Clinical Psychology and Mental Health Care
OPEN ACCESS | Volume 7 - Issue 1 - 2025
ISSN No: 2994-0184 | Journal DOI: 10.61148/2994-0184/CPMHC
Hani Raoul Khouzam1,2* and Sarah Jackson3
1Staff Psychiatrist, PTSD Treatment Program, VA Northern California Health Care System (VANCHCS), Mather, California.
2Clinical Professor of Psychiatry and Medicine, UC Davis Health, Sacramento, California.
3Clinical Psychologist, PTSD Clinical Team, Mental Health Care Line, Michael E. DeBakey VA Medical Center, Houston, Texas.
*Corresponding Author: Hani Raoul Khouzam, VA Northern California Health Care System, Sacramento VA Medical Center 10535 Hospital Way, Bldg. 649, Mather, CA 95827-4200
Received: December 15, 2021
Accepted: January 14, 2022
Published: January 18, 2022
Citation: Hani Raoul Khouzam and Sarah Jackson. “Orexin Receptor Antagonists: Alternative Treatment of Primary Insomnia”. Clinical Psychology and Mental Health Care, 1(5); DOI: http;//doi.org/01.2022/1.10060.
Copyright: © 2022 Hani Raoul Khouzam. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
Pharmacological agents currently available for the treatment of primary insomnia have demonstrated limited long-term efficacy and problematic side effects. The purpose of this review is to highlight the concerns surrounding the most widely used medications that are used for the management of primary insomnia, and to summarize the mechanism of action and beneficial effects of the orexin receptor antagonists suvorexant, and lemborexant as alternative therapeutic interventions for the management of primary insomnia.
Introduction
Insomnia is most widely defined as a state of a recurrent difficulty initiating sleep, staying asleep and /or early awakening with inability to resume sleep. In primary insomnia sleep difficulties are not related to underlying medical conditions, or other sleep-wake disorders, are not adequately explained by an underlying psychological condition, and persist despite the adequate opportunity and circumstances for sleep. It is estimated that about one-third of the adult population experiences symptoms of insomnia, with 10%-15% reporting daytime impairments in important areas of functioning [1]. It is estimated that between 6% and 10% of individuals with sleep difficulties would meet core criteria for primary insomnia disorder, making it the most common sleep disorder among sleep-wake disorders [2]. Insomnia as a disorder is quite different from a brief period of poor sleep, with far-reaching consequences to both physical and mental health. It is a persistent condition with a negative impact on many aspects of daily life, and could seriously affect interpersonal, vocational, academic, and social functioning.
Non-Pharmacological Approach
The goal of treating insomnia is to improve sleep quality and quantity, as well as daytime functioning, while avoiding adverse events and next-morning residual effects. The prevalence of insomnia is considerably higher in patients with chronic medical disorders and comorbid psychiatric conditions, especially mood, anxiety, substance use, and stress-and trauma-related disorders. General clinical guidelines including those of the American Academy of Sleep Medicine (AASM) clinical guidelines recommend cognitive-behavioral therapy for insomnia (CBT-I) as the most appropriate evidence-based treatment for patients with insomnia [3,4].
CBT-I includes sleep hygiene education, cognitive therapy, relaxation techniques, environment stimulus-control and implementation of sleep-restriction [5]. However, many patients with primary insomnia experience ongoing sleep difficulties despite adherence to the elements of CBT-I, and other patients are simply unable to practice the tenets of CBT-I consistently enough to achieve success; thus, necessitating adjunctive pharmacological interventions [5].
Pharmacological Treatment
The conventional pharmacological treatments of primary insomnia fall into four main categories which include certain benzodiazepines (BZDs), and non-BZDs hypnotics, a low dose of the tricyclic antidepressant (TCA) doxepin, melatonin agonists and other off-label sedating or hypnotic agents [6]. The various medications that are usually prescribed for insomnia treatment and their U.S. Food and Drug Administration (FDA) approved indications are outlined in table 1.
Table1: Medications Usually Prescribed for Insomnia Treatment

The BZDs receptor agonist hypnotics include: clonazepam, diazepam, flurazepam, lorazepam, temazepam, and triazolam ,which promote sleep by enhancing γ-aminobutyric acid (GABA) inhibitory effects [7]. The non-BZDs hypnotics, also known as the “Z”-drugs have 3 compounds that include eszopiclone, zaleplon, and zolpidem with alternate structures but similar mechanisms of action to their benzodiazepine counterparts, by acting on the GABAA receptor [8]. These two classes of medications have generalized central nervous system depressant effects and are associated with problematic adverse events, such as hangover, development of tolerance, addiction, rebound insomnia, muscular atonia, inhibition of respiratory system, and cognitive dysfunction especially in patients with underlying medical conditions and the elderly [9,10]. The abrupt discontinuation of the BZDs is also associated with physical withdrawal symptoms, manifested by increased anxiety, neurological, and cognitive symptoms, as well as the possibility of withdrawal seizures. The exact mechanism of the TCA doxepin on sleep is unknown, but is thought to be related to its histamine H1 receptors antagonism [11]. Doxepin seems to vary in its effects on sleep initiation and maintenance and its use is associated with sedation, somnolence, nausea, and possible upper respiratory tract infections [12]. The melatonin agonists, such as ramelteon [13], and various over the counter melatonin agents induce sleep through activation of melatonin 1 and melatonin 2 receptors in the suprachiasmatic nucleus of the hypothalamus [14,15]. Other off-label medications which have not been approved for the treatment of insomnia (but are used as alternative agents due to their sedating properties) include certain compounds with antihistaminic-like effects, such as diphenhydramine, hydroxyzine and doxylamine. Antidepressants such as trazodone, mirtazapine, amitriptyline and trimipramine [6] are also frequently utilized to leverage these same properties. The long-term efficacy of these off-label medications on insomnia is not well established and their adverse effect profile of sedation, motor incoordination and tolerance are considered undesirable by many patients.
Although these various classes of medications for the treatment of insomnia are widely available and prescribed frequently, they are commonly associated with limited and short-term efficacy and multiple problematic side effects. This has resulted in the need for exploration of alternative agents with greater efficacy and more tolerable side effects such as the orexin receptor antagonists. This review will summarize the mechanism action and the beneficial effects of the orexin receptor antagonists in the management of primary insomnia.
Orexin Receptor Antagonists
The orexin neuropeptides were discovered in 1998 and found to be produced by a small group of hypothalamic neurons whose actions are mediated by two receptors subtypes, (orexin-A (OXA) and orexin B (OXB), also known as hypocretin-1 and hypocretin -2 or OX1R and OX2R [16,17]. They are located in the lateral, dorsomedial and peripheral lateral hypothalamus, as illustrated in figure 1.
Figure 1: Orexin Neurons Location
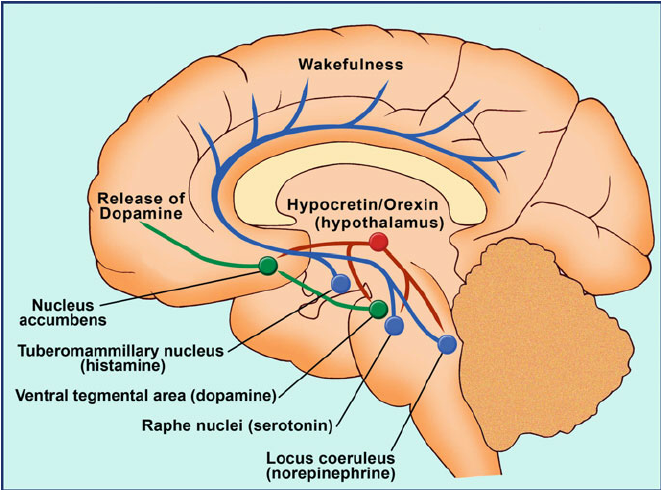
Despite being highly localized, approximately 70,000 orexin neurons project widely throughout the brain and spinal cord, sending signals through the brainstem, cortical, and limbic regions, which activate the cholinergic and monoaminergic neural pathways of the ascending arousal system [12]. Their diffuse pattern of distribution correlates with their wide variety of functions in regulating appetite, metabolism, the reward system, stress, autonomic functions; and the most salient to this review, being the transition between wakefulness and sleep. The role of the orexinergic neurons in regulating the sleep-wake cycle led to the development of the orexin receptor antagonists as a new class of pharmacological agents for the treatment of insomnia. There are three orexin receptor antagonists: suvorexant, lemborexant and daridorexant. Suvorexant (Belsomra ®) was approved by the FDA in 2014 [18], lemborexant (Dayvigo®) was approved by the FDA in 2019 for the treatment of insomnia [19] and on March 10, 2021, the FDA accepted daridorexant’s application for review.
Suvorexant
Mechanism of Action
Suvorexant is a dual orexin receptor agonist (DORA) that bind respectively to both OX1R and OX2R receptors and inhibit the activation of the arousal system, thus, facilitating sleep induction and maintenance, and thereby inactivating wakefulness [20].
Pharmacokinetics
Suvorexant is available as an immediate-release tablet with pharmacokinetic properties that potentiate onset and maintenance [21]. It is primarily metabolized through the cytochrome P450 (CYP) 3A pathway, with limited contribution by CYP2C19, it has no active metabolites, and its blood level and risk of side effects is higher with the concomitant use of CYP3A inhibitors [22]. It should not be administered with other strong CYP3A inhibitors; the initial dosage should be reduced with moderate CYP3A inhibitors [21,22]. Concomitant use of strong CYP3A inducers can result in a low suvorexant level and reduced efficacy [21,23]. The elimination half-life of suvorexant is approximately 12 hours, reaching a steady state in approximately 3 days [21]. Due to its moderately long half-life, it could be associated with residual morning sleepiness and somnolence which could impair daily functioning; however, this impairment could be minimized by using the lower dosage and by not exceeding the recommended dose [24].
The recommended starting dose of suvorexant is 10 mg within 30 minutes of initiating sleep and of at least 7 hours remaining before awakening time. If the 10 mg dose is well tolerated, the dose may be increased to a maximum of 20 mg if needed for sleep induction [25]. Elimination is approximately two-thirds through feces and one-third in the urine [16]. Suvorexant metabolism differs in males and females and can be affected by the body mass index. Females and overweight individuals a lower dosage [21-26].
Adverse Effects
Compared to those receiving placebo, patients receiving suvorexant were more likely to report fatigue, abnormal dreams, dry mouth, daytime sleepiness, and somnolence [27]. Impaired driving, suicidal ideation, sleep paralysis, hypnagogic/hypnopompic hallucinations, and cataplexy-like symptoms, although rare can still occur in some patients [29].
Contraindication
Suvorexant is contraindicated in patients with narcolepsy [29]. Although suvorexant was not evaluated in patients with narcolepsy, it might precipitate a spectrum of symptoms in patients with narcolepsy such as excessive sleepiness, cataplexy, hypnagogic hallucinations, and sleep paralysis.
Clinical Considerations
The FDA categorized suvorexant as a Schedule IV controlled substance. Although there is no evidence of physiological dependence or withdrawal symptoms with suvorexant, it could carry a low risk for misuse and abuse potential [30].
There are no specific guidelines about the duration of treatment with suvorexant use, and it has not been associated withdrawal symptoms upon its when discontinuation. Clinicians prescribing it for the maintenance treatment of insomnia need to inform their patients about its residual daytime sedation and somnolence and its potential for impairing impair driving or other activities that require full mental alertness, especially when prescribed the 20-mg dosage.
Lemborexant
Mechanism of Action
Lemborexant is a dual orexin receptor agonist (DORA) that exerts its effects by reversible competitive binding to, and thus inhibiting, the wakefulness effects of orexin on OX1R and OX2R receptors, with a stronger affinity for OX2R [31].
Pharmacokinetics
Lemborexant is available in immediate-release tablets with a peak concentration time of approximately 1 to 3 hours after ingestion. Its intake following a high-fat and high-calorie meal, could delay its absorption and decrease its plasma concentration [19]. The elimination half-life of Lemborexant is 17 to 19 hours, it is excreted in feces (57%) and to a lesser extent urine (29%) and it is primarily metabolized through the cytochrome P450 (CYP) 3A4 pathway, and to a lesser extent through CYP3A5 [32]. Concomitant use with moderate or strong CYP3A inhibitors or inducers should be avoided, while use with weak CYP3A inhibitors should be limited to the 5-mg dose of Lemborexant [33]. The use of Lemborexant with alcohol could lead to increased impairment in postural stability and memory, due to the direct effects of alcohol in addition to alcohol effects on increasing Lemborexant levels and as such patients receiving Lemborexant are encouraged to void alcohol use [34]. Lemborexant Is administered orally in doses of either 5 mg or 10 mg immediately before bedtime and of at least 7 hours remaining before awakening time to prevent impairment in alertness upon awaking. The maximum recommended clinical dose of Lemborexant should not exceed 10 mg [35].
Adverse Effects
The most common adverse effects are somnolence or fatigue. Headache, nightmares, or abnormal dreams also could occur [19,36].
Contraindication
Narcolepsy is the only contraindication to the use of Lemborexant [19]. Narcolepsy is associated with a decrease in the orexin-producing neurons in the hypothalamus, presumably causing the excessive sleepiness, sleep paralysis, hypnagogic hallucinations, and cataplexy characteristic of the disorder. Hypothetically, an orexin antagonist medication could exacerbate these symptoms [19,36].
Clinical Considerations
Lemborexant is classified as a Schedule IV controlled substances and has a low potential for abuse and dependence [34]. Possible impairment in alertness and motor coordination, especially with the 10-mg dose, could affect may affect next-morning driving especially in sensitive individuals [35] Caution is also advised with doses above 5 mg in patients age 65 and older due to possible increased somnolence and a higher risk of falls [19].
Daridorexant
At the time of writing this review, the FDA had accepted the new drug application (NDA) for review of the investigational dual orexin receptor antagonist, daridorexant, for the treatment of adult patients with insomnia.
In clinical trials daridorexant seems to be well tolerated with a favorable safety profile in adult and elderly patients. Its reported adverse effects included headache, somnolence, fatigue, dizziness, and nausea [37]. There was no excess of morning sleepiness, as assessed by the morning visual analogue scale (VAS), even at 50 mg [37]. The incidence of somnolence was low and did not increase with daridorexant 50 mg compared to placebo [37]. The incidence of adverse events associated with orexin deficiency in individuals with narcolepsy, was low, with isolated cases of sleep paralysis or hallucinations in the daridorexant treatment groups [37].
Summary
Several nonpharmacologic and pharmacologic interventions are currently available for treatment of the chronic disabling effects of primary insomnia. Among the nonpharmacologic interventions, CBT-I is recommended as first line treatment intervention. Individuals with persistent and chronic primary insomnia may require adjunctive pharmacologic interventions. While agents including benzodiazepines (BZD), and the non-benzodiazepines ‘Z’-drugs, or ramelteon, melatonin, doxepin, and other sedative and hypnotic agents are commonly used to improve sleep, these compounds have consistently demonstrated limited long term efficacy and problematic side effects. The discovery of the orexin signaling pathway and its role in sleep/wake maintenance has led to the development of the orexin antagonist agents such as suvorexant and Lemborexant. This review summarized the mechanism of action and the beneficial effects of these new therapeutic agents. Orexin antagonists have demonstrated promise as alternative treatment modality for the management of chronic primary insomnia in those individuals who have not responded to the various conventional nonpharmacologic and pharmacologic treatment interventions. Additional studies are needed to evaluate the efficacy of combining the newly available orexin antagonists with nonpharmacologic treatments, particularly in individuals with co-occurring medical and psychiatric conditions.
Acknowledgements
The authors express their thankfulness and gratitude to their family, friends and colleagues for their support and encouragements.
Conflict of interest
The materials described in this article are those of the authors and do not reflect the views of the Department of Veterans Affairs, the VA Northern California Health Care System, UC Davis Health, Sacramento, California, or the Michael E DeBakey VA Medical Center, Houston, Texas. Neither author has any conflicts of interest to report.