Clinical Research and Clinical Case Reports
OPEN ACCESS | Volume 7 - Issue 1 - 2026
ISSN No: 2836-2667 | Journal DOI: 10.61148/2836-2667/CRCCR
Adrian P. Hunis
Emeritus Member (ASCO), Emeritus Member (ESMO), School of Medicine, Universidad de Buenos Aires (UBA).
*Corresponding author: Adrian P. Hunis, Emeritus Member (ASCO), Emeritus Member (ESMO), School of Medicine, Universidad de Buenos Aires (UBA).
Received: September 06, 2021
Accepted: September 22, 2021
Published: September 24, 2021
Citation: Adrian P. Hunis. “Paraneoplastic Syndromes”. Clinical Research and Clinical Case Reports, 2(3); DOI: http;//doi.org/04.2021/1.1036
Copyright: © 2021 Adrian P. Hunis. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
,
Paraneoplastic Syndromes (PS) represent a constellation of signs and symptoms that result from effects distant from the tumor. These effects can occur in various organs and systems and are independent of the manifestations given by the tumor itself or by its metastases.
The classically best characterized SP were always those produced by those tumors secreting some polypeptide hormone; For example: ACTH or PTH, which are distributed through the circulation and act in the target organ, away from the cancer that produced them. They can also be due to the development of autoimmunity or to other mechanisms that were unknown until now. In the last 10 to 15 years, progress has been made in the knowledge of those SP that affect the Nervous System, both central and peripheral. These discoveries have revived interest in them. Although its frequency is low, it must be considered that it is difficult to determine with real accuracy the incidence of these disorders and this is due to several reasons; on the one hand the definitions and classifications are more than one and sometimes they do not coincide, in addition the etiologies are unclear and finally there are no controlled studies. Due to the reasons mentioned the frequencies vary from 1 to 7%
Despite its low frequency, its importance lies in the fact that its appearance can be the first sign of a malignant process since it frequently precedes the diagnosis of the tumor by months or years. This can generate an early detection, in a curable stage. Furthermore, it is important to note that its manifestations can be confused with those produced by the dissemination of the tumor (metastasis), perhaps leading to suspension of treatment and on the contrary; the presentation of treatable complications (for example: infections, drug toxicity), can be attributed to a PS, omitting its adequate treatment.
Due to the extensiveness of the subject, mention will be made of all known SPs, according to the organs and systems involved; and then the development will focus on Neurological Paraneoplastic Syndromes (PNS), which are the ones that have been best studied in the last decade.
PS, according to the organ or system involved:
1. Neurological.
2. Endocrine.
3. Hematological.
4. Renal.
5. Dermatological.
1) 1) Neurological: (They will be developed later along with the etiopathogenesis)
From the Central Nervous System:
A) Encephalomyelitis.
B) Limbic encephalitis.
C) Paraneoplastic retinopathy.
D) Cerebellar degeneration.
E) Opsoclonus-myoclonus.
From the peripheral nervous system:
A) Subacute motor neuropathy.
B) Sensory neuropathy.
C) Sensory-motor neuropathy.
From the neuromuscular junction
Eaton-Lambert myasthenic syndrome.
2) 2) Endocrine:
These syndromes are characterized by hormonal production independent of normal regulatory mechanisms (feed-back) and by the persistence of hormonal levels even after removal of the presumed producing gland.
A) A) Cushing's syndrome: secretion of adrenocorticotropin (ACTH), associated with lung cancer, especially small cell cancer.
B) B) Syndrome of inappropriate antidiuretic hormone secretion: Also associated with lung cancer and frequently with small cell cancer.
C) C) Non-metastatic hypercalcemia: parathyroid hormone (PTH) secretion, associated with lung cancer, especially squamous type
D) D) Gynecomastia: It can be associated with all types of lung cancer, especially small cell cancer.
E) E) Hyperthyroidism: Associated with lung cancer.
F) F) Calcitonin: Its secretion can be associated with the presence of medullary thyroid cancer, small cell lung cancer and breast cancer.
3) 3) Hematological:
In cancer patients, alterations have been reported in all hematopoietic cell lines, as well as in structural proteins. They are as follows:
A) Erythrocytosis: It is produced either by local or renal hypoxia, secretion of a factor that stimulates the release of erythropoietin, or by alteration of its metabolism, produced by the tumor itself. It is generally associated with kidney tumors, hepatomas, adrenal tumors, pheochromocytomas, and cerebellar hemangioblastomas.
B) Anemia: May be due to anemia of chronic processes, bone marrow invasion, blood loss, marrow suppression by chemotherapy, hypersplenism, autoimmune hemolytic anemia associated with solid tumors, megaloblastic anemia
and vitamin and iron deficiency.
C) Granulocytosis: Associated with gastric, pulmonary, pancreatic, melanoma, brain tumors, Hodgkin's disease, and Diffuse Histiocytic Lymphoma.
D) Granulocytopenia: Usually the result of chemotherapy and radiotherapy, and by action of other drugs or secondary to serious infection.
E) Eosinophilia and basophilia: In general, eosinophilia are seen in Hodgkin's disease and in Mycosis fungoides: It can also be seen in Melanomas, brain tumors and others. The existence of a factor that stimulates eosinophil production by tumor cells is possible. Basophilia is associated with Chronic Myeloid Leukemia, Myelofibrosis and Polycythemia Vera.
F) Thrombocytosis: occurs in 30 to 40% of cancer patients. It is seen in carcinomas, leukemias, and lymphomas. In these patients there is an increased risk of pulmonary embolism and deep vein thrombosis, compared to patients who do not present malignancies.
G) Thrombocytopenia: In general, it is related to chemotherapy, but there may be a similar ITP syndrome, which is rare and is seen in lymphomas, leukemias, sarcomas, lung cancer, breast, rectum, gallbladder, and testicle cancer.
H) DIC: It can appear as a chronic alteration of coagulation, as an acquired hemorrhagic diathesis or an alteration of coagulation only detected by laboratory studies.
Another cause of thrombotic or hemorrhagic complications, non-bacterial thrombotic endocarditis (NBTE), can appear with or without DIC, sometimes without clinical expression, only present in autopsy studies.
4) Renal:
Glomerular lesions and obstruction produced by tumor products can be considered true paraneoplastic syndromes.
In the case of nephrotic syndrome, which is rare, it can precede the diagnosis of the Neoplasia. An autoimmune mechanism is postulated. It is generally associated with lymphomas. Hodgkin's disease is the one most frequently associated with these disorders.
5) Dermatological:
They are a group of morphological variables that can be associated with both solid tumors and hematological neoplasms. Your diagnosis is important because it can suggest the underlying type of cancer. Its classification is difficult; In a recent review they are divided according to the basic skin lesion; and regarding their association with cancer, they are divided into those associated with solid tumors and those that present with hematological malignancies
I- Mucocutaneous syndromes associated with solid tumors:
A) A) Papulosquamous disorders:
-Acanthosis Nigricans: hyperpigmented warty hyperplasia.
It is seen in gastric and lung cancer. (fig. 1)
-Bazex syndrome (Acro keratosis): purplish erythema fingers, nose and pinna. It is seen in squamous cell lung cancer
-Paget's disease: exudative-erythematous dermatitis of the areola of the nipple. Present in breast cancer.
- Cutaneous florid papillomatosis: warty lesions on the back of the hand, present in gastric cancer.
-Sign of Leser-Trélat: predominant eruptive seborrheic keratosis on the trunk, associated with Lung Adenocarcinoma and Mycosis fungoides.
-Pityriasis rotunda: hyperpigmented plaques in the buttocks and abdomen, seen in hepatocarcinoma.
-Tylosis (Howell-Evans Syndrome): Palmoplantar keratosis. It is seen in cancer of the esophagus.

Fig. 1. Acanthosis Nigricans
B) B) Proliferative reactions:
-Hypertrichosis lanuginose: Reappearance of lanugo, hypertrichosis, seen in lung cancer.
-Hypertrophic pulmonary osteoarthropathy: drumstick fingers. (Lung cancer and mediastinal tumors) (Fig. 2).
-Multicentric reticulohistiocytosis: yellow papule-nodular lesions in the hands and periarticular, (associated with different
tumors).
-Palmar fasciitis-arthritis syndrome: nodular lesions of the palms, hands, and fingers. (Gynecological tumors).

Fig 2. Drumstick fingers.
C) Reactive erythema’s:
-Centrifugal annular erythema: erythematous polycyclic lesions, (associated with different tumors, infections and drugs).
-Erythema elevated: symmetrical erythematous plaques of the extremities. (Leukemias and monoclonal gamma diseases).
-Erythema gyratum repens: Erythematous concentric lesions
hives of the face, hands, and feet (lung cancer).
-Necrolytic erythema migrans: erythematous papules and plaques
that evolve to vesicles and scabs, migratrices. (Present
in Glucagonoma).
-Raynaud's phenomenon: Paleness, cyanosis, and hyperemia in
successive appearance, (associated with different cancers).
D) Vacuolar alterations of the basement membrane:
-Paraneoplastic dermatomyositis: Erythema (associated with different cancers)
E) Vasculitis:
-Trousseau syndrome: migraine thrombophlebitis (seen in cancers of the pancreas, lung and stomach).
II- Mucocutaneous syndromes associated with hematological neoplasms:
A) Dermo-epidermal alterations:
-Myxedematous lichen: papule-erythematous lesions (monoclonal gammopathies).
- Paraneoplastic amyloidosis (associated with different tumors).
-Scleromyxedema: Papules and plaques mainly on the face. (Monoclonal gamma diseases).
B) Neutrophilic dermatoses:
-Pyoderma gangrenosum: exudative purulent lesions with hemorrhagic content. (AML).
-Sweet syndrome (acute febrile neutrophilic dermatosis): nodules and asymmetric plaques on the extremities, head and neck. (AML). (Fig 3).

Fig. 3. Sweet syndrome.
C) papillomatous dermatoses:
-Ichthyosis: Keratinization predominantly in the hands and feet. (Seen in Hodgkin's disease).
-Paraneoplastic urticaria: persistent urticarial lesions. (Lymphomas and leukemias).
-Itch sine materia: generalizes in a few minutes, can be seen in Hodgkin's disease.
D) Reactive erythema’s:
-Erythroderma and exfoliative dermatitis: scaling and erosion with pustules, loss of hair and nails. (Mycosis fungoides).
-Erythromelalgia: Episodic pain and erythema in the extremities (rarely associated with tumors).
-Paneoplastic erythema nodosum: painful, scattered, erythematous violaceous nodules. (Leukemias and lymphomas).
E) Vasculitis:
-Leukocytoclastic vasculitis: Erythematous nodules and plaques, ulcers. (Leukemias, lymphomas, lung cancer).
-Nodorous periarteritis: subcutaneous nodules, erythematous papules, ulcers. (leukemias).
F) Vesicular-bullous disorders:
-Paraneoplastic bullous pemphigoid: bullous dermatosis, (different carcinomas).
-Paraneoplastic epidermolysis bullosa, associated with lung cancer.
-Paraneoplastic pemphigus: painful mucous erosions and skin eruptions (Hodgkin's disease).
-Pemphigus vulgaris: vesicular and bullous lesions (Kaposi's sarcoma, lymphoproliferative neoplasms) (Fig. 4).
-Pemphigoid of pregnancy: bullous lesions. (Choriocarcinoma)

Fig. 4. Pemphigus vulgaris.
G) Others:
-Bowen's disease: plaques of hyperkeratosis with a predominance of the trunk. (Squamous cell carcinoma of the skin, urogenital carcinomas).
-Diffuse melanosis: Pigmentation of exposed areas. (Visceral melanoma).
-Eruptive acrochordons: It is seen in breast cancer.
-Necrobiotic xanthogranuloma: Telangiectasias, deep nodules. (Monoclonal gamma diseases).
-Leukonychia: change in color of the fingernails. (Breast cancer).
-Generalized flat xanthoma: flat patches all over the body. (Myeloma).
-Subcutaneous fat necrosis: febrile nodular panniculitis. (Pancreatic cancer).
-POEMS syndrome: Hyperpigmentation and hypertrichosis. (Myeloma).
-Yellow nail syndrome: change in nail color. (Hodgkin's disease, Mycosis fungoides, monoclonal gamma diseases).
Hereditary diseases associated with cancer:
A series of diseases are described below, although it is still debated whether they should be included within the SP, they should also be considered due to their frequent association with cancer.
1) Gardner syndrome: epidermal cysts, sebaceous cysts, dermoid tumors, lipomas, and fibroids (adenocarcinoma of the small and large intestine).
2) Peutz-jeghers syndrome: Pigmentation of the lips, face, oral mucosa, and fingers (gastrointestinal adenocarcinoma).
3) Multiple mucosal neuromas: Neuromas of the eyelids, lips, tongue, and oral mucosa (Pheochromocytoma and medullary thyroid cancer).
4) Cowden's disease: Fibroids of the oral mucosa, warty papules acaras (thyroid cancer, breast cancer).
5) Multiple basal cell neuroma syndrome: Multiple and foveal basal cell carcinomas on palms and soles (medulloblastoma and fibrosarcoma of the jaw).
6) Phacomatosis:
Von Recklinghausen I-Neurofibromatosis: Neurofibromas and café au lait spots (Pheochromocytoma) (Fig. 1).
II-Tuberous Sclerosis (Bourneville's disease): Hypopigmented macules, adenomas, and fibromas (neoplasms of the nervous system).
III-Cerebellum-retinal Hemangioblastoma (Von-Hippel-Lindau): Retinal malformations and papilledema (neoplasms of the nervous system).
IV-encephalo-trigeminal syndrome (Stuger Weber): Capillary or cavernous hemangiomas following the cutaneous distribution of the trigeminal (neoplasms of the nervous system).
V-Ataxia-telangiectasias: Telangiectasias (lymphomas and leukemias).
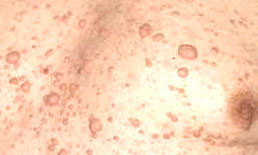
Fig. 1. Von Recklinghausen neurofibromatosis.
7) Bloom syndrome: Photosensitivity, telangiectasias and facial erythema (leukemias).
8) Fanconi anemia: hyperpigmentation in plaques (leukemias).
9) Chediak-Higashi syndrome: Recurrent pyoderma, giant melanosomes, and alteration of the color of the skin and hair (lymphomas).
10) Werner syndrome: sclerodermiform skin changes, early aging, leg ulcers (sarcomas, meningiomas and others).
11) Wiskott-Aldrich syndrome: Eczematoid dermatitis, pyoderma (lymphomas).
12) Sex-linked agammaglobulinemia (Bruton's syndrome): Recurrent infections. (Lymphomas and leukemias).
Miscellany
Anorexia-Cachexia: When they are diagnosed before cancer and disappear if the tumor improves or is resected.
Fever: When infections are ruled out, it can be associated with Hodgkin's disease or hypernephromas. It disappears if the tumor treatment is successful.
Lactic acidosis: Associated with Hodgkin's disease and acute leukemias.
Hyperlipidemias: They are seen in Multiple Myeloma, hepatomas, and colon cancer. It normalizes after tumor treatment.
Hypertension-hypotension: In lung cancer, hypernephroma and Wilms tumor. It subsides with the treatment of the tumor. It appears to be related to interference in the transmission of impulses to intrathoracic receptors, causing orthostatic hypotension and alterations in sodium excretion.
Amylase increased: Generally seen in lung adenocarcinoma (these tumors secrete salivary amylase).
Pneumatic hypertrophying osteoarthropathy: Finger and toe clubbing, periostitis of long bones. It appears more frequently in lung cancer (except in small cell cancer, in which this syndrome is almost non-existent). Interestingly, it often occurs in benign mesothelioma and rare neurinomas of the diaphragm, whereas malignant mesotheliomas never present with pneumatic hypertrophytic osteoarthropathy. It is also seen in metastases from different tumors (renal, thymoma, esophageal sarcoma, intrathoracic Hodgkin's disease, osteogenic sarcoma, fibrosarcoma). Estrogens, circulatory factors, neurogenic factors, and growth hormone have been postulated to play a role.
Amyloidosis: Around 15% of the cases of amyloidosis appear related to neoplasms such as Multiple Myeloma, lymphomas and carcinomas. Perhaps it is due to Ig fragments produced by blood dyscrasias and some tumors that provide the basis for the formation of the “amyloidogenic protein”. Treatment of the tumor does not make the already deposited amyloid substance disappear, but it does stop its progression.
Arthritis, polymyalgia rheumatica and SLE: There may be a high frequency of cancer in patients with asymmetric polyarthritis. Also 83% of patients with Polymyalgia rheumatica develop cancer a few months after their diagnosis. SLE is associated with lymphomas, acute myeloid leukemia, thymomas, ovarian and testicular tumors, and lung cancer. Treatment of the tumor conditions the remission of the SLE.
Etiopathogenesis:
Most researchers believe that PNS are of autoimmune etiology. Their hypothesis is that proteins normally expressed only by the nervous system are ectopically expressed by the tumor. For unknown reasons, the immune system recognizes the ectopic antigen as foreign and generates an attack that damages both tumor cells and those of the nervous system. The autoimmune hypothesis model is best understood in Eaton-Lambert Syndrome where antibodies that react against proteins ectopically expressed by the tumor bind to calcium channels, preventing their entry and thus decreasing the release of acetylcholine. In the other SP, the action of antigens and antibodies is less understood. The knowledge acquired in the last 15 years led to the discovery of several cancer-related antibodies that affect certain areas of the nervous system. This rekindled the interest of neurologists and oncologists; These cases represent a diagnostic challenge because, in general, the cancer is not evident when symptoms begin, and there may also be confusion with other inflammatory processes of the nervous system. The finding of some of the antibodies known to date unequivocally establishes that the disorder is of paraneoplastic origin.
The underlying cancer may be small or undetectable, even by the most sophisticated techniques. Fortunately, many antibodies also target the cancer most likely associated with them. For example: Anti-Hu indicates the presence of small cell lung cancer. The anti-Yo antibody is associated with ovarian and breast cancer; For some authors the relationship is so strong that they recommend hysterectomy and adnexectomy in postmenopausal patients with positive anti-ego, even with pelvic imaging studies without evidence of tumor and with normal mammograms
The existing evidence suggests that in patients with positive antibodies, neoplasms grow more indolently, and metastases are less frequent. This has been demonstrated in animals. Furthermore, it is pointed out that treating the symptoms of PNS could accelerate tumor growth.
Although the antibodies and the observed reactions have been detected, it remains to be understood their true role in these disorders. The evidence for an autoimmune etiology is strong for Eaton-Lambert myasthenic syndrome. For the other SPNs, the autoimmune theory is supported by the presence of specific antineuronal antibodies. These antibodies serve as a diagnostic weapon, but their role in neuronal injury and clinical disease is still unclear.
Hu antigens:
The term "Hu antigens" relates to a family of nuclear proteins that are normally expressed in all neurons of the central and peripheral nervous system, but not in other cell types (except for the testes). As early as 1948, Denny Brown described a sensory neuropathy associated with lung cancer, but at that time it was not related to any autoimmune mechanism. Many years later, in 1965; Wilkinson and Zeromski raised this possibility by finding that serum from patients with small cell lung cancer and paraneoplastic sensory neuropathy reacted with neurons in the cerebral cortex of guinea pigs. It was not until 1985 that Graus et al. find and define for the first-time high titers of antibodies called "Hu" in the serum of patients with small cell lung cancer. These antibodies fixed complement and reacted predominantly against the nucleus of neurons present in the central and peripheral nervous system.
Hu antigens correspond to a group of proteins of 35 to 40 kd which, by Western Blot analysis, are found both in neurons and in tumor tissue. Over time, evidence of anti-Hu antibodies associated with encephalomyelitis also began to appear. Several proteins have been identified that have been integrated into this "Hu family" of antigens. Studies carried out in animals try to see the role of these proteins, it is suspected that they could have importance in neuronal development. These proteins are expressed in various tumors, not only in small cell lung cancer, but also in neuroblastomas, various types of sarcomas, and prostate cancer. But it is not yet clear how the presence of antibodies against Hu proteins is related to the destruction of areas of the nervous system; and how important they may be to the growth of the underlying tumor. The true role of the Hu proteins present in the mentioned tumors is not known either.
Proteins I
The term "I proteins" refers to a family of proteins with high expression in the cytoplasm of Purkinje cells of the cerebellum and in tumor cells (generally ovarian and breast tumors), which is seen in patients with cerebellar degeneration. In animals, low serum titers of anti-Yo antibodies react against Purkinje cells of the cerebellum and also with other cells of the central nervous system. In humans the reaction is restricted to the cerebellum. There are 3 types of I proteins: CDR 34, CDR 62-1, and CDR 62-2. These proteins have been cloned and it was found that some of them could recognize anti-Yo antibodies. In any case, it is not clear what is the relationship of these proteins and antibodies with cerebellar degeneration. But it is important to note that high titers of antibodies that react predominantly against Purkinje cells; with relative indemnity from the rest of the nervous system, they strongly suggest the role of those. T cells have also been found in the blood of patients with cerebellar degeneration, these cells recognize Yo antigens and appear to be cytotoxic to tumor cells. On the other hand, so far it has not been proven that these cytotoxic mechanisms cause loss of Purkinje cells.
Other paraneoplastic antigens and antibodies
Several onconeural antigens have been identified by examination of serum from patients with SPN. Anti-amphiphysin antibodies are present in patients with Stiff-Man or Stiff Man Syndrome and breast cancer, less frequently in patients with encephalomyelitis and lung cancer. A new family of paraneoplastic antigens has recently been identified (the Ma proteins). The best characterized are Ma 1 and Ma 2. The expression of these proteins is restricted to neurons and spermatogenic cells of the testes. Antibodies that react against these proteins are found in cerebrospinal fluid of patients with cerebral and cerebellar dysfunction, associated with various types of tumors (lung, breast, parotid gland, colon). Anti-Ta antibody is present in the serum and cerebrospinal fluid of patients with limbic encephalitis associated with testicular cancer.
Ma proteins are expressed by tumors from patients with PNS, but not by similar tumors from patients without such syndromes. Patients with Eaton-Lambert Syndrome develop antibodies that react with active areas of the synapse and presynapse, blocking the entry of calcium necessary for the release of acetylcholine. Studies on this syndrome suggest that antibodies develop against multiple epitopes, mostly contained in voltage-gated calcium channels (CCVD) and in the P / Q-type subunit. It is not known if the antibodies are pathogenic or if they are the expression of an immune response.
In any case, the abundance of these antibodies in the calcium channels of cerebellar cells and in the serum of patients who develop Eaton-Lambert Syndrome is suggestive.
Paraneoplastic syndromes affecting the central nervous system:
1) Encephalomyelitis:
The term encephalomyelitis describes an inflammatory condition that affects various levels of the nervous system and that occurs in patients with small or hidden cancers, in general: small cell lung cancer. Clinical findings may be restricted to a single area or cell group of the nervous system (e.g., dorsal root or Purkinje cells) or several cell types and various levels of the nervous system may be involved, e.g.: brain, spinal cord, ganglia. of the dorsal root, autonomic nervous system, peripheral nerves and muscles. Most of these patients have a so-called antiHu antibody that reacts with the nuclei of all neurons in both the central and peripheral nervous systems. It is unknown why some areas of the nervous system are affected, and others are not, in the case of the same individual. The evolution has a subacute course and usually, although not always, leads to disability. Early in the disease there is pleocytosis in the cerebrospinal fluid. The proteins in this liquid and the concentration of Ig G are increased throughout evolution. Antibodies, when found, have higher titers in cerebrospinal fluid than in serum, suggesting that they are synthesized intrathecally. There is no known treatment.
2) Limbic encephalitis:
Paraneoplastic limbic encephalitis is a rare complication of small cell lung cancer and other less common cancers. It presents with changes in personality and mood over a period of days or weeks, associated with severe recent memory impairment and sometimes agitation, confusion, and hallucinations. It can occur isolated or associated with more diffuse encephalomyelitis or sensory neuropathy. Changes are restricted to the insular or limbic cortex, but deeper structures may sometimes be involved. Sometimes areas surrounding the white matter can be affected. There is reactive gliosis and extensive loss of neurons, accumulations of perivascular lymphocytes, and microglial proliferation. It has been seen to resolve after treatment of the underlying tumor, especially in Hodgkin's disease. It can be part of a more extensive encephalomyelitis, particularly in patients with anti-Hu antibody, but it can also exist in the absence of it.
3) Cancer-associated retinopathy:
Cancer-associated retinopathy is rare, seen in cases of small cell lung cancer, melanomas, and gynecological tumors. Symptoms precede the diagnosis of the neoplasm and progress, leading to vision loss, which is usually bilateral. There are episodes of darkening of vision and night blindness. Visual tests show scotomas and loss of visual acuity. The fundus may reveal arterial narrowing and abnormal mottling of the retina. The electroretinogram is always abnormal and establishes the diagnosis. Inflammatory cells can be identified in the vitreous by slit lamp examination. Pathologically there is loss of photoreceptors and ganglion cells with infiltration of lymphocytes and macrophages. The rest of the optic pathway is generally preserved. Serum antibodies that react with antigens of the photoreceptors and basal or ganglion cells have been found, although not in all cases; the best characterized (anti-retinal antibody) recognizes a photoreceptor protein. Treatment with prednisone, plasmapheresis, and immunoglobulin can stabilize symptoms.
4) Paraneoplastic cerebellar degeneration:
It has an abrupt beginning. It evolves rapidly and causes severe trunk and limb ataxia, dysarthria, and dysphasia. It can be very severe and lead to the total disability of the patient. It can be associated with other neurological signs or be purely cerebellar. Associated cancers are breast, ovarian, lung, and Hodgkin's disease. In general, the evolution is independent of the treatment of the underlying tumor. Occasionally, patients with Hodgkin's disease develop spontaneous remissions. In others, responses to treatment or spontaneous remissions are rare. Its frequency is low, less than 1% of cancer patients. However, when cerebellar degeneration develops in a patient, the risk of it being an PNS is close to 50%. Several antibodies are associated with cerebellar degeneration. The anti-Yo antibody occurs in degenerative Purkinje cell disease associated with breast and ovarian cancer. The anti-Tr antibody occurs in the same entity but in association with Hodgkin's disease. Anti-Hu is detected in patients with cerebellar degeneration associated with small cell lung cancer, but in these patients, it occurs together with more extensive encephalomyelitis.
Only 50% of patients have positive anti-Hu antibody. Sometimes some of the patients who are anti-Hu negative and signs of cerebellar degeneration plus lung cancer also present with Eaton-Lambert Myasthenic Syndrome.
Symptoms usually precede the appearance of the tumor. When a patient presents with disseminated cancer and develops cerebellar signs and symptoms, other entities that can be confused such as Wernicke's encephalopathy, drug neurotoxicity or metastatic disease must be ruled out.
5) Opsoclonus-Myoclonus:
Opsoclonus is a term used to describe involuntary, arrhythmic, conjugated, high amplitude eye movements that occur in the horizontal, vertical, and oblique planes. It is often associated with myoclonus and trunk instability, with or without cerebellar signs. Paraneoplastic opsoclonus-myoclonus is of acute onset and occurs in children with neuroblastoma; in adults it is associated with various cancers (breast, bladder, lung). Anti-Ri antibodies were found in some patients with opsoclonus-myoclonus.
In children, it appears to respond both to immunosuppression with corticosteroids and to treatment of the underlying tumor, although most patients do not fully recover. In adults there are sometimes spontaneous remissions.
In some patient’s abnormalities may be found in the cerebellum. In others, no positive result is obtained despite careful pathological study of the brain and cerebellum.
Paraneoplastic syndromes affecting the peripheral nervous system:
Paraneoplastic peripheral neuropathy:
Cancer patients can have peripheral neuropathy from several causes other than the tumor, including:
Neoplastic invasion: Metastatic leptomeninges’s. Neurolymphomatosis.
Chemotherapeutic agents: Vinca alkaloids. Platinum compounds. Taxanes.
Nutritional neuropathies: Cachexia. Vitamin deficiency (B1, B12).
Metabolic disorders: Uremia (pelvic tumors). Hypothyroidism (post-radiotherapy). Multi-organ failure (critical illness polyneuropathy).
Not related to cancer: Diabetes Mellitus.
All these causes must be considered and ruled out for the diagnosis of paraneoplastic neuropathy. But if a subacute sensory neuropathy is present and the presence of the anti-Hu antibody is confirmed, it can be affirmed without a doubt that the origin is paraneoplastic, and the most likely associated cancer is that of the small cell lung.
There are 4 types of paraneoplastic neuropathy: motor, sensory-motor, sensory, and autonomic.
I-Motor or sensory-motor: They can be acute or chronic, progressive, or not, demyelinating, axonal or neuronal (cells of the medullary anterior horn). Clinically they are indistinguishable from no paraneoplastic neuropathies unless they resolve after tumor treatment and / or are associated with the presence of anti-Hu. This group includes:
A) Guillain-Barré syndrome: It occurs more frequently in patients with Hodgkin's disease than in the general population. This marks its paraneoplastic origin-
B) Subacute motor neuropathy: Pathologically characterized by the disappearance of anterior horn cells (with or without signs of a lower motor neuron), which affects patients with Hodgkin's disease or other lymphomas. In some patients, the findings cannot be distinguished from those of Amyotrophic Lateral Sclerosis, but if spontaneous remission of symptoms occurs, this pathology is ruled out.
II-Sensitive:
It is estimated that in approximately 20% of patients with this disorder there may be an underlying cancer. Another disease that can be associated with this entity is Sjogren’s Syndrome. This neuropathy is of rapid and severe evolution, in which the patient loses all the sensitivity of the 4 extremities. Although it can begin on the face and trunk, it is common for it to begin distally in the extremities and extend proximally. The loss of sensation is so important that it makes normal activity difficult, such as walking or simply coordinating movements with the hands. Symptoms generally precede detection of the tumor. Small cell lung cancer is the one most frequently associated with this disorder; in addition, high titers of anti-Hu antibody are detected.
In electrodiagnosis there is an absence of sensory potentials. Motor nerve conduction may be intact. Neuropathological findings include loss of dorsal root neurons and inflammatory infiltrates, primarily composed of T cells and anti-Hu antibodies on the surface of the remaining sensory neurons.
III-Autonomous:
This neuropathy is frequently associated with encephalomyelitis, with the presence of anti-hu antibody. However, some patients develop isolated dysautonomia. Small cell lung cancer is seen together with this neuropathy. There may also be enteric autonomic dysfunction, which manifests as intestinal pseudo-obstruction; patients present with weight loss, stubborn constipation, and abdominal distention. There may also be esophageal dysmotility and gastroparesis, as well as other symptoms of autonomic dysfunction such as arterial hypotension, urinary retention, impotence, xerostomia, and pupillary abnormalities.
Pathologic studies show loss of myenteric plexus neurons along with inflammatory infiltrates.
Whenever a sensory or sensory-motor neuropathy is found that develops rapidly and severely, the possibility of an underlying tumor should be suspected, although it is often not detected.
IV-Neuromyotonic, myotonia and Stiff-Man Syndrome:
A. Neuromyotonic, myotonia: Characterized by rigidity, myokymia’s, numbness, profuse sweating, and difficulty in muscle relaxation. It is sometimes associated with sensory-motor neuropathies.
The electrophysiological study shows high frequencies and discharges of motor units. Muscle activity persists during sleep, general anesthesia, and neuromuscular junction blockage. It is associated with lung cancer and thymomas. Studies suggest that there may be potassium channel disturbance. It can be part of anti-Hu encephalomyelitis.
B. Stiff-man syndrome or Stiff-Man: It is characterized by rigidity of the skeletal muscles with superimposed painful spasms. All 4 members are affected. The spasms can be severe, sometimes causing deformities, and are accompanied by bone fractures. It is associated with small cell lung cancer, breast cancer, thymomas, and Hodgkin's disease. Some breast cancer patients have amphiphilic antibody and 128 kd neuronal synapse proteins. Sometimes treatment of the tumor and immunosuppression with corticosteroids can be beneficial.
Paraneoplastic syndromes affecting the neuromuscular junction:
Eaton-Lambert Myasthenic Syndrome:
1 to 3% of patients with small cell lung cancer have Eaton-Lambert Syndrome. Other tumors (thymomas and lymphomas for example) are only occasionally associated with this disorder. In more than 2/3 of the patients, the origin is paraneoplastic, in the remaining 1/3 the causal mechanism is unknown. It is characterized by presenting generalized weakness, mainly in the advanced stages of the disease, although it can sometimes be the first symptom. Classically, the weakness affects the proximal muscles more than the distal muscles, it is of such intensity that patients have difficulty climbing stairs, getting up from a low chair or lifting heavy objects. Most of the patients present autonomic dysfunction, manifested by xerostomia, impotence, constipation and blurred vision. Sensitivity is preserved, but there are paresthesia’s in the thighs. Fatigue is the characteristic symptom. On examination, patients appear less faint than their symptoms suggest. There is a decrease in tendon reflexes in the lower limbs. The characteristic sign is the increase in strength and reflexes that occurs after attempting a maximum contraction of the involved muscle. Alterations of the cranial nerves are common (palpebral ptosis, diplopia, or dysphagia), but the involvement is mild and generally transitory and should not be confused with that observed in Myasthenia Gravis, where it is more severe.
Electrophysiological abnormalities are pathognomonic, they include a decrease in the muscle component of the action potential; responding with a decrease in the response to repetitive stimuli of 3 Hz, but with an increase in said response with repetitive stimuli of 50 Hz. If this increase is greater than 100%, the test is confirmatory. The same increased response can be achieved with maximum voluntary muscle contractions lasting 10 to 30 seconds (Fig. 6). Eaton-Lambert Syndrome has generated much controversy regarding its treatment. Some authors point out that patients can improve with ex-blood transfusion and only Eaton-Lambert of non-paraneoplastic origin would have any response with immunosuppressive treatment with corticosteroids or azathioprine. It is also postulated that the treatment of the underlying tumor may be accompanied by a decrease in symptoms.
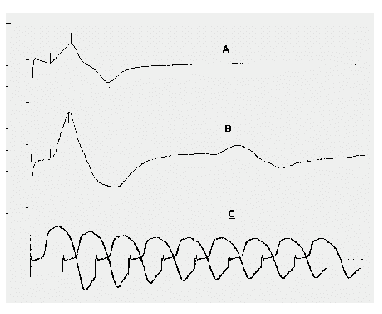
Fig. 1-Electrophysiological results of repetitive stimulation in patients with Eaton-Lambert Syndrome: A) Reduction of the motor evoked potential (PME) obtained after simple stimulation; B) Increase in the amplitude and area of the PME obtained after maximum contraction for 10-30 "in results greater than 100%; C) Stimulation at low frequencies will show a progressive decremental pattern with facilitation or increase at high frequencies.
Pathological anatomy:
The pathological anatomy is variable according to the syndrome in question. In some patients no lesions can be found, despite careful examination. This happens in patients with opsoclonus-myoclonus and Eaton-Lambert syndrome. In cerebellar degeneration, a total loss of Purkinje cells can be seen, with compensation for the rest of the nervous system. In the other disorders the characteristic finding, when present, is the disappearance of neurons together with inflammatory infiltrates present.
Antibody detection:
Although there are no large clinicopathological studies available to establish the sensitivity and specificity of the tests to establish the presence of an SPN associated with antineuronal antibodies, the presence of these antibodies is of high diagnostic value. In some patients, the tumor is not detected despite a careful search, even with high antibody titers and compatible symptoms. In these it is possible to think that the tumor is very small or not detectable; some authors also postulate that it could be a spontaneous remission. In any case, the presence of malignancy is not excluded.
In 1994, guidelines were established for the detection of antibodies that could be identified with certainty, (anti-Yo or APCA-1; anti-Hu or ANNA-1 and anti-Ri or APCA-2), these are the ones that until the At the moment they make a diagnosis of SPN without a doubt, despite the absence of tumor. There are also others that have appeared that are still in the study stage, their determination is not well publicized (anti-Tr; anti-Ta; anti-Ma).
On the other hand, there are cases in which the signs and symptoms of an SPN are observed together with the presence of a cancer, with negativity of the studies to detect antibodies; it may not be possible to rule out that they are undoable antibodies by the currently available methods.
Differential diagnosis:
The presence of other different mechanisms that can also affect the nervous system must be considered:
1) Metabolic, nutritional, or hormonal: Produced by organ failure, tumor marker hormones (ACTH, PTH), or by substrate competition at the level of the cells of the nervous system. This can lead to the presentation of Cushing's Syndrome, hypercalcemia, hypoglycemia, or vitamin deficiency syndromes.
2) Opportunistic infections: Side effects of treatment such as radiation myelopathy or neuropathy secondary to chemotherapy (vinca alkaloids, cisplatin, taxanes).
3) Vascular: embolic infarction (septic, tumor), thrombotic (due to vascular disease or DIC), subarachnoid hemorrhage, subdural hematoma, intraparenchymal hemorrhage (due to spontaneous bleeding or DIC).
4) Metastasis of the nervous system.

Fig. 6- Tomographic image of 2 brain metastases.
Conclusions:
PS are a set of signs and symptoms secondary to effects distant from the tumor, independent of the manifestations of them and their metastases. These effects are associated with several mechanisms: secretion of certain hormones, development of autoimmunity and still others that remain unknown until now. In the last 15 years, progress has been made in the knowledge of PNS, discovering various antigens and antibodies that could be related to the development of the signs and symptoms seen in these disorders. The result of the investigations strongly supports an autoimmune etiology, an antigen-antibody reaction is postulated that would affect both tumor cells and those of the central and peripheral nervous system. In any case, the mechanism by which they would act is not yet well defined.
The true frequency of these disorders is difficult to determine but it is always low (1 to 7%). The important thing to note is that despite its low frequency, its appearance usually precedes the detection of the tumor, thus being able to lead to a diagnosis at an early stage and to a treatment with a greater chance of success. The manifestations can occur at any level of the nervous system. In some cases of rapidly evolving and / or severe cerebellar degeneration or sensory neuropathy, perhaps the possibility of an underlying cancer should be considered.
The advances made suggest that there are possibilities to investigate new antibodies. The implications that future detections may have cannot be ruled out. Although its true role remains to be known, it is known that they affect tumor growth. This opens a panorama that could contribute to the management and treatment of neoplasms.