Clinical Research and Clinical Case Reports
OPEN ACCESS | Volume 7 - Issue 1 - 2026
ISSN No: 2836-2667 | Journal DOI: 10.61148/2836-2667/CRCCR
Kevin Emeka Chukwubuike
Department of Surgery, Enugu State University Teaching Hospital, Enugu, Nigeria.
*Corresponding authors: Kevin Emeka Chukwubuike, Department of Surgery, Enugu State University Teaching Hospital, Enugu, Nigeria.
Received: October 11, 2021
Accepted: October 29, 2021
Published: November 02, 2021
Citation: Kevin Emeka Chukwubuike (2021) “Hollow Viscus Injury from Blunt Abdominal Trauma in Children: Experience in a Developing Country”. Clinical Research and Clinical Case Reports, 2(3); DOI: http;//doi.org/04.2021/1.1037
Copyright: © 2021 Kevin Emeka Chukwubuike. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Objective: To evaluate our experience in management of children who sustained hollow viscus injury following blunt abdominal trauma.
Methodology: This was a retrospective study of children aged 15 years and below who were managed for hollow viscus injury between January 2009 and December 2018 at the pediatric surgery unit of Enugu State University Teaching Hospital (ESUTH) in Enugu, Nigeria.
Results: A total of 583 cases of blunt abdominal traumas were recorded during the study period, out of which 21 (3.6%) cases had hollow viscus injury. The ages of the patients ranged from 8 to 14 years, with a median of 10 years. Road traffic accident and abdominal pain were the most common mechanism of injury and presenting symptom respectively. Six (28.6%) patients were in a clinical state of shock at presentation. Small intestinal was the most injured hollow viscus and the spleen was the most associated injured solid organ. Surgical site infection was the most common post-operative complication and 1 (4.8%) patient expired. Conclusion: Our experience revealed that although hollow viscus injury is uncommon in children, the small intestine is the most injured. Hollow viscus injury can be associated with significant morbidity and mortality.
1. Introduction
Trauma to the abdomen could be blunt or penetrating. Globally, trauma is a significant cause of morbidity and mortality [1]. Hollow viscus injuries mostly result from penetrating abdominal trauma. In blunt abdominal trauma, attention is usually more focused on the intra-abdominal solid organs and patient’s hemodynamic status. Blunt abdominal trauma causing perforation of a hollow viscus is relatively an uncommon occurrence in children and diagnosis may not be prompt [2, 3]. Late presentation and treatment may result in peritonitis, increased morbidity and mortality. Prompt recognition and treatment is the cornerstone of management of hollow viscus injury [4]. Blunt abdominal trauma resulting in hollow viscus injury has been quoted to have an incidence of 1% to 8.5% and may vary with geographical location [5]. One study conducted in Brazil reported an incidence of 4 to 15% [6]. Hollow viscus injury necessitates operative treatment while most blunt abdominal trauma with solid organ injuries are managed non-operatively [7]. Limited experience on the management of hollow viscus injury results from uncommon nature of the condition. There is paucity of data on hollow viscus injury resulting from blunt abdominal trauma in Nigeria. Hence, there is need for a study to determine the incidence, etiology, management and outcome of children who sustained hollow viscus injury. The aim of this study was to evaluate our experience in management of children who sustained hollow viscus injury from blunt abdominal trauma.
2. Methods
This was a retrospective study of children, less than 15 years of age, who were managed for hollow viscus injury between January 2009 and December 2018 at the pediatric surgery unit of Enugu State University Teaching Hospital (ESUTH) in Enugu, Nigeria. ESUTH is a teaching hospital in Enugu, Nigeria. The hospital serves the people of Enugu State, which, according to the 2016 estimates of the National Population Commission and the Nigerian National Bureau of Statistics, has a population of about four million and a population density of 616.0/km2. The hospital also receive referral from peripheral hospitals. Patients who have had surgery for a hollow viscus injury at a peripheral hospital before referral to ESUTH for reoperation were excluded from the study. The information extracted from the patients’ medical records included age of the patient, gender, interval between the incident and presentation, mechanism (etiology) of injury, clinical state at presentation, presence/absence of associated intra-abdominal injury, presence/absence of peritonitis, associated extra-abdominal injuries, intra-operative finding, operative procedure performed, complications of treatment, duration of hospital stay and outcome of treatment. The period of follow up was for 12 months.
Ethical approval was obtained from the research ethics committee of ESUTH. Patients’ caregivers gave their consent for the study. Statistical Package for Social Science (SPSS) for Windows version 23 (IBM Corp., Armonk, NY) was used for data entry and analysis. Data were expressed as percentages, median, mean, and range.
Pre-operative protocol
On presentation to the hospital, the patients were clinically evaluated and resuscitated using Advanced Trauma Life Support (ATLS) protocol. Abdominal ultrasound and radiographs were performed and further imaging investigation such as computed tomography (CT) scan was requested based on findings on clinical assessment. Urgent hemoglobin estimation and serum electrolytes were obtained. Anemia and electrolyte derangements (if any) were corrected and patient taken to theater for surgery. All the patients had laparotomy under general anesthesia.
Intra-operative protocol
Abdominal access was through transverse abdominal incision. An abdominal exploration was performed and any damaged hollow viscus was repaired as appropriate. The definitive surgery performed was dependent on the particular viscus that was damaged. The surgical procedures were carried out by a pediatric surgeon.
Post-operative protocol
Oral intake was started on return of bowel function. Post-operative complications were documented. Discharge was based on full establishment of oral intake and adequate wound healing.
3. Results
3.1. Demographic profile of the patients
A total of 583 cases of blunt abdominal traumas were recorded during the study period, out of which 21 cases had hollow viscus injury. This translates to 3.6 percent. Details of the patients demography is shown in Table 1.
|
Gender |
Percentage |
|
Male |
15 (71.4%) |
|
Female |
6 (28.6%) |
|
Median age of the patients |
10 years (8-14) |
|
Mean interval between incident and presentation |
5 days (3 – 10) |
|
Presented within 24 hours |
2 (9.5%) |
|
Presented between 24 and 48 hours |
3 (14.3%) |
|
Presented after 48 hours |
16 (76.2%) |
|
The mean duration of hospital stay |
16 days (11-25) |
Table 1: Patients’ demographic features (N=21)
3.2. Mechanism (etiology) of injury.
Road traffic accident was the most common mechanism of injury. Others are depicted in Table 2.
|
Mechanism of injury |
Number of patients |
Percentage |
|
Road traffic accident |
|
|
|
Pedestrian |
5 |
23.8 |
|
Passenger |
3 |
14.3 |
|
Fall from a height |
7 |
33.3 |
|
Assault |
3 |
14.3 |
|
Recreational accident |
2 |
9.5 |
|
Child abuse |
1 |
4.8 |
Table 2: Mechanism of injury (N=21)
3.3. Symptoms at presentation
The patients presented with abdominal pain, vomiting, constipation and abdominal distension in various combinations: Abdominal pain 21 (100%); vomiting 13 (61.9%); constipation 11 (52.4%) and abdominal distension 5 (23.8%).
3.4. Investigation performed
All the patients had abdominal/chest x ray and abdominal ultrasound. Eleven (52.4) patients showed free air under the diaphragm on radiograph. Abdominal ultrasound showed the presence of echo rich peritoneal fluid in 15 (71.4%) patients. Computed tomography (CT) scan was performed in 5 (23.8%) patients.
3.5. Hemodynamic status/peritonitis at presentation
Six (28.6%) patients were in a clinical state of shock at presentation. This was evidenced by tachycardia, hypotension and narrow pulse pressure. Five (23.8%) patients had peritonitis which was characterized by rebound tenderness, fever, guarding and rigidity.
3.6. Associated intra-abdominal/extra-abdominal injury
Three (14.3%) patients had associated splenic injury while two (9.5%) patients had associated liver injuries. One (4.8%) patient each had an associated head injury, right femoral fracture and left hemothorax.
3.7. Intra-operative finding and operative procedure performed
The small intestine was the most injured organ. Others are shown in Table 3.
|
Intra-operative finding |
Operative procedure performed
|
Number (%) |
|
Small intestinal perforation |
|
|
|
Ileum |
Primary repair |
10 (47.6) |
|
Jejunum |
Primary repair |
6 (28.6) |
|
Urinary bladder rupture |
Primary repair |
2 (9.5) |
|
Mesenteric injury with bowel gangrene |
Resection and anastomosis |
2 (9.5) |
|
Large bowel perforation |
Repair + ileostomy |
1 (4.8) |
Table 3: Intra-operative finding and procedure performed (N=21)
3.8. Complications of treatment
There was no complication in 11 (52.4%) patients. Surgical site infection was the most common post-operative complication as reflected in Figure 1.
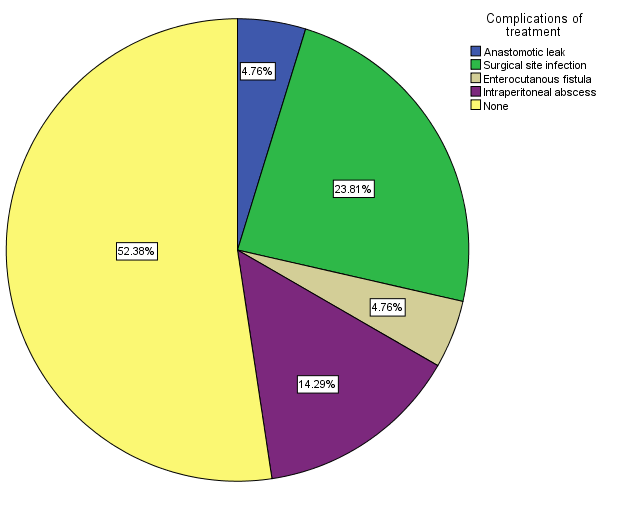
Figure 1: Post-operative complication (N=21)
3.9. Outcome of management
Nineteen (90.5%) patients recovered and were discharged home. One (4.8%) patient signed out against medical advice. One (4.8%) patient who had post-operative enterocutanous fistula expired.
4. Discussion
Early recognition of hollow viscus injury may not be easy and presents a task to the managing team [8]. The most frequent missed injury in blunt abdominal trauma is intestinal injury [9]. Forces such as compression or deceleration forces are responsible for hollow viscus injury. Compression force increases the intraluminal pressure resulting in rupture. Vascular injuries result from deceleration forces causing stretching/tearing of the mesentery [10]. Hollow viscus injury ranges from minor hematoma to frank perforation; it could also be partial thickness or full thickness injury.
In the present study, the incidence of hollow viscus perforation is consistent with the report of a similar study conducted in Turkey [11]. However, an incidence as low as 1% and as high as 15% has been reported [6, 12]. The difference in incidence may be due to the mechanism or severity of the trauma. The male predominance recorded in the current study is in line with the report of other studies [11, 13]. The exact reason for the male dominance is not clear but may be due to the fact that males behave more impulsively and take more risks than females. The median age of our patients is in agreement with the findings of other researchers [13, 14]. Howbeit, Borgialli et al reported a median age of 12 years [15]. The discrepancies in the median age of the patients in different studies may be explained by predominant etiology of the injury. For instance, in hollow viscus injuries resulting from abuse, the median age of the patients was 2.5 years [16]. The mean interval before presentation of our patients is not in agreement with the finding of Jha et al [17]. The late presentation of the patients may be due to ignorance and poverty which are quite common in low-income countries. There are wide variations in the duration of hospital stay of patients who sustain hollow viscus [13, 18, 19]. The duration of stay may be dependent on the extent of operative procedure and presence of associated injuries. Teuben et al reported longer stay in patients who have associated injuries [20].
Road traffic accident was the common mechanism of injury in the present study. This is comparable to the report of other series on hollow viscus injury [11, 19]. In developing countries, fall from height is a significant cause of hollow viscus injury [17, 21]. The explanation for the fall from height in children in low-income countries could be due to children climbing trees to pluck fruits. One uncommon cause of hollow viscus injury in children is abuse. Child abuse should be suspected in hollow viscus injury when the child or caregiver is in denial or when the degree of trauma is disproportionate to the extent of clinically observed injury [12]. The clinical presentation of children with hollow viscus injury may depend on the part of bowel that is injured and interval between the time of the incident and time of presentation to the hospital. Features of peritonitis may develop as early as 48 hours after a hollow viscus injury [13].
About half of our patients showed free air under the diaphragm. This is at variance with a report from South Asia [17]. The time interval between the incident and taking of the radiograph may explain the presence or absence of air under the diaphragm since it may take some time for air to accumulate in the peritoneal cavity. Abdominal ultrasound is essential for the detection of the site of hollow viscus perforation and echo rich peritoneal fluid. The ability of the sonographer to detect these features may depend on his experience and expertise. Computed tomography (CT) scan is considered the gold standard for evaluation of hollow viscus injury, however, non-availability, cost and exposure to significant radiations are the problems associated with CT scan [22].
About 29% of our patients presented in shock. One study conducted in Zaria, Nigeria reported that 23% of their patients presented in shock [23]. The late presentation of our patients may have accounted for the higher number of patients in shock at presentation. The associated injuries in our patients are similar to the findings of a study from Jharkhand, India [17]. Mortality is increased when hollow viscus injury is associated head injury [13].
The small bowel is the most injured hollow viscus in the index study. This finding is a consistent observation by other researcher [11, 17]. Gastric and urinary bladder injuries following blunt abdominal trauma have also been reported [24, 25]. The exact factors that determine which organs are injured in blunt abdominal trauma are unknown although the intensity of the trauma and area of impact may play a role. Surgical site infection following laparotomy for injured viscus is a common post-operative complication [26, 27]. This may be due to the bacterial loads in the intestine. Enterocutaneous fistula may follow anastomotic leak when anastomosis is performed in a background of gross peritoneal contamination [17].
The mortality rate of 4.8% recorded in the present study is comparable to the report of Jha et al. [17] However, Gunturi et al reported a mortality rate of 15% [28]. Mortality following surgery for hollow viscus injury could be multifactorial: disease related factors, patient related factors or surgeon related factors.
5. Conclusion
Hollow viscus injury following blunt abdominal trauma is uncommon in children and the small intestine was the most injured. In abdominal trauma following blunt abdominal trauma, a high index of suspicion for hollow viscus injury is required to avoid late diagnosis and its attendant morbidity/mortality. Emphasis should be placed on prevention which can be achieved by good parental control.
Limitation of the study
1. Children who succumbed to their hollow viscus injury before presentation to the hospital were not captured in this study.
2. Small sample size. A larger number of patients would have availed better analysis.
Declaration of conflict of interest: The author declares that there is no conflict of interest.
Sources of support: None