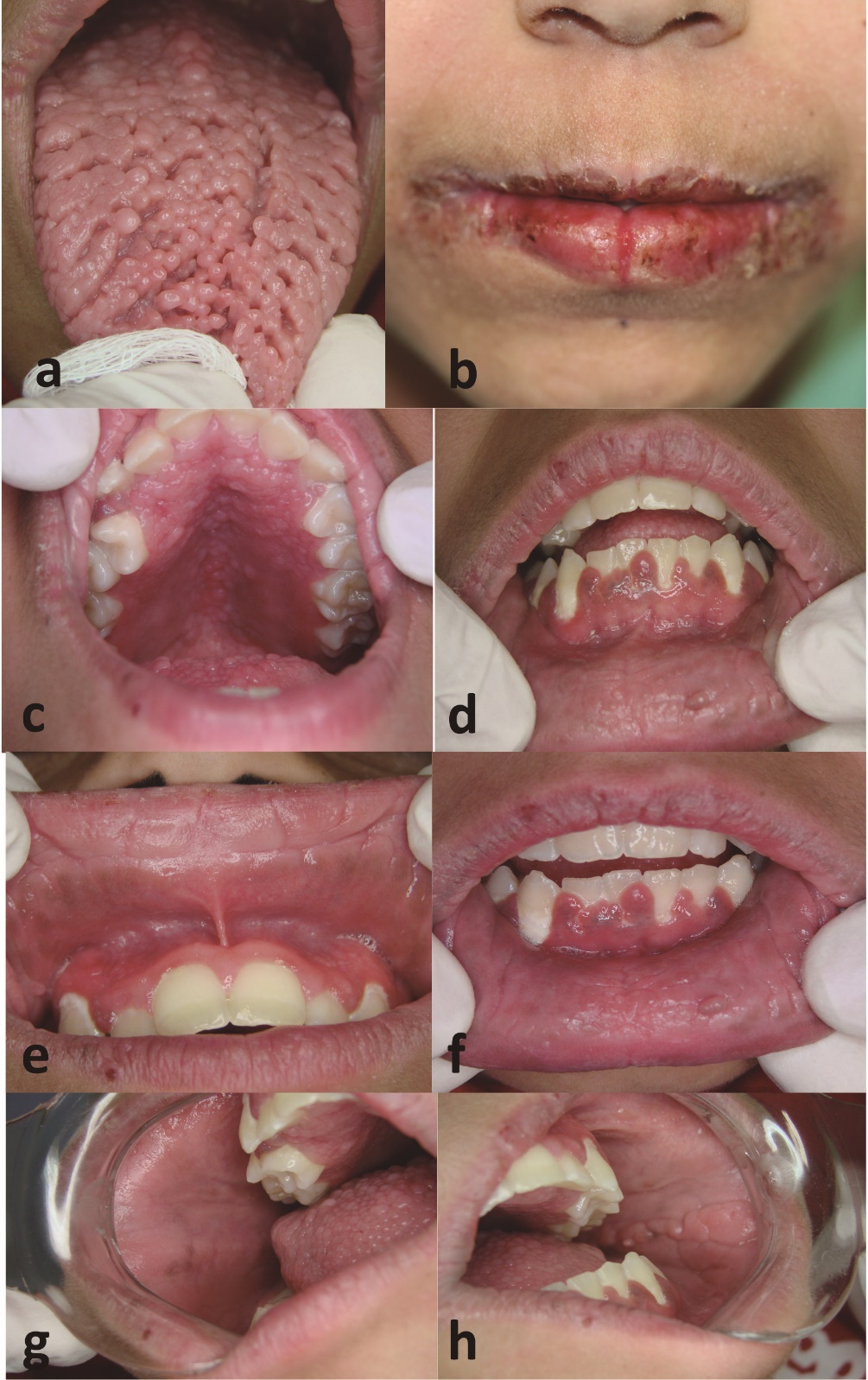
Figure 1: Clinical aspect of the oral cavity of the patient during the use of tacrolimus. a: Mucosa of the dorsum of the tongue with polypoid manifestations; b: dry lips with scaling, fissures, and angular cheilitis; c: mucosa of the hard palate with papillomatous hyperplasia; d: gingival overgrowth (vestibular aspect from anterior lower teeth); e, f, g, h: cobblestone appearance upper and lower lip mucosa and bilateral mucous membrane.
Histopathological Examinations:
Two biopsies were conducted, one on the mucous lining of the lower lip and one on the polypoid hyperplasia located in the dorsum of the tongue. The anatomo-pathological results for the lip mucosa were chronic inflammation with acanthosis, papillomatosis and parakeratosis of the squamous mucosa. In addition, the diagnosis of the sample of the dorsum of the tongue was papillomatous epithelial hyperplasia with mild chronic inflammation (Fig. 2).
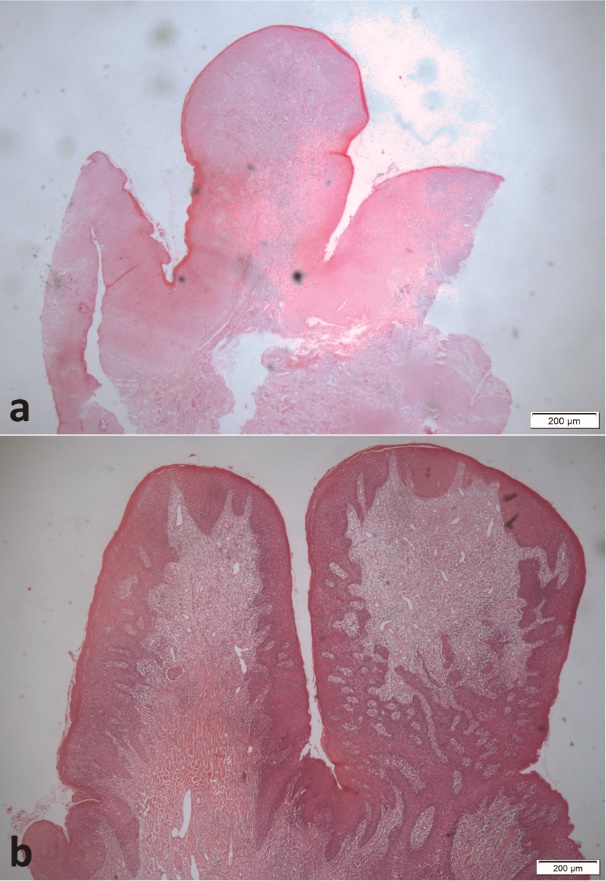
Figure 2: a: Microphotograph of the lower lip mucosa sample and; b: polypoid manifestations on the dorsum of the tongue. (200x, hematoxylin-eosin)
Final Diagnosis:
These results led the stomatology team to conclude that the lesions observed resulted from the chronic use of tacrolimus.
Treatment:
In 2015, when the patient was 14 years old, the medical team changed the immunosuppressant therapy in an effort to reduce the administered doses of tacrolimus. The initial dose was 1 mg 12/12h and it was decreased to 1mg/day. The use of tacrolimus was totally discontinued four months after its dose reduction. However, this initiative worsened the patient’s liver status. In the meantime, the patient exhibited new, pruritic, purple lesions across the skin of limbs and body that resembled Kaposi sarcoma lesions (Fig. 3). These lesions were also considered to result from the use of tacrolimus.
From this moment on, with so many lesions induced by tacrolimus that affected the patient’s quality of life so negatively, the medical team decided to change the treatment protocol once again, now discontinuing the immunosuppressant drug. The liver biopsy conducted four months later revealed acute moderate Rejection Activity Index (RAI = 6).
The new treatment protocol with immunosuppressant drugs included cyclosporine, everolimus, prednisone, and mycophenolate mofetil.

Figure 3: Lesions resembling Kaposi sarcoma on the back (bilateral, a, b), hand (c), and lumbar region (d).
Outcome and Follow-Up:
Five months after the discontinuation of tacrolimus skin lesions subsided completely, leaving behind a dark pigmentation on each lesion site. Perioral lesions also improved partly, while the cobblestone aspect of the jugal mucosa disappeared. The papillomatous hyperplasia on the palate did not disappear, and polypoid manifestations on the dorsum of the tongue were discretely reduced (Fig. 4). Currently, the patient remains under follow-up from the original medical team and the stomatology team of HPCA.

Figure 4: Clinical aspect after discontinuation of tacrolimus. a: Partial remission of polypoid manifestations on the dorsum of the tongue; b: remission of lip and perioral scaling, with reduction of angular cheilitis; c: remission of papillomatous hyperplasia of the palate; d: remission of gingival hyperplasia; e, f, g, h: remission of cobblestone appearance upper and lower lip mucosa and bilateral mucous membrane.
Discussion:
Approximately 80% of pediatric patients with solid organ transplant (heart, lung, liver and kidney) survive into teenage and adult life [1]. The adverse effects of immunosuppressants on the oral cavity are often observed due to the prolonged survival of these patients. The main changes observed include gingival hyperplasia induced by cyclosporine A and calcium channel blockers [4,5].
When tacrolimus was included in the immunosuppressant therapy after liver transplant, different lesions on the oral mucosa were recorded. Initially these lesions were clinically similar to the ones observed in CD [6,7] and OFG [8,9]. The adverse effects induced by tacrolimus on the oral cavity were observed in children, but not in adults submitted to liver transplant [10].
In the present study, the lesions observed on lips and mucous membrane were clinically equivalent to the cobblestone appearance mucosa diagnosed in CD patients, but the patient did not present frequent diarrhea episodes or recurrent aphthous stomatitis that could be seen as indications that he also presented the condition.
A retrospective study described the oral lesions detected in 251 children that underwent liver transplant [11]. The lesions observed by the authors had been described in previous studies [6,7], and were more frequent in patients who had undergone transplantation with 14 months of age, on average, and had received tacrolimus [11]. The OGLL present on the dorsum of the tongue were the most frequent and had emerged 28 months after transplantation, on average. Tongue fissures manifested, on average, 41 months after the surgery [11]. The other changes described by Saalman et al. [6] and Petti et al. [7] were also observed in the present case report. In this study the patient had used tacrolimus since the age of three years old, after the second liver transplant. The lesions on the tongue became perceptible when the patient was four years old. Therefore, within the same time span described by Saalman et al. [6], that is, between one and four years after transplantation.
A recent study described GPTD, which was considered a new nosologic entity [13]. The authors considered OGLL an unsuitable name for the lesions associated with the use of tacrolimus. The histological aspect of the lesions on the dorsum of the tongue in GPTD was described as overgrown fungiform papillae with subepithelial inflammatory infiltrate formed predominantly by lymphocytes and macrophages. No granulomatous manifestations were observed on the tongue or on the lips when cobblestone appearance mucosa was present. For this reason, the authors suggested that GPTD could not be included in the family of granulomatous diseases, since they did not exhibit granulomas. In the present case report, the results of the biopsy of lesions on the dorsum of the tongue and lower lip were similar to what was reported by Abreu Alves et al. [12,13].
Generalized Kaposi sarcoma was described in a child with liver transplant using tacrolimus [13]. The patient presented oral, skin, and digestive tract lesions that subsided when tacrolimus was discontinued and sirolimus was included in the therapy [13]. In the present case report, six years after the emergence of oral lesions, the patient had very pruritic, purple lesions across the skin of limbs and body that looked like Kaposi sarcoma. These skin lesions were not biopsied, and the patient did not complain of digestive problems or similar lesions on the oral cavity. These lesions only disappeared after tacrolimus was discontinued.
One of the theories proposed to explain the etiopathogeny of GPTD considers liver dysfunction prior to transplantation as a causal agent of poor tolerance progression, which is worsened due to post-transplantation immunosuppression and may lead to an inflammatory process that ends in GPTD.
Pediatric patients that underwent liver transplant and use tacrolimus require stomatological follow-up, since the oral lesions induced by this immunosuppressant agent emerge a few years into treatment.
For this reason, dentists should be part of a transdisciplinary team in organ transplantation. The role played by a dentist starts already before surgery in the effort to prevent any odontogenic infection soon after transplantation. After the procedure and during the prescription of immunosuppressant therapy, dental follow-up should be carried out aiming at preventing problems. Since the lesions induced by tacrolimus emerged late into the process, the dentist has to examine the oral cavity periodically in the search for GPDT characteristic lesions.
Conclusion:
Giant papillae tongue disorder (GPTD) is characterized by granulomatous formations on the dorsum of the tongue associated with alterations in the buccal mucosa. GPTD manifests in liver-transplanted children who receive a tacrolimus-based immunosuppressive protocol. Oral lesions arise after some years of chronic use of this medication. Diagnosis is established through the exclusion of other oral granulomatous lesions. GPTD regresses with the replacement of tacrolimus by another immunosuppressant. The dentist, as part of the multidisciplinary team that manages transplanted patients, will make the diagnosis of oral lesions and the oral infections prevention that may put the health of the pediatric transplant patient at risk.
Acknowledgements:
The authors thank the patient and his family for taking part in this case report.