Clinical Psychology and Mental Health Care
OPEN ACCESS | Volume 7 - Issue 1 - 2025
ISSN No: 2994-0184 | Journal DOI: 10.61148/2994-0184/CPMHC
Tanvi Goel, Naman Vijaykumar Jain, Dileep Kumar Sharma, Deepali Amol Bansode*
Department of Pharmaceutical Chemistry, Bharati Vidyapeeth (Deemed to be) University, Poona College of Pharmacy, Pune, India.
*Corresponding Author: Deepali Amol Bansode, Associate Professor, Department of Pharmaceutical Chemistry, Bharati Vidyapeeth (Deemed to be), Poona College of Pharmacy, Erandwane, Kothrud, Pune- 411038.
Received: September 13, 2021
Accepted: September 22, 2021
Published: September 24, 2021
Citation: Tanvi Goel, Naman Vijaykumar Jain, Dileep Kumar Sharma, Deepali Amol Bansode. “Focus on Paranoia: Effects, diagnosis, treatment and prognosis”. Clinical Psychology and Mental Health Care, 3(4); DOI: http;//doi.org/03.2021/1.10054.
Copyright: © 2021 Deepali Amol Bansode. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
Paranoia can be defined as an instinct and a process of thoughts of anxiety, fear, threat, suspicion integrated with delusions and irrationality. The classical symptoms include delusions, aggressiveness, suicidal thoughts, secretive. The causes of paranoia cannot be determined clearly but may be because of past traumas, drug-induced, or accompanied with other co-morbid psychotic disorders. The diagnosis and treatment of paranoia are difficult in comparison with other mental disorders. Paranoia is diagnosed in the form of paranoid personality disorder (PPD), paranoid schizophrenia and querulous paranoia. In the present article, varied aspects of paranoia like the social perception and behaviour, drug abuse, suicidality, personality traits, gender dysphoria along with the differences and similarities in male and female paranoic patients, case histories and their clinical features are discussed.
Introduction
Paranoia is the state of intense anxiousness and fearful feelings, including thoughts of severe sufferings, threat and conspiracy. The paranoia is often said to occur with other mental disorders, particularly psychotic disorders [1]. It is one of the central symptoms of psychosis. It mostly leads to a point of delusion and irrationality [2]. Paranoia is diagnosed as paranoid personality disorder (PPD), paranoid schizophrenia and querulous paranoia [3].
P.J. McKenna, the clinical psychologist described paranoia as a disorder whose every aspect including clinical features, boundaries, course are all controversial [4]. On the other hand, Jacques Lacan, a psychoanalyst, delineated psychosis as the prominent category of “functional psychosis” and also differentiated it from schizophrenia, to later mention it as an exemplary form of psychosis [5].
Paranoia is usually associated to be caused by, stress, life events such as insecure attachment, abandons, early life adversity, abuse, trauma, drug induced, psychiatric conditions and mood disorders such as anxiety, phobia, depression, but the exact reason is unlikely to be known on diagnosis [6]. The epidemiological studies of paranoia indicated no signs of categorical distributions and also the underlying causes of paranoia for continuous distribution among population is not completely understood [7].
The present review focuses on the varied effects and case studies of paranoia on gender, drug abuse, personality traits, social behaviour and gender dysphoria (fig 1).
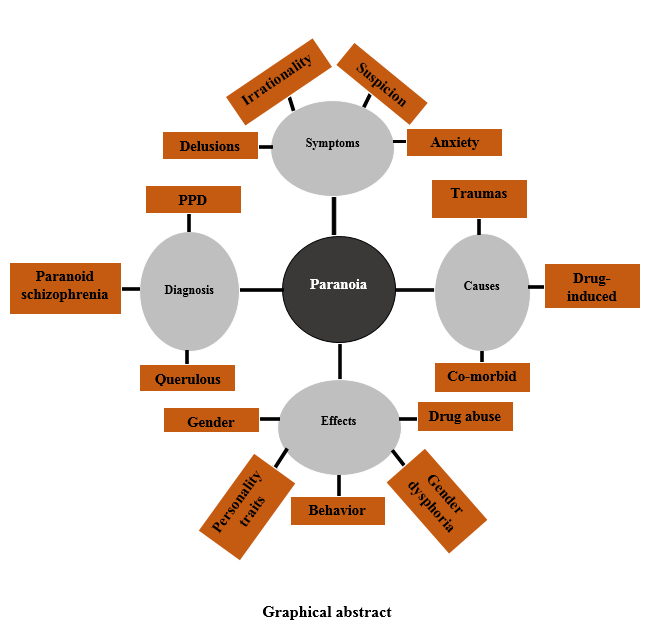

Fig 1: Common mental diseases and their drug of choice.
Paranoia- social perception & behaviour:
Researches on paranoia have suggested social function impairment in patients with high level of paranoia ideation. This interpersonal functioning is attributed to experience of being badly treated by others in clinical samples of patients whereas, negative feelings about others in non-clinical samples of patients [8].
Case vignette
Based on the paranoia scale (PS) two groups of patients were identified as high and low in subclinical paranoia. The patients with high subclinical paranoia showed greater depression, self-consciousness, anxiety and lower self-esteem when compared to the low subclinical paranoia patients. Also, the high subclinical paranoia patients performed worse in laboratory measures of perception and social behaviour [9]. It was then reported that levels of paranoia directly affect the social behaviour and activeness.
Clinically, level of oxytocin can be related with avoidance of social interaction in the paranoid patients. In a study pertaining with Approach-Avoidance task (ATT), reaction time is noted and the tendency to approach or avoid the gaze and happy or angry faces is noted. The basal plasma oxytocin levels of patients under study were measured and it was noted that, patients with higher level of oxytocin tend to avoid the angry faces, and in turn, this avoidance is co-related with the severe psychotic symptoms and the greater paranoia [10].
Paranoia and Suicidality:
Suicidality is a delusional disorder (DD). In the recent literatures it was studied that the suicide rates are more in youth, males, educated subjects, and also the presence of co-morbid psychotic disorders [11]. Paranoia and suicidality are common traits in general population to a varying degree.
Case studies:
Psychopathological corelation of suicide and delusional disorders: An empirical redefinition of delusional disorder and its phenomenology (DELIREMP) study was performed on 89 patients and four psychopathological factors - paranoid, cognitive, schizoid and affective were identified and co-related. These psychopathological factors were compared with the external markers such as diagnosis of comorbid major depressive disorder, delusions, high risk of suicide. The results showed that there was a corelation between these external markers and paranoia [14] and thus was concluded that there is a suicidal tendency in patients of paranoia.
Paranoia and drug abuse:
The literature survey showed that drug-induced paranoia is prominently due to cocaine. Although cocaine can cause various prominent psychotic disorders but inducing of paranoia is very frequent and is known as cocaine-induced paranoia (CIP) [15]. In a study it is concluded that 68% of cocaine users develop transient paranoia episodes gradually [16].
Case study:
A study on homeless subjects who were also high on paranoia revealed that they are most vulnerable to drug abuse, criminal behaviour, aggression and difficulty in controlling their emotions [17]. Thus, it can be concluded that drug abuse and paranoia are inter-related, that is, drug abusers are likely to develop paranoia and the ones suffering from paranoia can easily be tempted towards abusing of substances.
Clinical results of levels of dopamine β-hydroxylase (DβH) protein in plasma and cerebrospinal fluid have shown co-relation with vulnerability to psychotic disorders such as paranoia. It was observed that the levels of DβH proteins in CIP patients was low. DBH locus is responsible for controlling levels of DβH proteins in plasma and cerebrospinal fluid [18].
Paranoia and personality traits:
Paranoia patients are vulnerable in behaviour. They can be aggressive, concerned about body image, anxious, self-doubt. Chances of co-morbidities such as eating disorders, anorexia nervosa is high. Also, the adolescents are more prone to suffer from paranoia [19].
Case study:
A study on paranoia patients based on body image concerns and paranoia was carried out. 35.7% subjects agreed that they feared of being overweight or obese. 12.7% revealed to have felt people making fun of them on their back and 1.1% of subjects believed that there was an unjust plot going on them of which their friends and family did not believe to be true [20]. Although, no clinical evidence of this behaviour has been established, this study paves a way for more exploration of concerns of body image in paranoic patients.
A hypothetical idea suggests the obese or over-weight nature of paranoia subjects may be due to the anti-psychotic medications, psychosocial factors and obesogenic environment [21].
Other personality traits like aggression, dysregulated anger, self-injurious behaviour, criminal behaviour has been observed in patients. The exact reason of these is not clearly known.
Paranoia and gender dysphoria:
A perpetual unhappiness related with one’s own gender is termed as gender identity disorder (GID) or simply gender dysphoria. Usually, patients with gender dysphoria are observed to have paranoia.
Case study:
A research interview by Case Western Reserve University gender identity clinic with 51 male subjects about gender dysphoria revealed that 78% were diagnosed with schizoid and borderline personality disorders like paranoia, 6% were undeniably psychotic, 8% had genital abnormalities and 8% expressed only gender dysphoria. Thus, it can be assumed that that majority of gender dysphoric patients suffer from varied degree of psychotic disorders .
The common observation in the patients who seek sex conversion is that they are uncomfortable with their sexuality and would want to look like the opposite sex. They are also observed to have anxiety, lack familial support and extreme psychological distress [22,23].
Gender differences and similarities:
Paranoia or Paranoid personality disorder is generally more in males when compared to females. Males and females with paranoia are observed to showcase some similar and different traits or even varied level of traits. Some of the differences and similarities are as depicted in (Table 1)
|
Trait |
Male |
Female |
Reference |
|
|
Aggression and impulsive behaviour |
More aggressive and impulsive |
Less aggressive and impulsive |
[24] |
|
|
Suicidality |
Higher risk of suicide |
Lesser risk of suicide |
[25] |
|
|
Dysfunctional detachment |
Negative corelation with paranoid ideation |
Positive corelation with paranoid ideation |
[26] |
|
|
Onset of paranoia (age) |
No difference in onset of paranoia can be reported from the psychiatric consultations. Mean age of onset is 54.13±13.67 years |
[27] |
||
|
Cocaine-induced paranoia |
Men are more likely to suffer from CIP |
Women are less likely |
[28] |
|
|
Gender dysphoria |
Lesser reports of male dysphoria, also men cope more easily with gender dysphoria |
More reports of female dysphoria, women face difficulty for coping up with gender dysphoria |
[29] |
|
Table 1: Gender differences and similarities in paranoic patients
Discussion:
Mental disorders and their causes, nature and cure are related to the symptoms manifested by the specific disordered individual. Usually, the mental illness is co-related with personality or the brain. This poses great difficulty for the individual for even consulting the respective specialists due the fear of society [30]. Similarly, patients with paranoia are prone to suspicion on people and they do not trust anybody and tend to be more secretive and guarded. For the same reason the diagnosis becomes tricky as the patient does not easily trust the therapist. Paranoia is one the most least understood psychotic disorder and also the one which is most difficult to be treated [31].
Paranoia is manifested in almost all psychotic disorders; hence it becomes difficult to diagnose paranoia individually. Patients with chronic paranoia may be diagnosed easily when compared to patients with lower degree of paranoia due to the intensity of delusions. Paranoic patients usually do not require hospitalisation, as some of the patients can easily cope up with the delusions. Whereas, in severe cases where patients are uncontrollable, hospitalisation may be required. These patients have high levels of anxiety and are prescribed with tranquilising agents such as chlorpromazine. Few of the common medications with their recommended doses are as given (Table 2)
|
Sr. No. |
Drug |
Daily dose range (µg per day) |
|
1. |
Promazine |
40-800 |
|
2. |
Triflupromazine |
30-50 |
|
3. |
Acetophenazine |
40-80 |
|
4. |
Methotrimeprazine |
40 - 120 |
|
5. |
Levomepromazine |
40 - 120 |
|
6. |
Thioridazine |
300 - 800 |
|
7. |
Butaperazine |
15 -100 |
|
8. |
Trifluoperazine |
10 - 40 |
Table 2: Tranquilising agents used in paranoia
True paranoia is usually mentioned to be incurable. Even though incurable these patients can easily live in the society on medications for anxiety and delusions. With medications the delusions of the patients can be kept at bay. In general, the diagnosis and prognosis of paranoia is difficult, but is not fatal and the patient can be managed to lead a normal life [32].
Conclusion:
Paranoia as a mental disorder is not completely understood, be it be its nature, diagnosis, treatment and prognosis. Hence, there is a scope for research and development in this direction. Also, various aspects such as aggression, suicidality, drug abuse, gender dysphoria seems to be very common traits of paranoia, hence it necessitates early identification, prevention and cure.