Clinical Research and Clinical Case Reports
OPEN ACCESS | Volume 7 - Issue 1 - 2026
ISSN No: 2836-2667 | Journal DOI: 10.61148/2836-2667/CRCCR
Rabail Raza*, Aamer Iftikhar, Muhammad Atif Naveed
Department of Radiology. Shaukat Khanum Memorial Cancer Hospital and Research Centre.
*Corresponding authors: Rabail Raza, Department of Radiology. Shaukat Khanum Memorial Cancer Hospital and Research Centre.
Received: May 28, 2021
Accepted: June 14, 2021
Published: June 16, 2021
Citation: Rabail Raza, Aamer Iftikhar, Muhammad Atif Naveed. “ Last but not the least! Checklist for Radiologist”. Clinical Research and Clinical Case Reports, 1(4); DOI: http;//doi.org/04.2021/1.1016.
Copyright: © 2021 Rabail Raza. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background: As clinician, we analyze all the available information. For diagnostic radiology, same is true; we are trained and expected to review all the available data; i.e. images. The last images of data may have partly covered pathology as well as outside the area in question. The findings may be incidental or clinically significant which may impact on patients’ outcome. This article emphasizes on reviewing last image as part of satisfaction of search by giving examples from our center which changed patient’s management. In the literature, much emphasis has already been made for reviewing scout images but not about last image. We consider this as another review area or check list of every radiologist.
Objective: To illustrate the value of the last image, we present a series of representative cases.
Patients: Five patients with clinically significant findings on the last view.
Conclusion: Missed diagnoses can delay patient management and are the leading cause of lawsuits brought against radiologists worldwide. A missed finding on last image of a cross sectional study is a potential risk, which can be avoided by developing the habit of systematically viewing the last image as a mandatory checklist.
Introduction:
The answer is always on the film. —Harold G. Jacobson, MD, 1912–2001
Since last two decades, there have been a number of articles published in radiological literature that emphasize on the importance of reviewing scout images, however, not much has been mentioned about last image of any cross sectional imaging which may show critical diagnostic information, that is easily missed. This delineates the concept of diligence and meticulously reviewing all images including the edges, as a part of standard of care.
Therefore, focused viewing and search for pathology on last image of radiological scan may provide additional, sometimes clinically valuable information. To illustrate this, we present a series of cases that we have encountered.
Discussion:
Case 1:
A 63-year-old male patient known case of metastatic adenocarcinoma prostate, developed meningitis which was confirmed on CSF analysis. Patient underwent MRI brain with contrast which showed unremarkable intracranial structure, however, there were T2/Flair hyper intense cystic collection at the base of the skull in retropharyngeal space showing peripheral thick enhancing walls and patchy diffusion restriction. This is suggestive of retropharyngeal abscess and extends from C2 to C4 levels. This collection is extending posteriorly in bilateral paraspinal muscles around the C2 vertebra, more on the left side. There is mass effect narrowing of the nasopharyngeal airway. There is linear enhancement of the posterior longitudinal ligament against C2-4 levels. Patchy enhancement of the dens is noted. Ventricular system is not dilated. No midline shifts. No tonsillar herniation. Patient was immediately started on antibiotics and he was improving clinically. His follow-up imaging showed complete resolution of abscess. RPAs are potentially life-threatening deep space neck infections. The mortality rate for retropharyngeal abscess is less than 1% [1] and has declined in the last 50 years because of the availability of antibiotics and early diagnosis.
 Figure 1: (a and b) Post contrast MRI images demonstrate large neck mass with features of retropharyngeal abscess with lateral extension into parapharyngeal space. Central necrotic and peripherally enhancing mass with positive diffusion restriction (c).
Figure 1: (a and b) Post contrast MRI images demonstrate large neck mass with features of retropharyngeal abscess with lateral extension into parapharyngeal space. Central necrotic and peripherally enhancing mass with positive diffusion restriction (c).
Case 2:
56-year-old male with hepatitis C, presented with painless jaundice and weight loss. Patient had an elevated CA 19.9 of 5119, and underwent CT. The scan revealed pancreatic head/ uncinate process enhancing tumor without vascular encasement along with extensive local regional lymphadenopathy and pulmonary and hepatic metastasis deposits. There was intra/extra hepatic biliary channel and pancreatic duct dilatation, for which retrograde cholangiopancreatography, endoscopic ultrasound and biopsy were recommended. Histopathology proved this malignancy as adenocarcinoma of pancreas. Patient was offered placement of external biliary drainage catheter to relieve biliary channel obstruction followed by palliative chemotherapy and was advised surveillance, since it was a metastatic disease process.
On his subsequent imaging, he was known to have developed aggressive osseous lesions concerning for metastasis. Interesting the finding was picked up on last image of scan. Bone scan proved osseous metastatic deposit.
The mainstay of management for sacral metastatic tumors is palliation. Preoperative angioembolization is shown to be of value in cases of highly vascularized tumors. Radiotherapy is used as the primary treatment in cases of inoperable tumors without spinal instability where pain relief and neurological improvement are attainable [2].
 Figure 2: (a and b) CT scan axial and coronal images showing focal sclerotic lesion in S1 vertebral body, (c) bone scan images demonstrate Focal increased tracer uptake with underlying sclerotic changes in sacrum is consistent with metastatic disease involvement.
Figure 2: (a and b) CT scan axial and coronal images showing focal sclerotic lesion in S1 vertebral body, (c) bone scan images demonstrate Focal increased tracer uptake with underlying sclerotic changes in sacrum is consistent with metastatic disease involvement.
Case 3:
44-year-old female, known hypertensive presented with clinical complaints of sudden loss of consciousness. No complaint of headache, nausea, fits. Patient recovered without any neurological deficit.
Her physical examination showed no obvious physical deformity. She underwent MRI brain which showed multiple lacunar infarcts. A note was made of bone centered abnormality involving clivus, right sphenoid sinus and floor of right temporal lobe/greater wing of sphenoid. This returns foci of heterogeneous high T1 and FLAIR signals in this area. No high signal is demonstrated on T2-weighted sequence. Mild patchy contrast enhancement seen. No diffusion restriction is seen, however. Imaging features suggestive of fibrous dysplasia. Since fibrous dysplasia is considered as “do not touch” lesions, no treatment is required as the bone lesions usually do not progress beyond puberty. It is worth mentioning that localized FD on MR imaging, however, may mimic a tumour because fibrous tissue has low to intermediate T1 and heterogeneous T2 signal and enhances after the administration of contrast material [3]. Recognizing the benign expansion of bone with preservation of normal contours and the characteristically dark T2 signal of the fibrous tissue.
Treatment for fibrous dysplasia depends on the severity of the disorder and the presence of symptoms. In some cases, doctors simply monitor your bone health to make sure FD does not get worse. Doctors frequently prescribe bisphosphonates in an effort to ease pain and help prevent fractures. Our patient was also advised pain relief therapy.
 Figure 3: MRI brain axial images show abnormal signal intensity lesion involving clivus, floor of right temporal lobe/greater wing of sphenoid, (a) heterogeneous high T1 signals, (b) low T2 signals and (c) Mild patchy contrast enhancement. Imaging features consistent with fibrous dysplasia.
Figure 3: MRI brain axial images show abnormal signal intensity lesion involving clivus, floor of right temporal lobe/greater wing of sphenoid, (a) heterogeneous high T1 signals, (b) low T2 signals and (c) Mild patchy contrast enhancement. Imaging features consistent with fibrous dysplasia.
Case 4: 78768 Bilateral breast CA with brain meets
Known case of bilateral breast cancer, with progressive metastatic pulmonary disease along with mediastinal lymphadenopathy and osseous metastasis. Patient was hormonal treatment and chemotherapy. Follow up CT imaging was advised for restaging purposes, which showed small focus of gyri form enhancement in the right parietal region concerning for metastasis. Later MRI brain with contrast was performed which confirmed metastatic brain disease. The patient was then started on intra-thecal chemotherapy.
It is estimated that 10-35% of patients diagnosed with breast cancer will develop metastasis to the brain [4]. Intravenous chemotherapy and, independently, intrathecal chemotherapy improve survival in breast cancer patients. Radiotherapy has a positive impact on the quality of life due to the alleviation of neurological symptoms. The role of radiotherapy in prolonging survival is questionable [5].
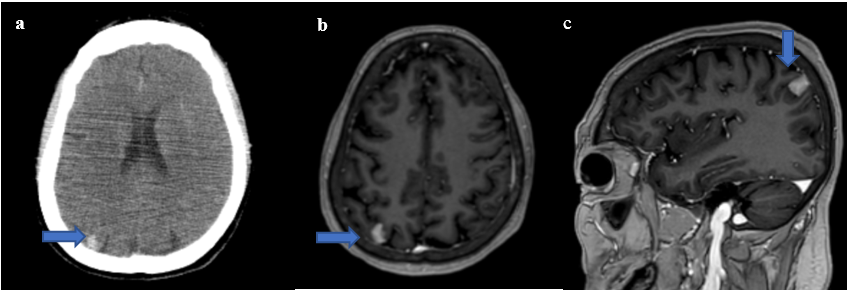 Figure 4: (a) CT brain with contrast, axial image showing enhancing focus in right parietal lobe is concerning for metastasis. MRI brain axial and sagittal (b and c) confirmed brain metastasis.
Figure 4: (a) CT brain with contrast, axial image showing enhancing focus in right parietal lobe is concerning for metastasis. MRI brain axial and sagittal (b and c) confirmed brain metastasis.
Case 5:
78-year-old gentleman with complains of hip pain, noted to have an elevated PSA. MR pelvis revealed locally aggressive mass centered over peripheral zone of left prostate with involvement of left seminal vesicle, mesorectum and external anal sphincter. TRUS prostate biopsy showed prostatic adenocarcinoma with predicted stage is T4, N1, M0.
Patient underwent bone scan which was negative for osseous metastasis. However, SPECT-CT images of bone scan showed retroperitoneal and left common iliac lymph node. Retrospectively, left common iliac lymph node could also be appreciated on MRI. This was a non-regional lymph node, which upstaged the disease to T4 N1 M1. Patient was then offered hormonal therapy, chemotherapy for nodal disease.
From this case, we learn the importance of reviewing all sequences, as missing a critical finding can have a drastic impact on patient’s treatment.
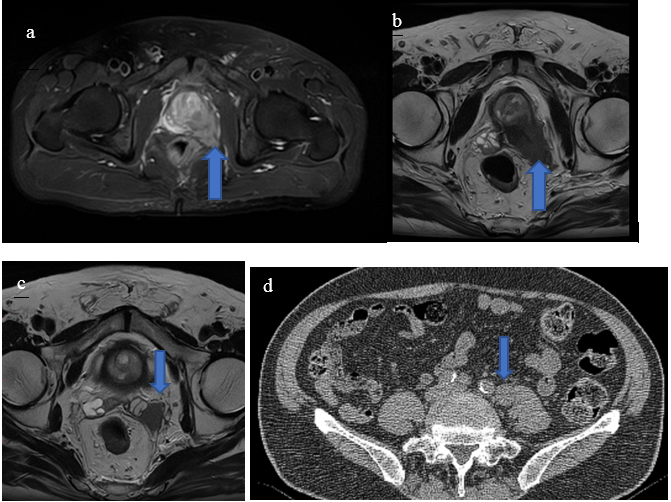 Figure 5: MRI pelvis for staging prostate adenocarcinoma Axial (a) STIR (b) T2W images show a lesion in the peripheral zone. The bulging and irregularity of the capsule (arrows) highly concerning for extra prostatic tumor extension, (c) enlarged left mesorecta lymph node, (d) SPECT-CT image showing left common iliac lymph node.
Figure 5: MRI pelvis for staging prostate adenocarcinoma Axial (a) STIR (b) T2W images show a lesion in the peripheral zone. The bulging and irregularity of the capsule (arrows) highly concerning for extra prostatic tumor extension, (c) enlarged left mesorecta lymph node, (d) SPECT-CT image showing left common iliac lymph node.
Conclusion:
In conclusion, by presenting the above cases, we emphasize the value of the last image of cross-sectional imaging and the importance of its evaluation as critical pathologies are hidden and can be easily missed.
Therefore, reviewing the last image should be in the check list of every radiologist.