Clinical Research and Clinical Case Reports
OPEN ACCESS | Volume 7 - Issue 1 - 2026
ISSN No: 2836-2667 | Journal DOI: 10.61148/2836-2667/CRCCR
Zannatul Ferdous Sonia1, ARM Luthful Kabir2, Mahmuda Hasan3,Akmat Ali4, Richmond Ronald Gomes5, Masuma Khan6
1Assistant Professor, Pediatrics, Ad-din Women’s Medical College Hospital, Dhaka
2Professor, Pediatrics, Ad-din Women’s Medical College Hospital, Dhaka
3Professor, Pediatrics, Ad-din Women’s Medical College Hospital, Dhaka
4Professor, Hepatology, Ad-din Women’s Medical College Hospital, Dhaka
5Associate Professor, Medicine, Ad-din Women’s Medical College Hospital, Dhaka
6Assistant Professor, Pediatrics, Ad-din Women’s Medical College Hospital, Dhaka
*Corresponding authors: Richmond Ronald Gomes, Associate Professor, Medicine Ad-din Women’s Medical College Hospital, Dhaka, Bangladesh
Received: March 28, 2021
Accepted: April 06, 2021
Published: April 09, 2021
Citation: Z Ferdous Sonia, ARM Luthful Kabir, Md Hasan, A Ali, R Ronald Gomes, M Khan. “A Rare Case of Choledochal Cyst complicated by Choledocholithiasis with Acute Pancreatitis”. Clinical Research and Clinical Case Reports, 1(1); DOI: http;//doi.org/04.2021/1.1004.
Copyright: © 2021 Richmond Ronald Gomes. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Choledochal cysts are dilatations of biliary tree that causes a diversity of clinical symptoms & lead to several complications. Choledochal cysts are most usually diagnosed in childhood & frequently present with abdominal pain, jaundice and abdominal mass. Albeit the most concerning complication is malignancy. Other complications are stone formation, acute pancreatitis. Stricture may also occur & can lead to morbidity. Treatment goal is not only relieving patient symptoms but also decreasing long term cancer risk. Here we present a young child presenting with abdominal pain & vomiting secondary to type 1b choledochal cyst complicated by acute pancreatitis with choledocholithiasis.
Introduction: Choledochal cysts are rare congenital dilatation of extra hepatic & or intra hepatic bile ducts. The incidence of choledochal cyst in Asian population has been reported to be 1 in 13,000 and 1:1000 in Japan [1]. Female are more frequently affected than male with a ratio 4:1 [2]. Although choledochal cysts are predominantly diagnosed in children, about 25% of patient’s diagnosis is delayed until adulthood [3]. Choledochal cyst causes a variety of clinical presentation & can lead to several types of complications. It can be diagnosed by chance or serendipitously due to complications such as acute pancreatitis [4,5], choledocholitiasis. Early diagnosis & treatment of choledochal cyst are crucial as they carry malignant potential that increases with age.
Here in, we present a child presenting with abdominal pain & vomiting secondary to type 1b choledochal cyst complicated by acute pancreatitis with choledocholithiasis.
Case Description: An 18 month old female child presented at pediatric department with the complaints of eruptive vomiting for 3 days and abdominal pain for same duration. Pain appeared to be cramping & intermittent, relived by lapping.
On physical examination, body weight 9 kg, height 79 cm,( WAZ: on 3rd centile, WHZ: on 3rd centile), icteric, irritable. Patient had significant sensitivity in abdomen.
Laboratory data showed the following values: Hb-8.4 g/l, microcytic hypochromic anemia, WBC-8.2×10˄3/mL, S. bilirubin was 3.9mg/dl with dominant direct bilirubin, SGPT 349 U/L, Anti HAV IgM: negative. Serum amylase 306u/l, S. lipase 2270 U/L, electrolyte was normal. Abdominal USG showed-fusiform dilatation of CBD measuring about (4.1×1.7cm) cystic duct dilated. There were multiple granules mobile echogenic structure without shadow seen in lumen of the CBD. MRCP showed fusiform dilatation (2.2cm) of proximal CBD involving common hepatic duct over 3.5 cm segment (Figure 1). Distal CBD was mildly (1cm) dilated containing 2 tiny flow void suggesting calculus (0.5cm) seen with lumen of distal CBD (Figure 2). Pancreatic duct was visualized & mildly dilated.

Figure 1: MRCP showing fusiform dilatation of proximal CBD involving common hepatic duct.
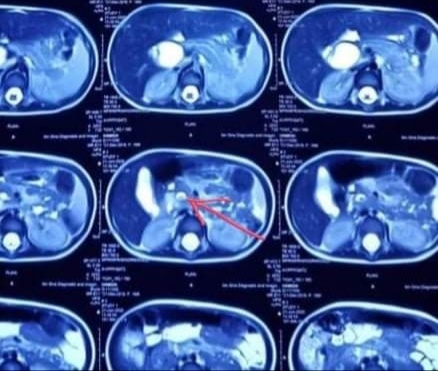
Figure 2: Distal CBD with signal void structure within suggestive of stones.
Thus the final diagnosis with acute pancreatitis with Choledocholithiasis caused by choledochal cyst type 1b was made. Fluid resuscitation was given initially due to profuse vomiting. Other treatment included parenteral antiemetic, proton pump inhibitor, opiate analgesic. After treatment, patient showed significant clinical improvement with decreased frequency of vomiting. Intensity of abdominal pain was also decreased. She was planned to undergo definite treatment by surgery. After complete resolution of 1st episode of pancreatitis the patient was operated 2 month later. The cyst was completely excised and cholecystectomy (Figure 3) and hepaticoduodenostomy were performed. Histopathology showed inflamed structure lined with biliary epithelium, free of any malignant lesion. The patient made an uneventful postoperative recovery.

Figure 3: Resected common bile duct cyst & gallbladder.
Discussion: Vater and Ezler (1723) defined Choledochal cyst as a congenital dilatation of extra & / or intrahepatic bile duct. Pathophysiology remains still mysterious. The most widely accepted hypothesis is abnormal biliopancreatic junction [6]. Our patient has no such abnormality.
Anomalous Pancreaticobiliary Ductal Union (APBDU) allows reflux of pancreatic enzyme into biliary tree with consequent biliary duct inflammation predisposing to abnormal dilatation [7,8]. Some studies reported that sphincter of oddi dysfunction may predispose to Choledochal cyst [9]. Choledochal cyst may be part of congenital anomaly of biliary system or multiple conginatal anomaly proposed by some other expert [10,11,12].
According to modified Todani classification (Figure). Choledochal cyst are classified into 5 types [13]. Clinical feature is variable & may depend on patient age. Frequently observed symptom in infant is jaundice and abdominal pain as in adult [14]. Classic triad consisting of jaundice, abdominal pain and palpable mass would only be found in 15 to 25 % case [15]. Our case, patient had jaundice and abdominal pain.
Potential complications of this malformation include acute pancreatitis, ascending cholangitis, cholecystitis, cholelithiasis ,biliary cirrhosis and cholangiocarcinoma have been reported [7]. Choledochal cyst in adult are often associated with complication compared to children has been reported [16].
The occurance of pancreatobiliary complications were to be brought by biliary stasis. This causes stone & sludge formation that lead to bile duct & pancreatic duct obstruction and resultanting pancreatitis [18].
Acute pancreatitis is a common complaint of adult patient. Acute pancreatitis is rare occurrence in patient with type 1 choledochal cyst & just a couple of cases have been reported in the literature. Only 9% of pediatric patient with choledochal cyst were reported to have choledolithiasis [18]. In this patient diagnosis of pancreatitis was based on abdominal pain and high level of amylase. To our Knowledge the current patient is the youngest person with concomitant acute pancreatitis with choledocholithiasis which is rare.
Different imaging technique USG, MRI(MRCP), CT are available for the determination of choledochal cyst [19]. MRCP is considered the gold standard for diagnosis of biliary cyst with sensitivity 90-100% 20.
Appropriate management consists of conservative treatment of complications followed by definitive surgery [16,17]. Saluja et al found that cyst excision with biliary reconstruction is necessary to prevent the recurrence of complication [16]. Now a days, complete resection of the cyst with cholecystectomy & biliary reconstruction (RYHJ or HD) is considered the treatment of choice [21]. This operation was successful in our patient with no post operative complication.
There are small numbers of studies in the literature on the pancreatic complication of choledochal cyst in children. Fujishiro et al [22]. stated that pre-operative pancreatitis was most commonly seen in children with choledochal cyst type a.
To date, couples of studies have discussed the optimal timing of surgery for choledochal cyst complicated with acute pancreatitis in children. Cho et al proposed that early cyst excision after development of acute pancreatitis in patient with choledochal cyst reduced patient symptoms, especially occurrence of pseudopancreatis [23]. However deciding the timing of surgery in choledochal cyst complicated with pancreatitis is challenging. Here we report our experience in treating type 1b choledochal cyst with acute pancreatitis with choledocholithiasis.
Conclusion: Congenital cystic dilatation of biliary tract is a rare anomaly that may stay quiet or uncovered by acute pancreatitis. The diagnosis is based on USG & MRCP. Early diagnosis and prompt treatment is required to prevent long term complications. Acute pancreatitis is a uncommon occurrence in patient with type 1 choledochal cyst. Our patient with choledochal cyst associated with pancreatitis with choledocholithiasis was treated surgically with uneventful clinical outcome.