Clinical Psychology and Mental Health Care
OPEN ACCESS | Volume 7 - Issue 1 - 2025
ISSN No: 2994-0184 | Journal DOI: 10.61148/2994-0184/CPMHC
Shivanie Hendricks, Tamica Daniels-Williamson, Roy Permual
(St Cuthbert’s Secondary School, Guyana) Family Medicine, Georgetown Public Hospital Corporation.
*Corresponding Author: Tamica Daniels-Williamson, (St Cuthbert’s Secondary School, Guyana) Family Medicine, Georgetown Public Hospital Corporation.
Received Date: February 09, 2023
Accepted Date: April 15, 2023
Published Date: July 24, 2023
Citation: Hendricks S, Tamica D Williamson, Permual R. (2023). “Prevalence of Depression Among Adolescents at ST Cuthbert’s Mission Secondary School”. Clinical Psychology and Mental Health Care, 5(1); DOI: http;//doi.org/01.2023/1.10078.
Copyright: © 2023 Tamica Daniels-Williamson. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Objectives:
To determine the prevalence and severity of depression among the students at St Cuthbert’s Secondary School.
To determine that ratio of female-to-male Depression and the age group most commonly affected.
To determine factors that contribute to Depression.
Design and Method: This was a cross-sectional study on students from St. Cuthbert’s Mission Secondary School. From a population of 125 students, 95 was determined to be the sample size corresponding to a 95% confidence level. However, only 89 students participated in data collection due to no parental consent for 6 students. The research utilized both demographic data and responses to a Patient Health Questionnaire-A. Data was analyzed using Microsoft Excel and SPSS software.
Results: Depression was found to be 88.8%, 9.0% and 2.2% for zero or minimal, mild-to-moderate and moderately severe depression, respectively. Depression was also found to affect female adolescents more (58%) than it affects male adolescents (42%). Furthermore, depression was discovered to rise with age. Four risk factors were found to have more impact on depression among adolescents. These four factors, by order of average severity scores, are number of occupants in the home, presence of both parents, family history of depression and family type.
Conclusion: Despite the presence of various risk factors, severe depression was not found to be prevalent among students at the students at St. Cuthbert’s Mission Secondary School.
Recommendations:
Screen adolescents for depression annually.
Include depression sensitization programs in schools.
Conduct similar research in schools countrywide.
Introduction:
St. Cuthbert’s Mission is a small Indigenous Community with a population of 1200 persons, located on the Linden Soesdyke Highway in Guyana. The Secondary school was established in 2008 and has a current student population of 125 students.
Depression is a common and serious medical illness that affects how individuals feel, think and act. It can occur in any age group, usually affects a person’s ability to function in their daily lives and has significant impact on the management of other medical issues the individual may have.1 In Guyana, depression was determined to be approximately 4.5% of the population in 2016.2
Any person between ages 10 and 19 years old is considered an adolescent.3 If an adolescent withdraws from society, displays acts of delinquency and senseless behavior, but was previously a well performing individual, he or she should be considered depressed.4 These symptoms are frequently associated with rebellion, and the family may view them as a normal and temporary stage of the adolescent’s development. Other more traditional symptoms include a sad demeanor, diminished capacity for pleasure, feelings of rejection and not being loved, weight loss or gain, persistent self-blame and suicidal ideation.4 Adolescent depression can result in social, behavioral and cognitive problems.5 These symptoms must last for at least two weeks in order to be considered depressed.6
Depression in girls increases after puberty and exceeds 4% at the end of first year of adolescence. Depression has the greatest impact in low- and middle-income countries. Family history of depression and exposure to psychological stress are both high risk factors for depression in adolescents. Inherited risks, developmental factors, sex hormones, and psychosocial adversity interact to raise risk via hormonal factors and disrupted neural pathways.7 A study was conducted in 2020 among USA adolescents which revealed that 4.1 million (17%) reported depression symptoms. Furthermore, the prevalence of depressive symptoms increased with age in adolescents and the increase was far greater in females than males. Ages 12-13, 14-15 and 16-17 were associated with 11.2, 18.2 and 21.9 percent of adolescent depression, respectively.8 The increase in males was also noticeable, indicating a rapid emergence of depressive symptoms among youths.9 Guyana, considered a middle income country, has many risk factors for depression e.g. low socio-economic status and poverty, low education levels and exposure to abuse in many forms.10,11 Depression in adolescents left undiagnosed and untreated can result in psychological disorders (anxiety, bipolar disorders), physical health issues, substance abuse disorders and suicide. Hence it is very important to screen for depression for early detection and necessary treatment.5
Since there is limited statistics in the adolescent population, this study was conducted in the St. Cuthbert’s Mission Secondary School to determine the prevalence of depression.
Methodology:
This research was approved by Ministry of Health Institutional Review Board (IRB) and the Chief Education Officer. Data was quantitative and was collected based on a pre-calculated sample size of 95 students representing a 95% confidence level (p-value of 0.05 or 5%) from 125 total students at the St Cuthbert’s Secondary school. Consent was only obtained from parents/guardians for 89 students. The results determined the prevalence of depression among these 89 students at the school. Statistical significance was also determined using the data obtained from prevalence of depression. Results also established the male-to-female ratio of depression, and the distribution of depression among various age groups. In addition, the effects of social factors on the severity of depression were also reported, where the major factors were identified and discussed. The research utilized both demographic and a PHQ-A questionnaires (Patient Health Questionnaire-A). The PHQ-A is a 9-item screening tool that assesses the severity of depressive disorders and episodes (or clinically significant symptoms of depressive disorders and episodes) in children ages 11–17.12 The depression severity scale is as follows: 0-4 for none to minimal, 5-9 for mild, 10-14 for moderate, 15-19 for moderately severe and 20-27 for severe depression.
Results
Prevalence and severity of depression
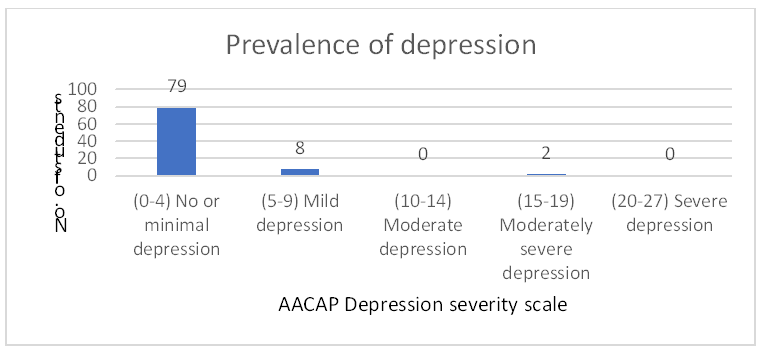
Figure 1: Prevalence of depression
Figure 1 shows that 79 students presented with a severity score between 0 and 4 and 8 students presented 5-8, and 2 students presented with 17 and 19 severity scores.
Male to Female depression
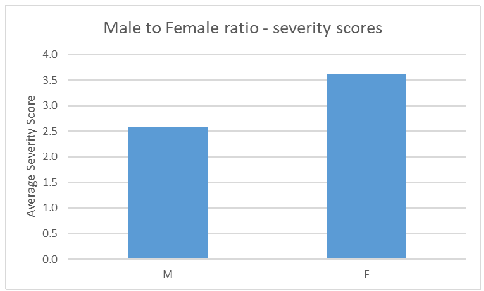
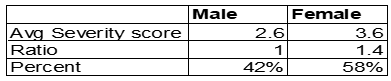
Figure 2: Ratio of male to female depression
Figure 2 shows depressive symptoms are more common among females compared to males since the average severity scores, across all severity ratings, among females was 3.6 compared to 2.6 for males, which is a 1:1.4 ratio.
Depression vs. age group
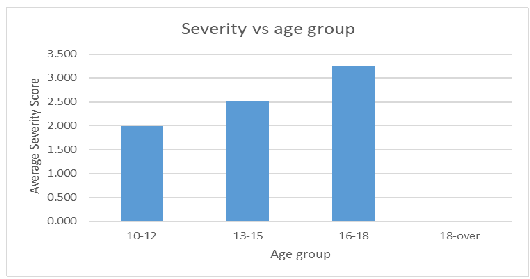
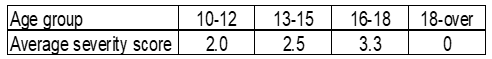
Figure 3: Average severity score according to age group
Figure 3 shows depression is more prevalent with increasing age group as indicated by increasing average severity scores.
Factors contributing to Depression
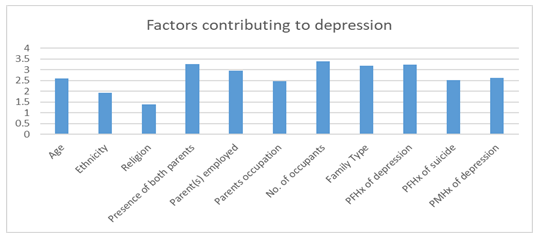
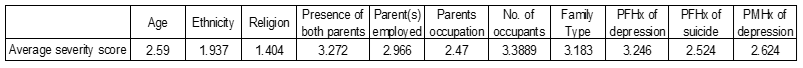
Figure 4: Average severity score according to social factors
Figure 4 shows the number of occupants living with the student is the most impactful factor contributing to depression due to the highest average severity score.
Discussion:
Prevalence of Depression
Using the American Academy of Child and Adolescent Psychiatry (AACAP) ratings,13 from a total of 89 students, 79 (88.8%) presented with no to minimal depression while 8 (9.0%) students presented with mild to moderate depression. Furthermore, 2 (2.2%) students presented with moderately severe depression. No student was found to be severely depressed. The AACAP ratings are also presented in Figure 1 above.
From this research data, only 2 persons displayed moderately severe depression, which equates to 2.2%. This is less than what was determined by the Centers for Disease Control and Prevention (CDC), which found this figure to be 4.4%, but that was from a study of 2.7 million adolescents.14 The 2.2% is also less than 24.5 – 40.6% of moderate to severe depression prevalence that was determined among adolescents in some Caribbean countries.15 Using the SPSS tool, 2 of the n=89 students (2.2%) equates to a p-value of 0.213 from the Pearson Chi-square test, which is more than 0.05 from a 95% confidence interval. This indicates that the 2.2% is not considered statistically significant. Overall, using the PHQ-A depression classification, the data shows that zero to minimal depression was more prevalent compared to the mild to moderate and moderate to severe depression.
Male to Female Ratio
This research revealed that depression is more common in females (58%) than in males (42%) with a male-female ratio of 1:1.4 for the average severity scores. A study published by the Children’s Hospital of Pittsburg also demonstrated similar results with the female adolescent population (36%) being more affected than the male adolescent population (14%).16 In similar research reported by PEW Research Center, depression affected females (74%) more than males (26%).17 Likewise, Thapar and colleagues found that depression increases sharply in girls more than in boys.7 Therefore, the data from this research is consistent with previous studies and it is evident that depression affects female adolescents more than their male counterparts.
Age Group
As age increases, depression increases for both male and female adolescents.9 This was confirmed as shown in Figure 3. Average severity scores were observed to be increasing with increasing age, but it must be noted that even at higher age groups, the average severity scores did not exceed 4. This indicates that considering depression by age group, the older adolescents did not display symptoms beyond mild depression. The 16-18 age group was determined to be affected more by depression than the 10-12 and 13-15 age groups.
Major Factors Contributing to Depression
Figure 4 shows that of the 11 factors investigated, 4 were the major contributors to minimal adolescent depression as shown by the higher average severity scores of more than 3.0. These 4 factors were: the presence of both parents in the home, the number of occupants, the family type and family history of depression.
From this research, it was found that the average severity score for both parents present in the home was 3.04, while it was 3.50 for the absence of one parent. The absence of one parent essentially reflects a single Parent type family and this type of household home puts significant strain on the single parent that is present.18 This therefore puts a significant strain in the mental and even physical development of adolescents in the home due to lack of support and resulting in an increased risk for adolescent depression.19
Similarly, the type of family present and number of occupants in the home affects depression, that is, a single parent compared to a nuclear or extended family, and less occupants compared to more occupants in the home. Literature shows that depression increases with the order of nuclear family, joint-physical custody followed by single parent family.20 In addition, adolescent depression decreases with more persons being present in the home through an extended family. This can be attributed to the level of support from family members to improve adolescent self-esteem and overall decrease of depression.21 Data gathered from this research showed average severity scores of 2.4 for nuclear and 4.2 for single parent households, indicating relatively more depression was present in the single parent homes compared to nuclear families. For the number of occupants in the home, data showed that with 3 to 5 persons being present, average severity scores decreased from an average of 3.8 to 2.2.
The other major factor that contributed to depression in this research was a family history of depression (maternal or paternal) and the average severity score was determined to be 3.2. This factor has always know to be of great influence in Adolescent Depression. Having a parent who has suffered from Depression increases the risk three to four times higher for adolescent depression.7 The risks also greater with history of multiple previous generation depression. Thus, it is important to always include a Family Mental History when screening adolescents.22
Conclusion:
The findings of this study have indicated that of a total of 89 students, 88.8% had zero to minimum depression while 9.0 and 2.2% presented with mild to moderate, and moderate to severe depression respectively. No student was found to be severely depressed. The 2 students (2.2%) that were found to be mild to moderately depressed was determined to be not statistically significant based on the p-value determined. The results also showed that, consistent with the literature, female students were found to be more affected by depression than their male counterparts with a male to female ratio of 1:1.4 for the average severity scores. In addition, it was determined that with an increase in age, the risk of depression also increased. Specifically, the 16-18 age group was determined to be more affected than the 10-12 and 13-15 age groups. Furthermore, from the 11 factors investigated for adolescent depression, the presence of both parents in the home, the number of occupants, the family type and family history of depression were the 4 factors that highly contributed to adolescent depression. The nuclear family presented lower levels of depression than the single parent family while the presence of less occupants in a household increases the risk of depression. A family history of depression also increases the risk of adolescent depression. Overall, as evident in the findings, adolescent depression at the St Cuthbert’s Mission Secondary school was as a result of a multiple risk factors.
Limitations:
Recommendations: