Clinical Research and Clinical Case Reports
OPEN ACCESS | Volume 6 - Issue 2 - 2025
ISSN No: 2836-2667 | Journal DOI: 10.61148/2836-2667/CRCCR
Pedram Habibi1, Hojjat Molaei MD2*
1School of Medicine,Tehran University of Medical Sciences, Tehran, Iran.
2plastic & reconstructive surgery department, School of Medicine,Tehran University of Medical Sciences, Tehran, Iran.
*Corresponding author: Hojjat Molaei MD, Vali-e-asr Hospital, IKHC, Bagherkhan St., Towhid Sq., Tehran, Iran.
Received: September 01, 2021
Accepted: September 22, 2021
Published: September 24, 2021
Citation: Pedram Habibi, Hojjat Molaei MD. “What Prevents Recurrence of Marjolin’s Ulcer and What the Best Treatment Is: A Systematic Review”. Clinical Research and Clinical Case Reports, 2(2); DOI: http;//doi.org/04.2021/1.1034
Copyright: © 2021 Hojjat Molaei MD. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
Marjolin’s Ulcer (MU) is defined as an ulcer that progresses through malignancy over a period of time. Pathophysiology of this disease is not 100% clear, although some findings suggest mutation of genes, responsible for cell division and apoptosis, is observed in MU patients. It takes 32 years on average for MU to develop after the first contact with the damaging agents. The best recommended treatment for MU is resection surgery for the affected area and amputation if the malignancy reaches the bone and deep tissue. Adjuvant therapy such as radiotherapy and chemotherapy are not supported by the literature to be in the treatment, however, some physicians decide to implement these non surgical interventions.
Methodology
Utilizing the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA), we managed to find 52 records and after exclusion, being left with 9 articles related to our questions in mind, which were “What is the best available intervention for MU?” and “what are the predicting factors for MU?”.
Results
After carefully scanning 9 articles for possible answers to our question, we found 414 patients from different demographics. There was enough information in each article that together, a complete puzzle started revealing itself, suggesting that lymph node involvement is an important factor in recurrence and, possibly, survival of the patient. Also it has been revealed that adjuvant therapy is still not proven effective in treating MU.
Conclusion
Based on our findings, we suggest health care providers first assess the degree of involvement. If it is only local, local resection might suffice. If there are any bone involvements, amputation is indicated. All the palpable lymph nodes must be removed to prevent further recurrence of MU. Radiotherapy and Chemotherapy are not indicated in MU patients.
Introduction
Although the definition (and even the name) of the disease has been changed (or has been in controversy ,for the lack of a better phrase) we could safely suggest that Marjolin(‘s) Ulcer (MU) is a type of skin injury (mostly after an incidence of burn) that progresses towards some type of malignancy (Squamous Cell Carcinoma, in most cases). (1) This type of malignancy-related ulcer is highly aggressive with high rates of recurrence. Nearly 1.7% of all chronic scar cases lead to malignancy and are considered to be MU by the definition given above (2). It has been suggested that the initial wound formation (eg. burning of the skin) could be as long as 32 years earlier than the first diagnosis of MU. This period between exposure and diagnosis is called latency. Considering the long latency and the intrinsic characteristics of MU, it has been shown that the longer the period, the worse the prognosis of the affected patient.
Different pathophysiological pathways might be responsible for the occurrence of MU, one of which has been reported to be the mutation of genes responsible for cell division and apoptosis in the affected patients. Also it has been suggested that prolonged presence of scar tissue might be responsible for loss of immune cells in the affected tissue, leading to escape of malignant cells from immunological response, resulting in possible metastasis. Also (3, 4)
As mentioned before, it takes ,on average, 32 years to diagnose MU after the first contact with the damaging agent (burning agents, such as heat or acid for the most common ones). This is the case present for chronic MU. It has also been suggested that there is acute MU, which takes 12 months or less to form after the initial damage. It has been previously pointed out that squamous cell carcinoma is the most common form of malignancy in MU patients. However, in the setting of acute disease, basal cell carcinoma is mostly seen in MU patients. In an overlook, it has been shown that 71% of cases of MU are squamous cell carcinoma, 12% basal cell carcinoma, 6% melanoma, 5% sarcoma, and the remaining 4% are other types of neoplasms. (5)
Although we are dealing with a malignancy, due to the fact that we are also dealing with an ulcer, necessary surgical interventions must be taken into account. To further explain different modalities of surgery, we must initially understand how the ulcer acts in different people. Starting from the top, some people might encounter isolated skin involvement, while others might have lymph node metastasis, and last ,but certainly not least, malignancy might reach deep tissues and bones. For each pathogenesis there is the respective surgical modality. If there is no metastasis and the malignancy limits to the surface tissue, ie. dermis, epidermis, and subdermis, excision and resection of the local area might suffice, while if there is lymph node involvement, the surgeon must remove the affected node, as they should in any malignancy-related surgery. If there is deep tissue and bone involvement, amputation of the limb is the preferred method to effectively prevent the spread of the malignant cells. To state the obvious, if the patient is not cleared for surgery (ie. advanced age, underlying condition, …) non-surgical interventions are the only options, which translate to radiotherapy and chemotherapy. (6)
The role of radiotherapy remains unclear. Some studies have implemented this approach for patients, tumors of whom are inoperable, the patient is not cleared for surgery for whatever the underlying condition might be, or as an adjutant therapy after the surgery has been performed.(7) No clear causal benefit from radiotherapy has been drawn in the papers published to this day. This might be due to poor vascularization of the tissue, hence the possible decreased benefit of this treatment. The role of chemotherapy and immunotherapy is even more vague than radiotherapy. In one study it had been shown that Cemiplimab has 47% success in treating squamous cell carcinoma, but still no causal relationship between this treatment and MU could be drawn since no Randomized Clinical Trials (RCTs) have been done regarding the subject. (8, 9)
Considering the factors mentioned above, regarding treatment of MU patients, we have decided to do a systematic review of the literature, aiming in mind to find the best available treatments with the help of our colleagues in different centers around the globe, using their experience in this field with the number of the patients they have had and the modalities of treatments they have utilized in the course of their patient’s disease.
Methodology
Bearing in mind that we are looking for the best treatment, or maybe a combination of such, we decided to look for centers with enough experience treating these patients (ie. more than 1 patient in their experience) suggesting the answers, published in the 21st century. The first phrase for the search was “Marjolin Ulcer” but after a quick review, we realized that some papers have used the term “Marjolin’s Ulcer” in their terminology, so we separated two phrases with the command “or” to be searched for in the title and/or the abstract of articles in PubMed, done in July 13th, 2021. One of the things that was considered to be our criteria for treatment was surgical intervention. So we included the word “surgery” in our search terminology to be included in the title and/or the abstract, separated from the first phrase by the command “and” to make sure both of these are included in the title and/or the article. A total of 52 articles were found.
Using the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) (10), first we observed for any duplicates in those 52 articles, and because only PubMed database was used in the search (with no additional records through other sources), no duplicated were found. Then the 52 remaining records were screened for relevance to the initial question of the present study. 10 records were published before the year 2000. 22 records were case reports, which, as mentioned before, is not sufficient to be called an ‘experience in treating MU patients with different presentations and different modalities of treatment”. 8 records were non-English. 1 study was not concerned with the surgical outcome and another confused SCC with MU, which as we know today, do not overlap thoroughly. 11 records remained for further investigation and full-text screening for relevance. After screening full texts, one article was concerned with all malignancies of the skin, and another one was related to leg defects, not just MU. In the End, 9 records remained for the final qualitative analysis. Some factors, as mentioned further in this article, were not completely covered by all the articles but all 9 publications had some factors that would complement each other that would make them enter the final meta-analysis.(7, 11-18) (fig 1)
Variables that the present study have searched for in the final records contain: number of marjolin patients in each record, of those, patients who had gone under surgery, mean age in which marjolin had occured in the patients (considering minimum and maximum age), sex of the patients with male to female ratio, type of surgery (local excision vs amputation) suggestive of severity of the ulcer, patients with second surgery performed on them, adjuvant treatments such as radiotherapy and chemotherapy, lymphnode involvement, number and percentage of reccurence of the ulcer, and the number of deaths observed in the patients.
Different factors required different modes of statistical analysis. Having this in mind, we used IBM SPSS Statistics 26 to analyze our data, looking for significance of our findings. Significance has been reported by P, representative of P-value, followed by Odds Radio (OR) with 95% confidence interval, minimum and maximum amount in parentheses.
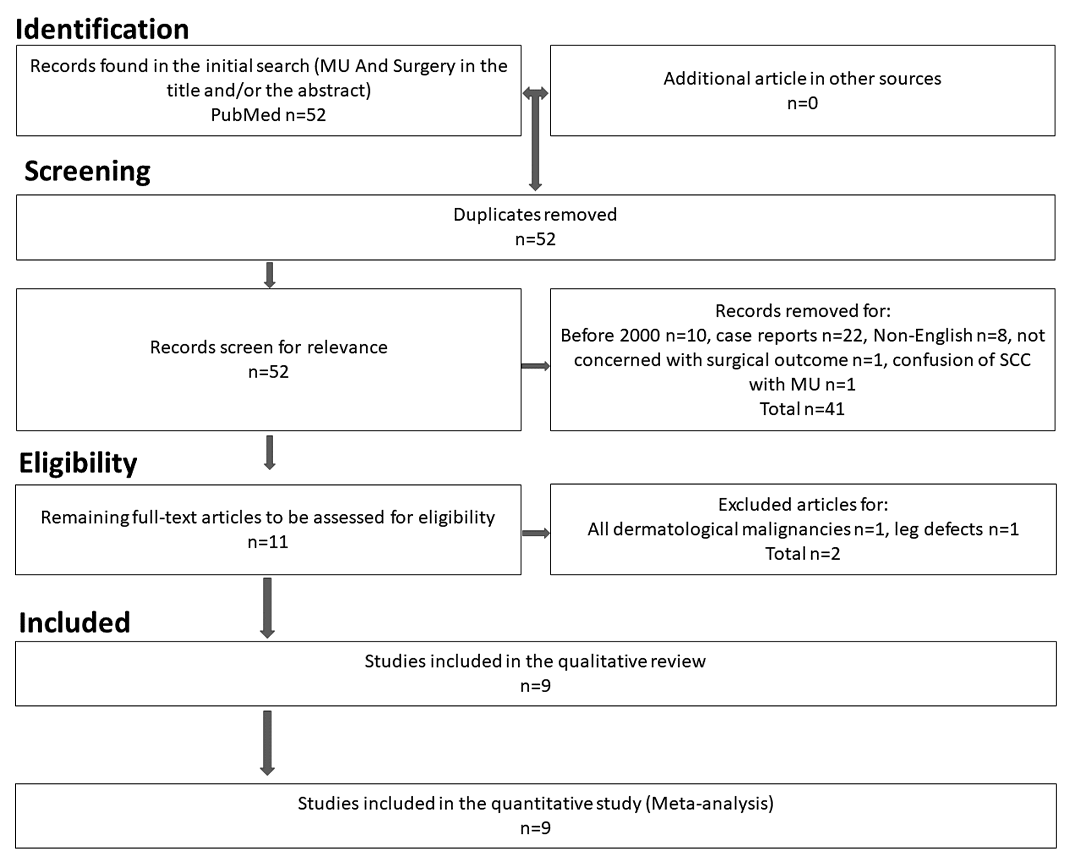
fig 1. flow chart of article selection.
Results
Amongst 9 publications eligible for analysis, 414 MU patients were presented. 381 patients underwent surgery. Mean age of the patients was 52.2 year with the youngest patient being 13 years old and the oldest one presenting with 89 years of age. 228 patients were male and the remaining 186 patients were female (male to female ratio 5:4). Out of 381 patients who underwent surgery, 48 amputations and 307 local excisions were done with the remaining 26 patients unknown for the type of surgery. Not enough information about second surgery was provided by the authors, but 22 out of 84 patients were reported to have had second surgery. 186 patients were assessed for adjuvant therapy, 83 of whom received the aforementioned therapy. Recurrence happened in 73 patients out of 298 patients that were followed up, 46 out of 50 analyzed for having gone under surgery, had surgery. Also 12 of those 73 recurrences were assessed for having gone under adjuvant therapy, all of whom have been exposed to this treatment. Also out of 77 people being followed up for death, 40 passed away.
Discussion
As mentioned above, there are different reasons why 33 patients did not undergo surgery. One reason was reported to be that the patient did not consent to the surgery (14) or the tumor was inoperable, or the patient was of advanced age to undergo surgery (7). Considering the risks and the benefits, excision surgery still remains the first line of treatment for MU, considering the nature of this disease. If the tumor metastasizes to the bone, local resection and excision might not suffice, for which complication the surgeon has to amputate the affected limb. One study did not provide us with the type of surgery (17) and from the remaining 355 patients, 48 underwent amputation, suggesting that there was bone involvement (13.5%) and 307 patients underwent local excision with or without lymph node resection. It could be inferred that nearly one eighth of patients will need amputation (P<0.001, OR 1.86 (1.83-1.90)).
The literature does not clearly suggest the mean age for diagnosis of MU, however in our final list of articles, the mean age at which the diagnosis of MU occurs is 52.2 years with the youngest patient being 13 (15) and the oldest with 89 years of age. (16)
Studies show that there might be a 1:1.4 ratio, male to female, for the gender of patients affected with Marjolin ulcer (19), however our findings clearly contradict this statement. In our sample data, 228 male patients were present, compared to 186 females, resulting in the final ratio of male to female 1.22:1 (P<0.001 , OR 1.44 (1.40-1.50)). Being significant looking at the P-value, the percentage of male patients is almost 55% and females just under 45%, demonstrating a 10% gap which affects more men than does women.
Not all studies included their follow up for second surgeries, however out of the ones that did (7, 15, 17), concluding to 86 patients, 22 required second (or further) surgeries in follow up, resulting in 25.5% need for second surgery or more (P<0.001, OR 0.74 (0.65-0.84)).
The literature is not quite clear on the use of radiotherapy and chemotherapy for MU. Not enough data is available to support their use in MU, however, some physicians might decide to utilize adjuvant therapy as a last resort for patients who cannot undergo surgeries, for the reasons mentioned above, or the ones that did but are trying to improve their outcome. 3 articles did not provide information about treatments other than surgery (12, 17, 18), out of 186 patients that were followed up for adjuvant therapy, meaning radiotherapy, chemotherapy, or both, 83 did receive the complementary treatment. However, not all publications are clear on the outcome of the patients that did or did not receive the adjuvant therapy. One paper suggested implementing adjuvant therapy, but did not specify which kind, and out of 7 patients who received the treatment, none of whom had recurrence. (11) Another article suggested that using chemotherapy for 2 of their patients had no apparent benefit (13). Another study devised radiotherapy for all of their patients and had 6 patients with recurrence of MU. (15) Another center included radiotherapy for 18 patients and chemotherapy for 3 patients, out of 34, and had 6 of them with the recurrence of the disease. A center prescribed radiotherapy alone for 8 patients (out of 15), 1 patient went under chemotherapy alone, and 2 patients underwent both treatments. All of these patients had recurrence of MU and passed away 8 to 20 months later. (7) Only two articles have specified the history of adjuvant therapy and recurrence for their patients, demonstrating the fact that, except for one patient. all of the ones that had recurrence, had undergone some form of adjuvant therapy. (7, 11) There is no justification, to our knowledge, that one might undergo systemic or radiotherapy when there is no clear understanding of the direct harms and benefits of these treatments, considering their risk and their cost for the patient and the burden on the system of health.
Lymph node enlargement might happen in many carcinomas. MU is not exempt from this phenomenon. Out of 414 patients, 106 patients had lymph node enlargement, palpable to the touch (25.6%). One paper reported lymph node enlargement for 18 patients, 11 of whom had recurrence, 5 of whom were positive for palpable lymph nodes (13). Another study reported 9 cases of palpable lymph nodes, 5 of which recurred with MU (17). The final study reported 3 cases of lymph node enlargement with 2 of them being recurred (7). Out of 73 cases being screened for palpable lymph nodes and recurrence, 29 had recurrence, 12 of which had palpable lymph nodes, out of 17 total cases of palpable lymph nodes, resulting in 70.6% probability of recurring MU in patients who have palpable lymph nodes. (P=0.003)
Death was not available in most publications, understanding the fact that follow up until death might be time consuming and resource limiting. One paper reported 29 deaths out of 62 patients, all of which have been before or during 6-year post-op period. Another center, as mentioned before, had 11 deaths occur out of 15 between 8 to 20 months after the treatment, in all of whom MU had recurred, coming to a sum of 40 out of 77, which translates to 51.9% death rate in MU patients (P<0.001, OR 0.51 (0.41-0.63)).
Conclusion
Different centers suggested different possible risk factors for the recurrence of MU in their patients, but the most common ones could be named as lymph node involvement and latency period. Suggestions for treatment is resection surgery of the affected area, either local excision or amputation of the limb with removal of palpable lymph nodes.
As of current date, there is no data that suggests adjuvant therapy is effective for treatment of MU, hence any burden on the patient and the system of health regarding this fact might yield to no desirable results.
Limitations
Like any other meta-analysis, not all data were provided in the included articles. This made analysis slightly more difficult, as the researchers had to dig deeper into the already limited number of paper, looking for the data that most probably was not going to be there, making the sample size even smaller, especially the recurrence and death outcome of the patients presented in the articles. Despite this hurdle, decent number of patients were able to be found to conclude a certain risk factor for the outcome of death or recurrence.
Fundings
This research has no fundings inserted from any private or public institution.
Conflict of Interest
The authors claim no conflict of interest.