Clinical Research and Clinical Case Reports
OPEN ACCESS | Volume 7 - Issue 1 - 2026
ISSN No: 2836-2667 | Journal DOI: 10.61148/2836-2667/CRCCR
Sujay Kumar Das, Ravi Shanker Singh, Bhavya Sharma, Lokesh Meena*, Pankaj Sharma
Institution: Department of Radiodiagnosis, AIIMS Rishikesh 249203, Uttarakhand India
*Corresponding authors: Lokesh Meena, Institution: Department of Radiodiagnosis, AIIMS Rishikesh 249203, Uttarakhand India.
Received: July 27, 2021
Accepted: August 09, 2021
Published: August 12, 2021
Citation: Sujay Kumar Das, Ravi Shanker Singh, Bhavya Sharma, Lokesh Meena, Pankaj Sharma. “Radiological Intervention in spontaneous pneumomediastinum associated with COVID 19 pneumonia: A case series”. Clinical Research and Clinical Case Reports, 1(5); DOI: http;//doi.org/04.2021/1.1025
Copyright: © 2021 Lokesh Meena. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background: Spontaneous pneumomediastinum is a newly described complication of COVID-19 pneumonia. The objective of this case presentation is to highlight an important complication and to explore potential predisposing risk factors and possible underlying pathophysiology of this phenomenon.
Case presentation: We present three patients with COVID-19 pneumonia complicated by spontaneous pneumomediastinum, pneumothorax, and subcutaneous emphysema, with and without positive pressure ventilation. Two patients had comorbidities, received supportive oxygen therapy, and underwent routine laboratory workup. They then developed spontaneous pneumomediastinum, and ultimately required intubation and mechanical ventilation, which proved to be challenging to manage, ultimately managed by interventional radiology team with CT guided pigtail catheter insertion.
Conclusions: Spontaneous pneumomediastinum is a serious complication of COVID-19 pneumonia, of which clinicians should be aware. Further studies are needed to determine risk factors and laboratory data predictive of the development of spontaneous pneumomediastinum in COVID-19 pneumonia.
Abbreviations: SPM: Spontaneous pneumomediastinum; ARDS: Acute respiratory distress syndrome; SARS: Severe Acute Respiratory Syndrome; CXR: Chest X-Ray; CT: Computed Tomography.
Aims and Objectives
To understand and evaluate the role of interventional radiology (IR) in the immediate management of spontaneous pneumomediastinum associated with COVID 19 pneumonia.
Introduction
As the 2019 coronavirus pandemic unfolded globally, numerous reports of severe and unusual complications in infected patients have been published. Acute respiratory distress syndrome (ARDS) is a major and sometimes fatal complication observed in a major population of hospitalized patients with COVID-19 [1].
The cases discussed here outline the clinical course of three patients with COVID-19 pneumonia who developed spontaneous pneumomediastinum (SPM), pneumothorax, and subcutaneous emphysema, with and without positive pressure ventilation. These findings are rare [2,3].
Tension pneumomediastinum is a life-threatening condition, especially in critically ill patients. One of the most common situations in which it occurs is prolonged invasive and non-invasive ventilation, with high end-expiratory pressure [4,5]. Due to the high number of patients with SARS-CoV-2 related respiratory infections being treated with this type of ventilation, we are seeing an increase in the number of tension pneumomediastinum cases [6].
Air leakage from the alveolus occurs due to a pressure gradient between the alveolus and the perivascular sheaths. If the pressure gradient is maintained, the air tracks along the vascular sheaths to the mediastinum. Due to increasing mediastinal pressure, compression of the great vessels occurs, leading to decreased venous return, hypotension, and finally to cardiac collapse [7,8]. The initial diagnosis may be difficult, due to associated subcutaneous emphysema that covers the underlying disease on chest X-ray.
Treatment may be conservative, reducing the airway pressures, allowing permissive hypercapnia, and increasing the oxygen percentage of the airflow to denitrogenate the mediastinal space [9,10]. Considering the fragility of patients with COVID-19, this approach is often insufficient, thus radiologic intervention may be necessary. In our experience, the approach we described immediately improves the clinical condition of the patient, with very low risks of complications.
Material and Method
Case presentation
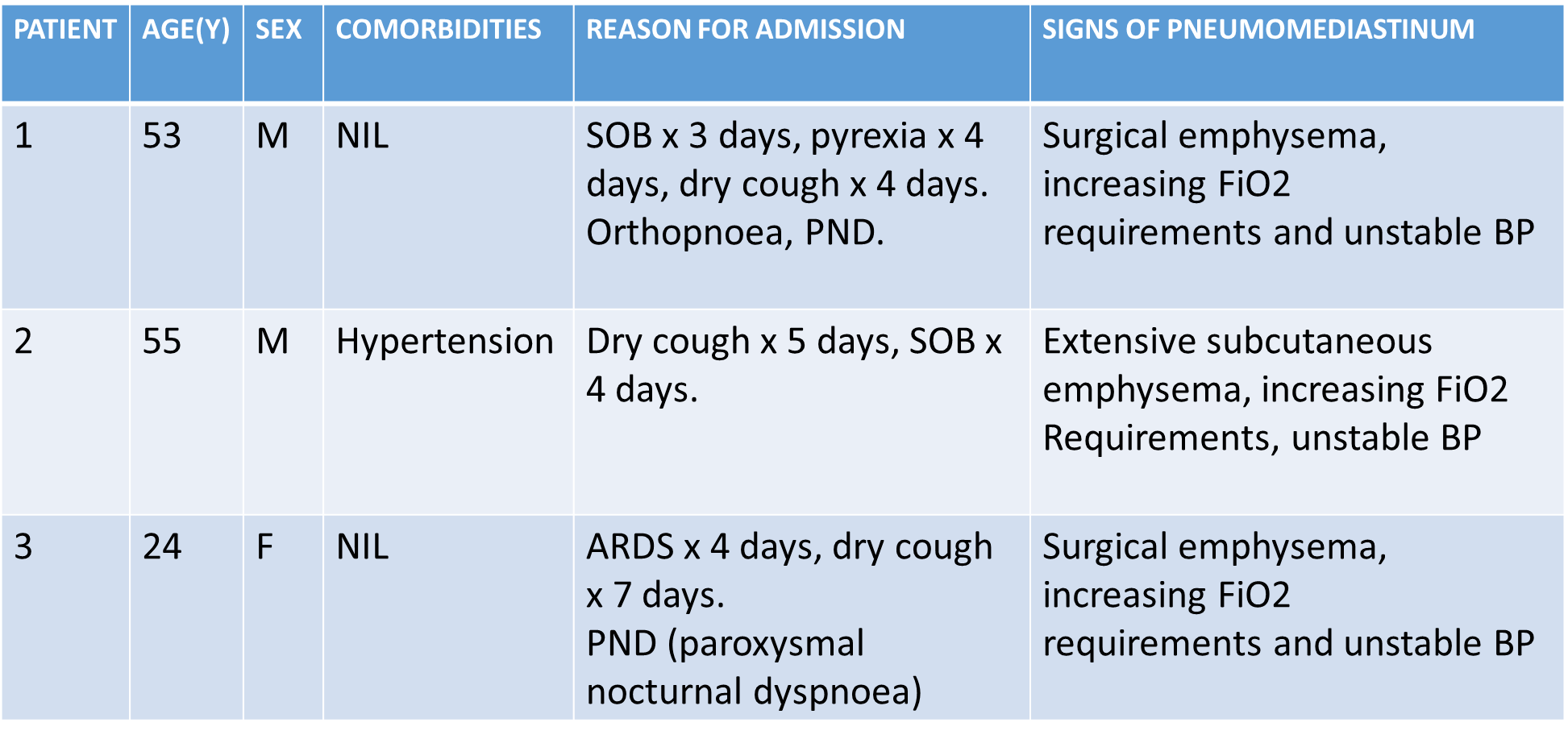
Patient 1
A 53-year-old man with hypertension and obesity presented to the emergency department with severe cough and progressive shortness of breath. He tested positive for COVID-19 via RT-PCR. He was having orthopnea and PND, and unstable BP. On HRCT thorax, the CORADS score was 33/40. He was saturating 89% on a 4 L/min nasal cannula (NC). He continued to require increasing levels of supplemental oxygen and was placed on a 15 L/min high flow nasal cannula (HFNC). A bedside CXR performed in the COVID ward on day five showed pneumomediastinum, small bilateral apical pneumothorax, and subcutaneous emphysema. A follow-up chest Computed Tomography (CT) revealed pneumopericardium and progression of multifocal interstitial opacities. His respiratory status continued to worsen and was intubated on day 7. Under CT guidance, an 8 F pigtail catheter was inserted in the mediastinum, which improved his vitals immediately.
Patient 2
A 55 years old man with hypertension was admitted to our intensive care unit for acute respiratory failure, due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. The patient was mechanically ventilated (intermittent positive pressure ventilation autoflow mode, with a tidal volume of 6 mL/kg, positive end-expiratory pressure (PEEP) 12 cm H2O, and respiratory rate 22 breaths/min. After 7 days, his condition abruptly worsened. He became hemodynamically unstable, with changes in the cardiac electrical activity and hypotension, unresponsive to catecholamines. An initial plain chest X-ray revealed widespread subcutaneous emphysema. Chest CT demonstrated a massive tension pneumomediastinum. Mediastinal decompression was performed via CT-guided pigtail catheter insertion in the mediastinum. After the procedure, the ventilation mode was modified, reducing the PEEP to 8 cm H2O, and respiratory rate to 16, increasing the FiO2 to 80%. The patient was hemodynamically stable, and remained on mechanical ventilation for 6 more days, followed by cycles of non-invasive ventilation for a further 5 days. He was transferred to a respiratory ward, where he went on to make a full recovery and was discharged 2 weeks later.
Patient 3
A 24 years old woman presented to our intensive care unit, with ARDS and dry cough. She was placed on 5 L/min NC and admitted to the hospital. Initial CXR revealed patchy left basilar airspace opacities. Her condition continued to deteriorate, and she required 15 L/min HFNC, to maintain oxygen saturation ≥ 90%. On day four, the patient developed pleuritic chest pain and an episode of ventricular tachyarrhythmia. A repeat CXR showed interval development of pneumomediastinum. On day five, she was intubated due to progressive ARDS. Chest CT revealed extensive subcutaneous emphysema, large pneumomediastinum. Cardiothoracic surgery opted for consultation with our IR team, as she was hemodynamically unstable.
All of these patients were positive for COVID-19 pneumonia. They developed spontaneous shortness of breath and became hemodynamically unstable. On chest X-ray, pneumomediastinum was seen. X-ray images could not be retrieved as these were done bedside, and there was strict COVID protocol. The pulmonology team gave a diagnosis of barotrauma induced pneumomediastinum and opinioned for pigtail insertion after discussion with the IR team. In all these cases, under CT guidance, an 8 F pigtail catheter was inserted in the anterior mediastinum through the parasternal intercostal space by the Seldinger technique. Pneumomediastinum was relieved with immediate hemodynamic improvement
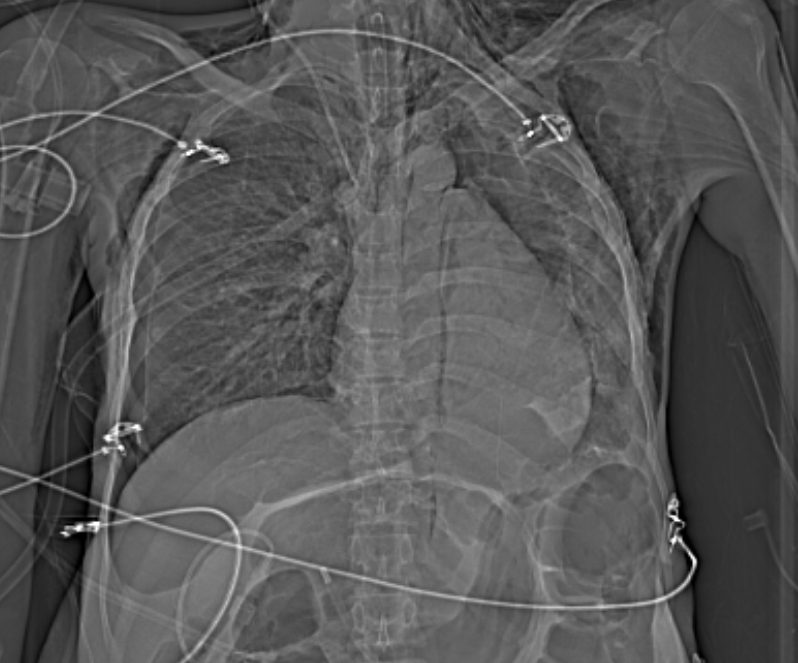
Figure 1: Pre-intervention scannogram shows pneumothorax, pneumomediastinum, and diffuse subcutaneous emphysema (marked with stars).

Figure 2: Pre-Intervention HRCT thorax: Axial sections show: Severe pneumomediastinum, Mediastinal shift towards the left side, reduction in lung volume, right tension pneumothorax, Flattening of the normal curvature of the right heart border suggestive of tamponade. Bilateral ground-glass opacities (GGO) are typical of COVID-19 pneumonitis.

Figure 3: Pneumomediastinum with air along major vessels (marked with a star).
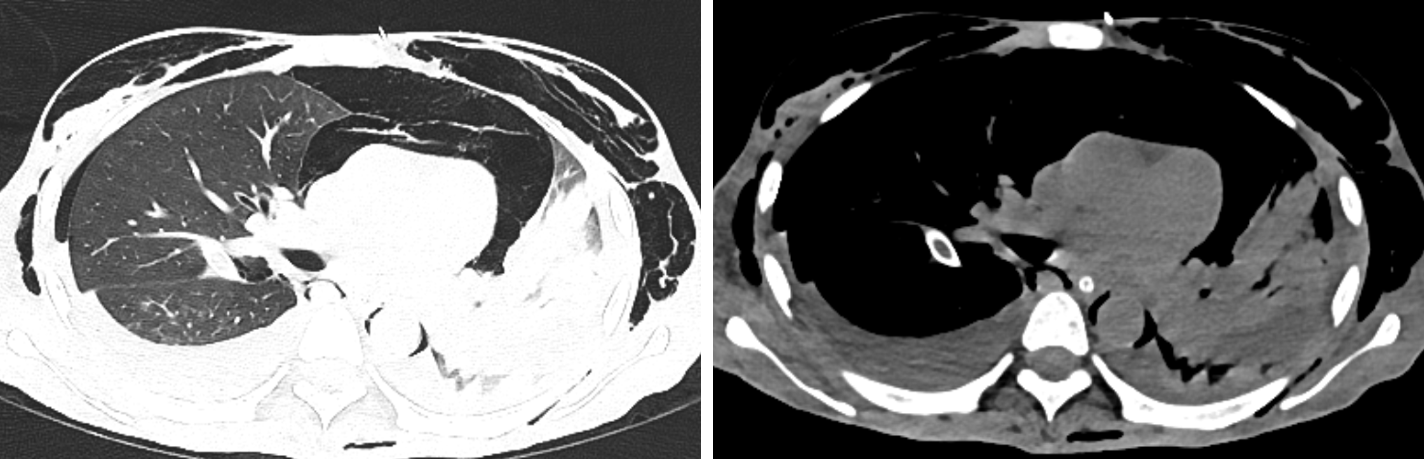
Figure 4: HRCT and NCCT thorax showing bilateral mild pleural effusion, left basal consolidation (marked with stars).
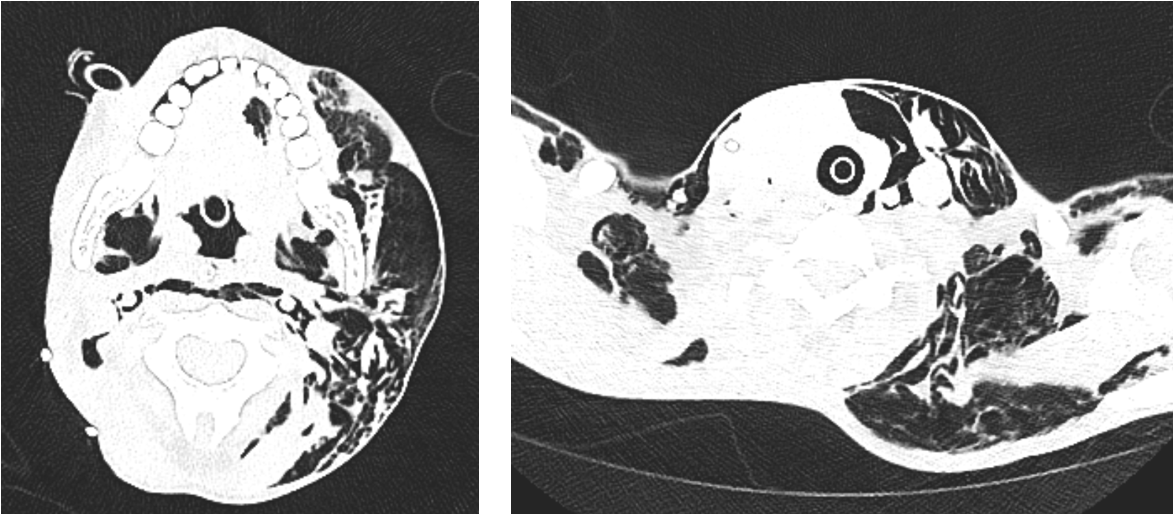
Figure 5: diffuse subcutaneous emphysema, along with neck spaces and intermuscular spaces (marked with stars).
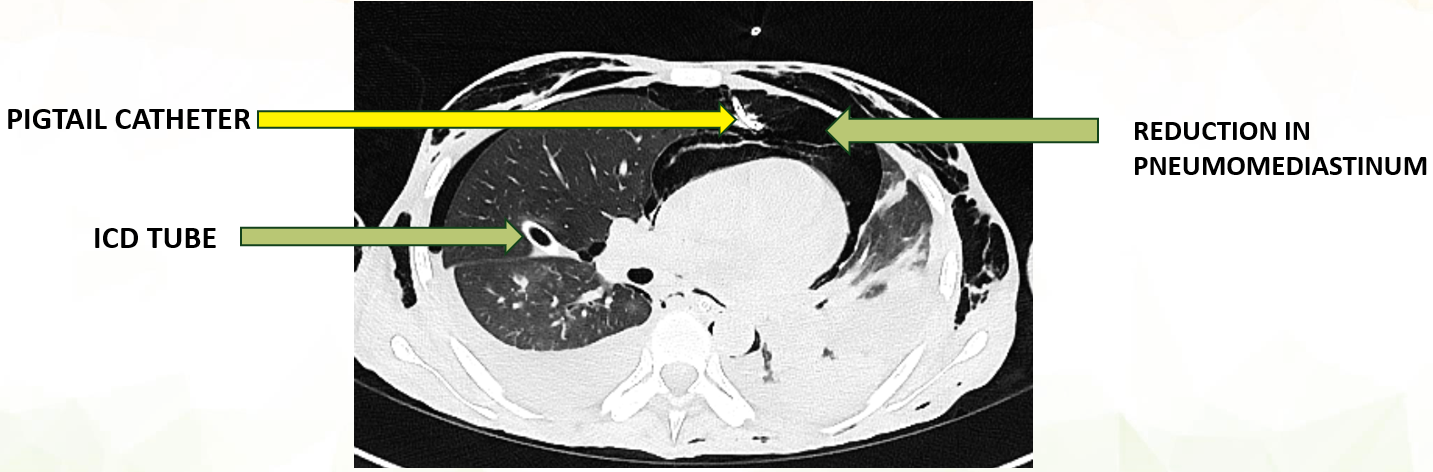
Figure 6: Post-Intervention HRCT thorax: Axial sections show: Pigtail catheter seen through left parasternal intercostal space, Reduction in pneumomediastinum, ICD tube seen on the right side.
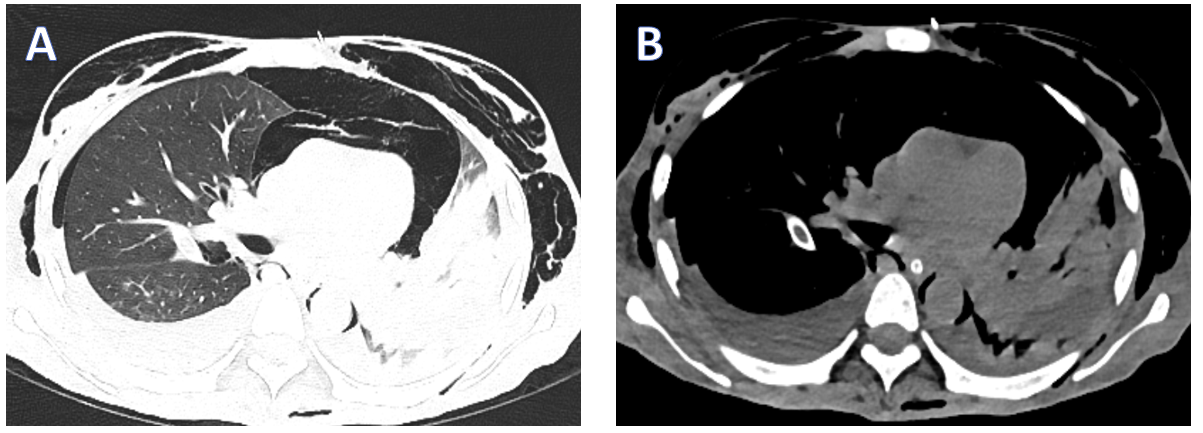

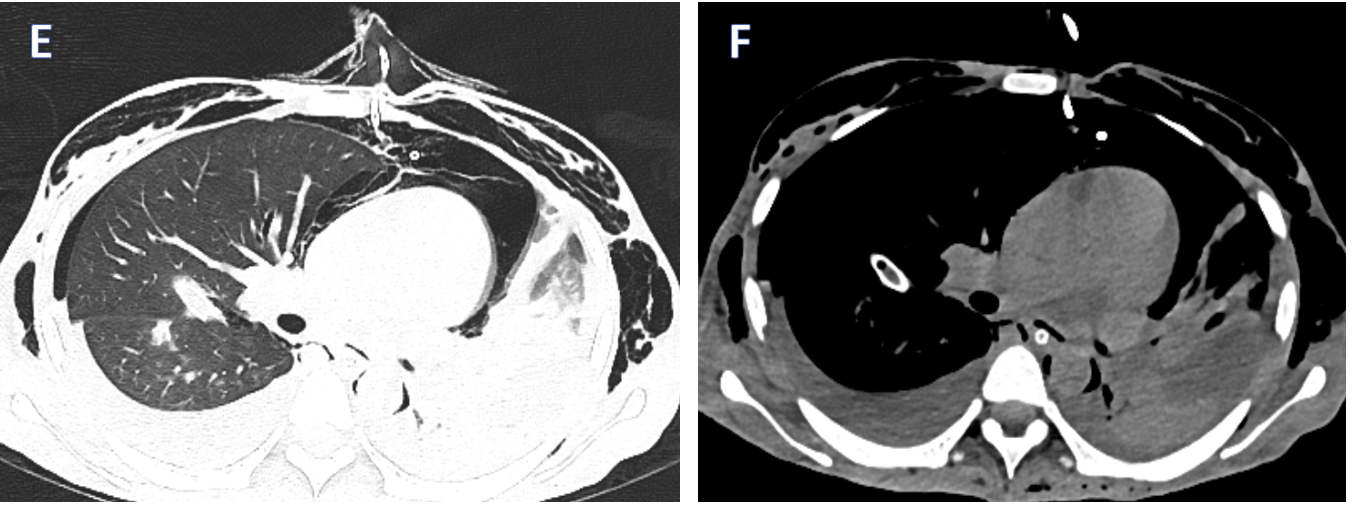
Figure 7: Serial images from A to F showing axial sections of HRCT and NCCT thorax. There is a reduction in pneumomediastinum following pigtail insertion.
Discussion
Secondary pneumomediastinum is most often associated with chest trauma, oesophageal perforation, cardiothoracic surgery, or mechanical ventilation. Spontaneous pneumomediastinum (SPM), however, is a less common phenomena [11]. The pathophysiology of SPM in SARS patients is thought to be related to diffuse alveolar damage (DAD), which leads to gas leak into the pulmonary interstitium causing pneumomediastinum [12]. This concept is supported by post-mortem studies on SARS lungs revealing extensive features of acute exudative alveolar and vascular injury [13]. Like the SARS virus, the novel COVID-19 virus causes ARDS in a sizable percentage of infected patients, but the mechanisms of alveolar injury are still under investigation. However, autopsy reports of COVID-19 patients from Italy and the United States revealed that DAD appears to also be the predominant pathologic pattern of pulmonary injury in COVID-19 patients [14,15].
Pulmonary barotrauma from mechanical ventilation, especially with high positive end-expiratory end pressure (PEEP), is a well-known risk factor for pneumomediastinum and pneumopericardium. High intra-alveolar pressure causes susceptible alveoli to rupture, allowing air to dissect along the bronchovascular sheaths towards the mediastinum, known as Macklin phenomena [7,11]. Occasionally, pressure accumulation in the mediastinum causes air to escape into the pleural space (pneumothorax), or through weaknesses of the parietal pericardium (pneumopericardium). Air can also travel towards the thoracic inlet and into the neck soft tissue causing cervicofacial subcutaneous emphysema [11], as happened in one of our patients.
A cough is a forceful expiration of air that causes sudden transient alveolar over-distention and occasionally rupture. It is a well-known risk factor for pneumomediastinum and pneumothorax [16]. All of our patients had significant coughs upon presentation to the hospital, and during the early part of their hospital stay. The coughing spells, exerting strain upon the already damaged and weakened alveoli from COVID-19 pneumonia, could have directly contributed to the development of pneumomediastinum in our two patients.
There are noteworthy diagnostic difficulties relating to SPM, especially in COVID-19 patients. Curvilinear radiolucency outlining the cardiac border is typical of pneumomediastinum on frontal CXR. This view, however, may only identify 50% of pneumomediastinum cases [17]. A lateral CXR, where gas is seen in the retrosternal space, is more sensitive [17]. When the diagnosis of pneumomediastinum remains uncertain, a chest CT is the modality of choice. Both lateral CXR and CT scans require transferring patients to and from the radiology suite. When applied to COVID-19 patients, these episodes of intrahospital transport create potential breaches in infection control measures, a decision which must be weighed against the risk of missing a diagnosis of SPM [19]. Due to this risk of breaches in infection control measures, X-ray images of patients could not be retrieved from the portable x-ray system.
Finally, while SPM is usually self-limited in healthy individuals, patients with SARS and SPM had worse outcomes. All of our COVID-19 patients eventually required intubation and mechanical ventilation, and they suffered a significant worsening of the subcutaneous emphysema on the ventilator. It is prudent to keep in mind that significantly elevated pressure in the mediastinal cavity (tension pneumomediastinum) can cause compression of intrathoracic structures, leading to rapid respiratory and hemodynamic instabilities, complications that are more likely to occur with the use of positive pressure ventilation [18]. In such situations, a mediastinotomy with insertion of a drainage catheter should be strongly considered [19]. Management in our patients with pigtail catheter insertion in mediastinum improved the vitals dramatically, without the requirement of mediastinotomy. However, patient 1 in our case series succumbed later due to COVID-19 related complications.
Treatment and Prognosis
Management in our patients with pigtail catheter insertion in mediastinum improved the vitals dramatically. However, patient 1 in our case series succumbed later due to COVID-19 related complications.
Conclusion
COVID-19 patients display diverse complications; pneumomediastinum is an emerging one. Further research is needed to study COVID-19 and barotrauma within the clinical and pathological phenotypes of the disease. Pigtail catheter insertion under CT guidance rapidly improves clinical outcomes.
Take-home points
Acknowledgment
No acknowledgments.
Funding
No funding was received.
Availability of data and materials
Not applicable.
Conflicts of Interest
The authors declare that they have no conflicts of interest
Provenance and Peer review
Not commissioned; externally peer-reviewed.