Clinical Psychology and Mental Health Care
OPEN ACCESS | Volume 7 - Issue 1 - 2025
ISSN No: 2994-0184 | Journal DOI: 10.61148/2994-0184/CPMHC
Daniel Tuinstra, MD; Brian Nixon*, MD; Jessica O’Mara, MD.
Pine Rest Christian Mental Health Services and Michigan State University College of Human Medicine Psychiatry Residency and Fellowships Program.
*Corresponding Author: Brian Nixon, Pine Rest Christian Mental Health Services and Michigan State University College of Human Medicine Psychiatry Residency and Fellowships Program.
Received Date: April 04, 2022
Accepted Date: April 18, 2022
Published Date: April 22, 2022
Citation: Daniel Tuinstra, Brian Nixon, Jessica O’Mara (2022). “Electroconvulsive Therapy for Refractory Neuropsychiatric “Long Covid-19” Symptoms: Two case Reports.” Clinical Psychology and Mental Health Care, 4(2); DOI: http;//doi.org/01.2022/1.10064.
Copyright: © 2022 Brian Nixon. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
,
Background:
The SARS-COV-2 pandemic (COVID-19) began impacting the United States heavily in March, 2020 and was affecting the Wuhan province of China well before that. More than 44.3 million cases have been reported in the United States (Ritche H. et al. 2021). Approximately 10 percent of cases may develop so-called “Long-COVID” defined by some as extending beyond three weeks of first onset of symptoms (Greenhalgh T., et al., 2020). Symptoms of COVID-19 infection can include neuropsychiatric symptoms (Taquet M., et al., 2021) such as anxiety, depression, somatization, and psychoticism in all stages of recovery (Xie, Q., et al., 2021) up to eight months or more with social and occupational impairment (Havervall S., et al., 2021) even in mild cases of COVID-19. Roughly 23 percent of these patients reported concerns of depression or anxiety (Huang C., et al., 2021). Clinical researchers are still only beginning to analyze neuropsychiatric symptoms and treatment data while the pandemic continues to rage given new mutations of the SARS-COV-2 virus. There is minimal data available for ECT treatment for severe refractory psychosis, depression, or anxiety symptoms associated with COVID-19. To the best of our knowledge we are one of the few to report the possible benefits of ECT for patients with COVID-19.
Summary:
We present two cases of robust response to acute series electroconvulsive therapy (ECT) for two hospitalized females with COVID-19 related treatment resistant neuropsychiatric symptoms of severe psychosis, depression, and anxiety. Case #1, a 62-year-old female with no psychiatric history demonstrated remission of psychotic depression and severe anxiety symptoms secondary to COVID-19 after 10 acute series ECT treatments. Case #2, a 65-year- old female with no psychiatric history also presented with remarkably similar delusional content, psychotic depression, and severe anxiety that remitted after seven acute series ECT treatments. There are few other such published reports and offer these examples as some evidence for possible inclusion of ECT for treatment of COVID-19 related treatment resistant neuropsychiatric symptoms.
Case #1:
Case #1 was a 62-year-old married, recently unemployed, white, cis-gender, heterosexual, able-bodied female with psychiatric history of recurrent moderate depression treated with escitalopram 15 mg daily after October 2020 when she also contracted COVID-19. Her past medical history was otherwise significant for primary hypertension treated with clonidine 0.1mg twice daily and lisinopril 20 mg daily, GERD treated with omeprazole 20 mg daily, seasonal allergic rhinitis treated with fluticasone propionate intranasal spray, and uses hearing aids. She required hospitalization for COVID-19 infection, hyponatremia, and urinary tract infection. She had an abrupt severe depressive episode at this time, crying “60% of the day” and expressing to her husband that she did not want to live. She required nine subsequent inpatient hospitalizations at various clinical and academic treatment centers between October 2020 and May 2021. During this time, she presented with delirium multiple times, hospital stays ranged from 3 days to 5 weeks in duration, and she was tried on multiple psychotropic medications with no perceived benefit. Aside from depression in her brother and mother, there was no other significant family health history and no surgical history. The patient and her husband were poor historians and medical records from outside hospitals were incomplete.
She was also being seen by a private practice outpatient psychiatrist and an outpatient neurology service for 3 weeks prior to the 10th inpatient psychiatric hospitalization for ongoing provisional diagnosis of Major Depressive Disorder, recurrent, severe, with anxious distress and psychotic features due to COVID-19 infection. Her outpatient neurologist ruled out organic causes of the patient’s signs and symptoms prior to the admission. Computed Tomography (CT) scan of the brain months earlier showed general parenchymal loss but without any acute or abnormal processes. A brain MRI was scheduled for four days after the 10th psychiatric admission but was unable to be completed.
The patient and her husband were seeking inpatient psychiatric treatment two days prior to her tenth admission at another institution due to severe impairment in her ability to work at her co-owned industrial shop. She had been experiencing severe and persistent low mood, extreme tearfulness “over 60% of each day”, with severe initial insomnia without use of psychotropic medications, severe inattention, anergia, and anhedonia. She was denying thoughts of suicide at the time of admission. During the initial interview the patient was continuously pacing and wringing her hands and crying loudly. She expressed paranoia and believed that unknown people were coming into her home and moving things around. Paranoia began after initial medical hospitalization for COVID-19 infection when her purse was removed from her possession by a nurse. The patient believed that the nurse in question, along with other hospital staff, would obtain all of her account information and stole her family’s money from their business and personal accounts. She believed this left her husband and children financially ruined. She could not be reassured by her husband who gave her evidence that their bank accounts remained unharmed. She felt the hospital staff in question had discovered a way to hide their theft and was convinced that her family would be destitute. As a result of this belief she felt overwhelmed with guilt and thought she would be better off dead. She did not feel any subjective improvement on her home medications despite adherence to Quetiapine 400 mg twice daily, escitalopram 15 mg daily, trazodone 25 mg nightly, and lorazepam 1 mg twice daily and 0.5 mg nightly. Lorazepam was reportedly recently decreased from 1 mg three times daily with no apparent change in symptoms.
At time of her tenth admission the patient was visibly shaking with severely anxious affect, tearful, loudly weeping, perseverating on her paranoid and nihilistic delusional beliefs. She was unable to sit through the interview due to the severity of restlessness. She was unable to sleep or eat appropriately. Case # 1 was guarded about paranoid beliefs. Her husband of 45 years was able to provide crucial collateral information and he stated that the patient had no known trauma history or psychiatric symptoms prior to October 2020 when the patient contracted SARS-CoV-2. Importantly, over two weeks prior to the hospitalization the patient was reported to have used edible THC-containing gummies to help with anxiety, insomnia, and anorexia equivalent to “50 mg of cannabis daily” per the husband’s report. Her last use was two days prior to psychiatric hospitalization. The product used could not be verified due to geographic constraints and ongoing COVID-19 related visitor policy restrictions. There were no other substance use concerns and no concerns for sexually transmitted infections. Physical exam was otherwise non-contributory. Admission labs were significant for elevated leukocyte esterase in urine analysis, elevated alkaline phosphatase (126), and urine drug screen positive for THC. CBC with differential, CMP, COVID-19 PCR, TSH, A1c, and lipid panel were otherwise within normal limits. Her vital signs were within normal limits at admission. Her memory and orientation were intact. She was limited in her mental status exam participation due to severe anxiety and distress. The patient’s admitting diagnosis was Major Depressive Disorder, Recurrent, Severe, with psychotic features and anxious features and Cannabis Use Disorder, Moderate. Other contributing factors considered included neuropsychiatric sequelae from COVID-19 infection, possible side effects such as delirium from her current psychiatric medications, and substance-induced depression and anxiety symptoms from cannabis. The possibility of a new or unrecognized neurocognitive disorder was also considered. The patient’s lorazepam was increased initially to 1 mg three times daily due to the severe distress of her anxiety. Her home medications were otherwise continued at the time of admission.
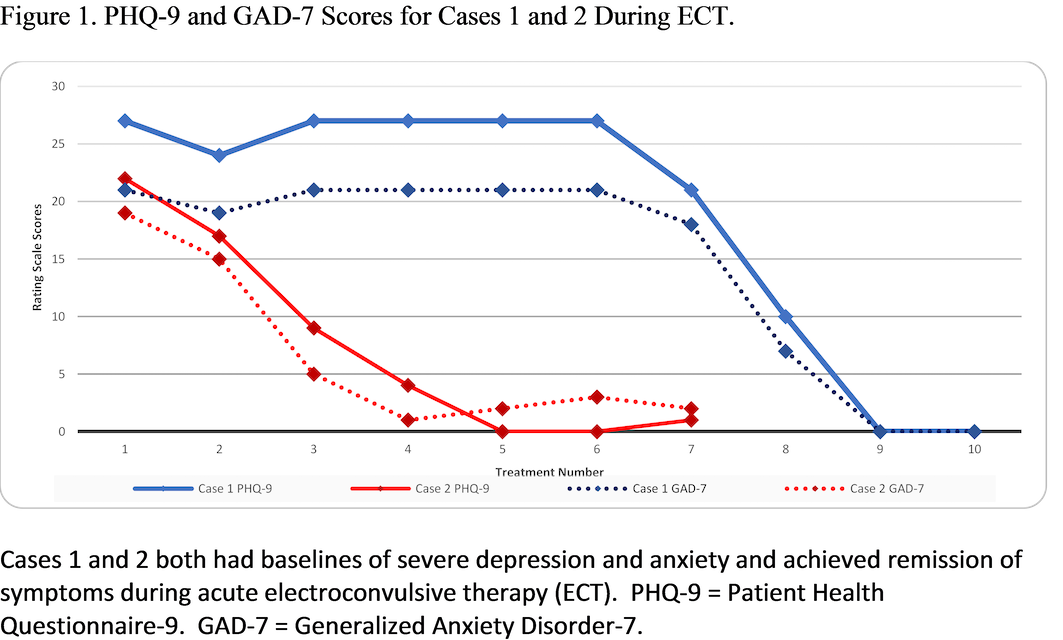
On hospital day 18 of the tenth admission the patient was cleared for electroconvulsive therapy (ECT) following failure of trials on mirtazapine, Quetiapine, escitalopram, haloperidol, risperidone, trazodone, citalopram, clonazepam, lorazepam, propranolol, and olanzapine without benefit. Her Patient Health Questionnaire-9 (PHQ-9) score was 27 and Generalized Anxiety Disorder-7 (GAD-7) score was 21 (see Table 1). She continued to present with poor appetite, insomnia, decreased ability to perform activities of daily living (ADLs), with ongoing severe depression, anxiety, delusional thought content, and suicidal ideation. The patient was closely monitored with staff support for orientation, regular sleep/wake cycle, medication administration, assistance with ADLs, serial cognitive assessments, and any non-essential medications were eliminated to minimize possible delirium contribution. After each of initial four bilateral ECT treatments administered three times weekly, the patient demonstrated marked improvement in affect, perseveration, mood, anxiety, ADLs, sleep, appetite, communication, and suicidal ideation. She continued to hold delusional beliefs although less tenaciously and with much less distress. She experienced transient anterograde amnesia that resolved typically within two hours. Right unilateral ECT treatment was administered at the fifth session due to the patient’s confusion. She was switched back to bilateral for the sixth and seventh treatment due to concerns for efficacy. After the seventh bilateral ECT treatment she demonstrated more pronounced confusion. Treatment eight was delayed two days and the patient demonstrated significant improvement in confusion side effects. Treatments eight through 10 were completed using right sided ECT treatment only. See Table 1 for additional ECT information related to this case. Delusional paranoid and nihilistic beliefs resolved. Severe depression, anxiety, and suicidal ideation symptoms achieved remission based on serial verbal numeric rating scales, clinical observations, and collateral information from family during the tenth hospitalization.
Case # 1’s PHQ-9 score was zero and her GAD-7 score was zero at the ninth ECT treatment. She was discharged home on hospital day 43 with outpatient psychiatric care. She continued escitalopram 30 mg daily and olanzapine 10 mg twice daily which had remained stable during the final 25 days of her psychiatric hospitalization. A three-month follow-up phone call showed the patient to have progressive return of anxiety symptoms without delusional conviction or depression and was considering maintenance ECT treatments which were not initially planned due to geographic limitations.
 Case #2:
Case #2:
Case #2 was a 65-year-old married, retired administrative assistant, Caucasian female with no formally diagnosed psychiatric history prior to contracting COVID-19 in May, 2021.
Symptoms were mild and managed at home. Medical history was significant for paroxysmal atrial fibrillation and recurrent urinary tract infections (UTIs), which had recently been well managed using cranberry supplements. She first noticed mild worsening of mood and difficulty sleeping following a hysterectomy in January 2021; however, symptoms were not significantly distressing until after she contracted COVID-19 in May 2021. She began to experience significant anxiety, rapid deterioration of sleep, averaging 0-3 hours per night with associated nightmares often waking in a panic due to various concerns. She saw her primary care physician (PCP) one month later where she was diagnosed with Generalized Anxiety Disorder and initiated on buspirone 5 mg daily and as needed trazodone 25 mg nightly. She was seen in the emergency department a few days later for musculoskeletal chest pain and subsequently prescribed gabapentin for persistent jaw pain following dental surgery in December 2020.
Gabapentin was rapidly discontinued for perceived side effects of insomnia and paresthesia. Her PCP discontinued buspirone and trazodone due to no perceived improvement and recommended Lexapro which the patient declined due to concerns for side effects. She consented to starting as needed hydroxyzine 25 mg up to three times daily. The patient returned several weeks later noting no improvement in mood symptoms or insomnia and new concerns for distal bilateral paresthesia of extremities and dysuria. She was concerned for Guillain-Barre as a side effect of hydroxyzine and requested a change in anxiety medication. She was started on citalopram 20 mg daily and as needed hydroxyzine 25 mg nightly. The patient discontinued hydroxyzine approximately two weeks later due to patient being concerned for potential interactions between hydroxyzine and citalopram, but without physical concerns at that time. Follow-up for neuropathy resulted in unclear etiology of symptoms with the following labs: unremarkable connective tissue disease antibodies, CBC, globulin, protein electrophoresis, CMP (except for Na of 128), Vitamin B12 of 296, and positive ANA. Patient was advised to follow-up with her PCP. She endorsed mild improvement of mood since starting citalopram by the end of July 2021. Three days later the patient’s husband of 15 years contacted the PCP reporting increased episodes of confusion, depression, aggression, and paranoia over the last several weeks and requested a full psychiatric evaluation. Patient was medically cleared and referred to a local psychiatric urgent care center for evaluation and was ultimately admitted voluntarily to an older adult psychiatric hospital floor.
Upon admission she endorsed several weeks of worsening sleep disturbance, “night terrors”, anxiety, and new onset delusions that she and her husband were the victims of identity theft. She related that these delusional thoughts began after a phone conversation with someone she feels was a telemarketer who was then using her voice to steal her identity.
Concerned about this possible identity theft, she visited an “unsafe website” to freeze their accounts, which she felt made things worse. She feared that someone hacked into her phone and computer and was listening to her conversations. She endorsed auditory hallucinations involving “hearing a clicking sound” while on phone calls. She was resistant to reassurance from her husband and experienced significant guilt, depression, and anxiety surrounding these delusions. She reported losing 20 lbs after hysterectomy and another 20 lbs since COVID infection in May 2021 due to poor appetite. During the initial interview the patient was partially cooperative but tearful, restless, “scared”, hypervigilant and paranoid. There was no concern for substance use. The patient reported a significant history of physical and emotional abuse during her childhood. The patient’s husband was able to provide critical collateral information of no prior psychiatric history, being “fully functional with stable cheerful mood” prior to her recent COVID-19 infection. She completed an extensive lab workup including ferritin and B12, all of which were unremarkable. Patient also initially endorsed UTI symptoms, but UA was negative and symptoms resolved spontaneously. The admitting diagnosis was psychotic disorder due to a medical condition (COVID-19) with delusions and unspecified anxiety. Treatment team continued Citalopram 20 mg per day and started as needed hydroxyzine 25 mg and melatonin 9 mg nightly. Hydroxyzine and melatonin were rapidly discontinued due to reported side effects. Quetiapine 12.5 mg nightly was then added for insomnia and paranoia. Her paranoid and nihilistic delusions responded well to quetiapine titration, but she admitted to an aborted suicide attempt the week prior, during the hospitalization that was previously unknown to staff. She reported guilt and remorse about suicide attempt and feared that she had “ruined everything” and was “letting her husband down”, despite repeated reassurance by medical team and husband that this was not the case. She demonstrated remission of presenting symptoms and was discharged after 13 days.
She described the two days after discharge as “awesome” with a “good” mood with no anxiety or delusional thoughts. She noted overwhelming anticipatory anxiety when disclosing her previous suicide attempt to her husband. She stated, “I was feeling closed in," and delusional/paranoid thoughts returned that her/her husband's identity had been stolen after reading an insurance statement and not recognizing some charges. Auditory hallucinations of "clicking noises" on the phone returned. She stated that it quickly felt like “everything was back to where it was before I came last time.” The patient informed her husband about her recent suicide attempt because she did not want him to misunderstand current symptoms and reported that he was very supportive. The next day, family convinced her to return to the ED and was admitted a second time to the inpatient psychiatric hospital older adult unit. At admission, she was in obvious distress, tremulous, perseverating on feeling “like a failure, letting everyone down,” and somatic delusions fearing that she had inflicted permanent damage to her body during previous suicide attempt despite reassurance from medical staff. She endorsed thoughts of “being better off gone or dead.”
During the second hospitalization she experienced persistent insomnia, severe anxiety, depressed mood with significant guilt, and nihilistic, delusional thoughts. Quetiapine was titrated to 250 mg nightly and 50 mg three times daily with meals. Citalopram was titrated to 40 mg daily. Serum B12 was subclinical, 296 pg/mL, and supplemented with minimal improvement of sleep, mood symptoms, delusional thoughts. Her delusions evolved to incorporate staff. She had persistent passive suicidal ideation. Due to persistent, severe symptoms and resistance to treatment efforts, electroconvulsive therapy (ECT) was offered but she declined due to low confidence in the effectiveness and fear of potential side effects. The patient disclosed that she had a second aborted suicide attempt during the second hospitalization and felt “ashamed”.
She was transferred to the close observation area (COA) with room lockout and family was contacted to discuss options. After additional education and discussion with family she consented to an acute series of ECT (see Table 2).
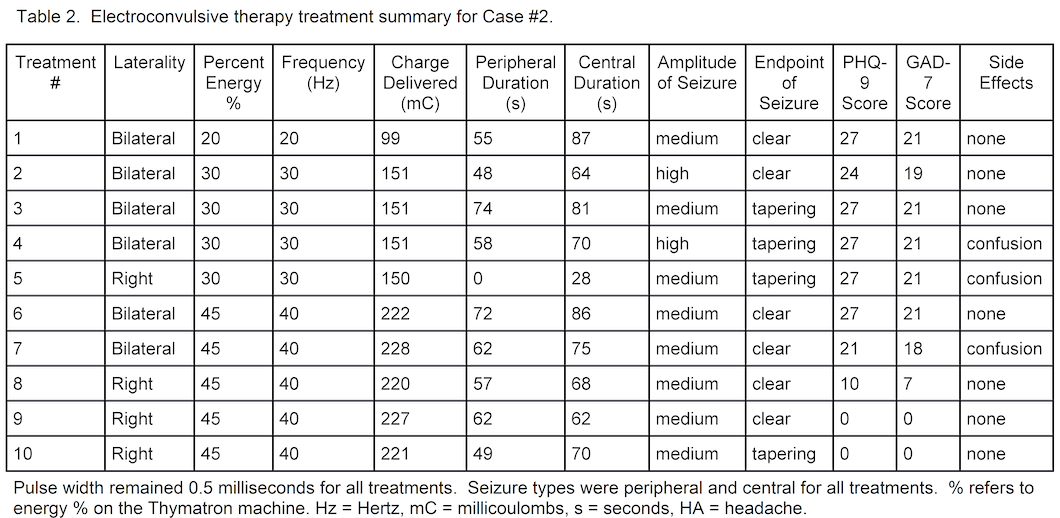
The patient’s Patient Health Questionnaire-9 (PHQ-9) score was 22 and Generalized Anxiety Disorder-7 (GAD-7) score was 19 at time of her first ECT treatment. She was concerned that ECT may lead to personality changes, memory deficits, and continued to demonstrate nihilistic and delusional beliefs about nursing having a hard time finding a vein for IV access because of her suicide attempt. After a long holiday weekend the patient then received the next two treatments (second and third treatments) on consecutive days. She tolerated procedures well and was subjectively less anxious, less paranoid, and had an improved mood. PHQ-9 and GAD-7 improved to nine and five, respectively. The patient denied suicidal thoughts and stated “I have a lot of reasons to live.” Following the third treatment, she reported transient recent recall difficulty. The following day she was markedly more paranoid including beliefs that ECT clinic staff was poisoning her through her IV. Prior to the fourth ECT treatment, PHQ-9 and GAD-7 scores were four and one, respectively. She was much less delusional, denying any recollection of thoughts about her IV line being poisoned or her identity being stolen, denying hallucinations, and denying suicidal thoughts. Her PHQ-9 and GAD-7 scores were zero and two, respectively, prior to the fifth ECT treatment. However, the patient became disoriented to time, missing the current year by 26 years in the past. Her PHQ-9 and GAD-7 scores were zero and three before the sixth ECT treatment. She continued to demonstrate remission of psychiatric symptoms and good tolerability to ECT and her medication regimen (as above). Throughout acute series ECT, no medication changes were made. A seventh and final acute series ECT treatment was completed and outpatient maintenance ECT was planned at discharge. A two-week follow-up call to the patient showed ongoing remission of all psychiatric symptoms.
Discussion:
The etiology of neuropsychiatric symptoms related to COVID-19 infections is not well understood. The possible pathogenic mechanisms could include extrapolation from other corona viruses. Banerjee and Viswanath ‘s (2020) review describes possible etiologies including direct injury through blood circulation compromise resulting from an exaggerated immune response; direct neuronal injury; hypoxic injury secondary to pulmonary compromise cerebral edema or increased intracranial pressure; dysregulated immunomodulation; immune cell transmigration to the central nervous system; ACE-2 and CoV spike protein interaction; autoimmunity, or other means. Additionally, there is evidence that coronavirus related neuropsychiatric effects could make chronic psychiatric conditions worse. Neuropsychiatric symptoms associated with COVID-19 can endure and are impacted by severity of the illness and are associated with dementia, mood and anxiety disorders (decreasing after 6 months), and psychotic disorders at six months from infection (Taquet et al., 2021). These authors also importantly note that there may be social and psychological factors related to the infection that may impact common psychiatric symptoms such as mood and anxiety disorders.
In these two cases we see a rapid remission of COVID-19 related severe neuropsychiatric symptoms after only four to nine acute series, predominantly bilateral ECT treaments. Overall the treatments were well tolerated with minimal temporary confusion similar to well known side effects of ECT used for established clinical indications. ECT treatment was effective after one patient required nine previous inpatient psychiatric hospitalizations and in both cases after multiple failed pharmacologic interventions including augmentation and antidepressants with antipsychotic medications. Both cases presented were women of relatively advanced age with similar presentations of severe anxiety and depression with psychotic features. Treatment of COVID-19 related neuropsychiatric presentations that differ from the cases described above may not benefit in the same manner. We do not know the long- term effects of ECT for COVID-19 neuropsychiatric symptoms or the role of maintenance ECT for these cases. Caution must be used in using ECT, as for any patient receiveing this treatment, to screen for contraindicated medical comorbidities or medications that may interfere with the optimal seizure activity or associated anesthesia. In the absence of signficiant response or remission of COVID-19 related severe neuropsychiatric symptoms using multiple pharmacologic intervention strategies, ECT may be an important tool for treateing refractory sytmpoms as in the cases described above.
Treatment for neuropsychiatric symptoms of “long COVID” is not well understood at this time and there is no consensus though some treatments have been suggested for delirium associated with COVID-19 (Baller et al., 2020) but encourages caution with ECT in this context. Psychiatrists should work to be actively engaged in coordination of COVID-19 infection care.
Psychiatric consults in one study included 25.5% of hospitalized COVID-19 patients (Yue, L., et al., 2020) for concerns related to (in decreasing frequency) sleep, anxiety, depression and delirium. The vast majority were new-onset mental health concerns. Psychiatric care coordination was especially important in critically ill patients and interventions included supportive therapy, anxiolytics (including benzodiazepines), antidepressants, and antipsychotics. Of note, there were some interesting commonalities in the delusional themes of these two patients including financial ruin and identity theft which may warrant further exploration. These cases highlight the need for further investigation into the role of ECT for refractory neuropsychiatric symptoms of “Long COVID”.