Clinical Psychology and Mental Health Care
OPEN ACCESS | Volume 7 - Issue 1 - 2025
ISSN No: 2994-0184 | Journal DOI: 10.61148/2994-0184/CPMHC
Kathy Sexton-Radek
Elmhurst University, Elmhurst/Suburban Pulmonary & Sleep Associates, Westmont, IL, USA
*Corresponding Author: Kathy Sexton-Radek, Elmhurst University, Elmhurst/Suburban Pulmonary & Sleep Associates, Westmont, IL, USA.
Received: August 13, 2021
Accepted: August 30, 2021
Published: September 15, 2021
Citation: Kathy Sexton-Radek. “Adult Parasomnia Case Revealed in Insomnia Clinic”. Clinical Psychology and Mental Health Care, 3(3); DOI: http;//doi.org/03.2021/1.10047.
Copyright: © 2021 Kathy Sexton-Radek. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
Thirty-three-year-old male presented to Insomnia Clinic with a positive history of sleep onset latency insomnia, intermittently for eight years and a childhood history of sleep terrors and somnambulism. The patient’s medical history is positive for nicotine use 2 ppd x 18 years (since age 15), moderate alcohol use and denial of recreational drug use. The patient’s surgical history is positive for tonsillectomy at age 7, anterior cruciate ligament surgeries: right at age 18, left at age 27. Patient has COVID-19 vaccine and all childhood/adolescence inoculations. Patient’s BMI is 26.7. Patient reported last physical exam laboratory findings indicated Hyperlipidemia (he has positive family history) and that last two measures of blood pressure were elevated. Diet and life style control were indicated for the HL and HTN warnings. Patient denies psychiatric conditions and family history. The patient is _______ time three. He spoke clearly with good eye contact. Patient denied falls, stated he has had two care accidents without severe injury. The patient reported his appetite as good with three meals per day and two snacks. He stated that he purchases his food as he does not cook. The patient lives alone with his family of origin (father, mother, brother age 25, sister age 20 living in family home eleven miles away. The patient stated that he’s not currently in a relationship. The patient completed two years of community college “pre-engineering” program then stopped to take his current position as a construction worker for commercial buildings for the last thirteen years. He stated that is hobbies are viewing films and video games. He describes friendship with two co-workers, a neighbor and a friend from high school. He stated his family is his main source of social support.
Introduction:
A case study of an adult sleeper presenting to an Insomnia Clinic is discussed. Following the intake interview and clinical sleep history was completed that identified confusional arousal episodes and a positive childhood history for somnambulism and sleep terrors. The assessment with standard measures was conducted including Actigraphy was administered. The patient was treated with a cognitive behavioral therapy for insomnia (CBTi) with the integration of components to address the parasomnia episodes. Treatment findings were favorable in terms of good patient engagement, adherence to sleep schedule changes, reduce sleep efficiency and use of skills (e.g., mindfulness). Sleep medicine research and concepts related to the case are presented.
Assessment:
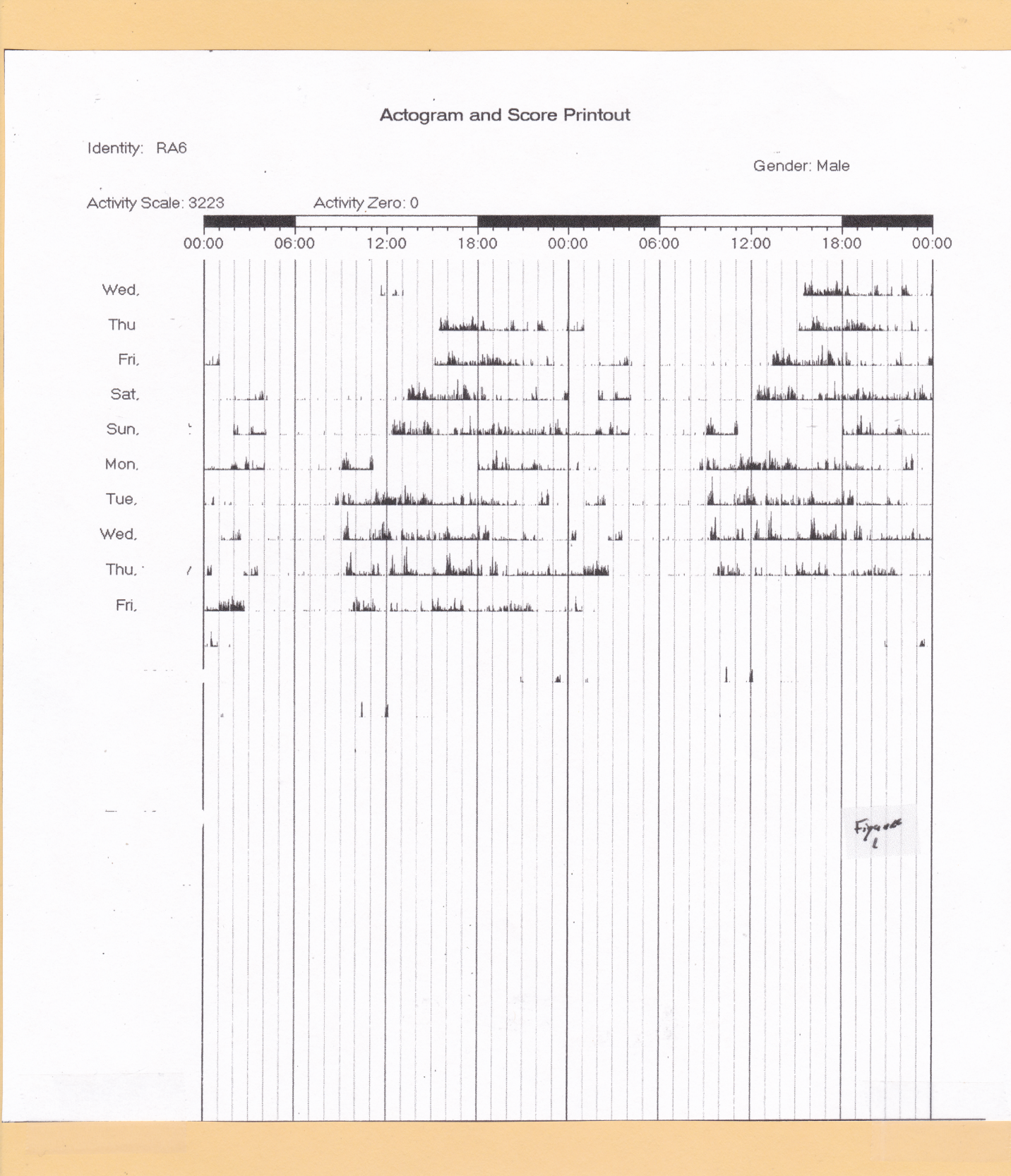
The patient was referred to the insomnia Clinic by his PCP based on his comments of sleep disturbance. The patient completed the Pittsburgh Sleep Quality Index with a score of 11, the Epworth Sleepiness Scale with a score of 6. The patient seemed uncertain of his bedtime/waketimes on the third day recall diary task and indicated non-compliance on the sleep log sent to him with other self-report measures about his sleep as part of the Insomnia Clinic protocol. The patient was provided with an explanation and contract to wear the Actiwatch for the week. Sleep history questions were positive for sleep terror and somnambulism. Figure 1 depicts the findings from the Actiwatch for the 10/14 days compliance. The tabulations below the table confirm essential findings of insomnia with decreased sleep efficiency, increase percent awake, and increased Sleep Latency. The fragmentation index findings are remarkable. The clinically indicates excessive movement. On day 5 of the actigraph recordings that corresponds to the session two of the treatment, the patient brought Figure 2 to the session. His only comment accompanying the figure was “something… somebody like this came at me.” Modified CBTi was recommended two weekly sessions then two bimonthly sessions and then a follow-up session. The patient was encouraged to adhere to PCP recommendations for dies/lifestyle changes to address HL and HTN. The patient does not take medication.
|
Score Report |
|||||||||
|
|
Wed |
Thu |
Fri |
Sat |
Sun |
Mon |
Tues |
Wed |
Thu |
|
Sleep Efficiency |
92 |
78.4 |
71.2 |
70.3 |
88.3 |
67.7 |
92.4 |
91.8 |
84.8 |
|
Awake % |
0 |
14.8 |
22.6 |
23.1 |
24.2 |
22.6 |
17.4 |
14.6 |
22.5 |
|
Fragmentation Index |
0 |
75.2 |
64.0 |
65.1 |
89.2 |
88.6 |
73.4 |
62.1 |
64.7 |
|
Increased Sleep Latency (>30 min) |
+ |
+ |
+ |
+ |
+ |
+ |
+ |
+ |
+ |
|
Note: Sleep efficiency = 100(minutes asleep/minutes in bed); Awake % = percentage of minutes awake; Fragmentation Index = the amount of movement or restlessness in a deep period |
|||||||||
|
Decreased Total Sleep Time |
+ |
+ |
+ |
+ |
+ |
+ |
+ |
+ |
+ |
Figure 1. Actigraphy Study: Actogram and Score Report

Note: Patient brought to session 2 (8th day actigraphy) stated “something… somebody like this came at me.”
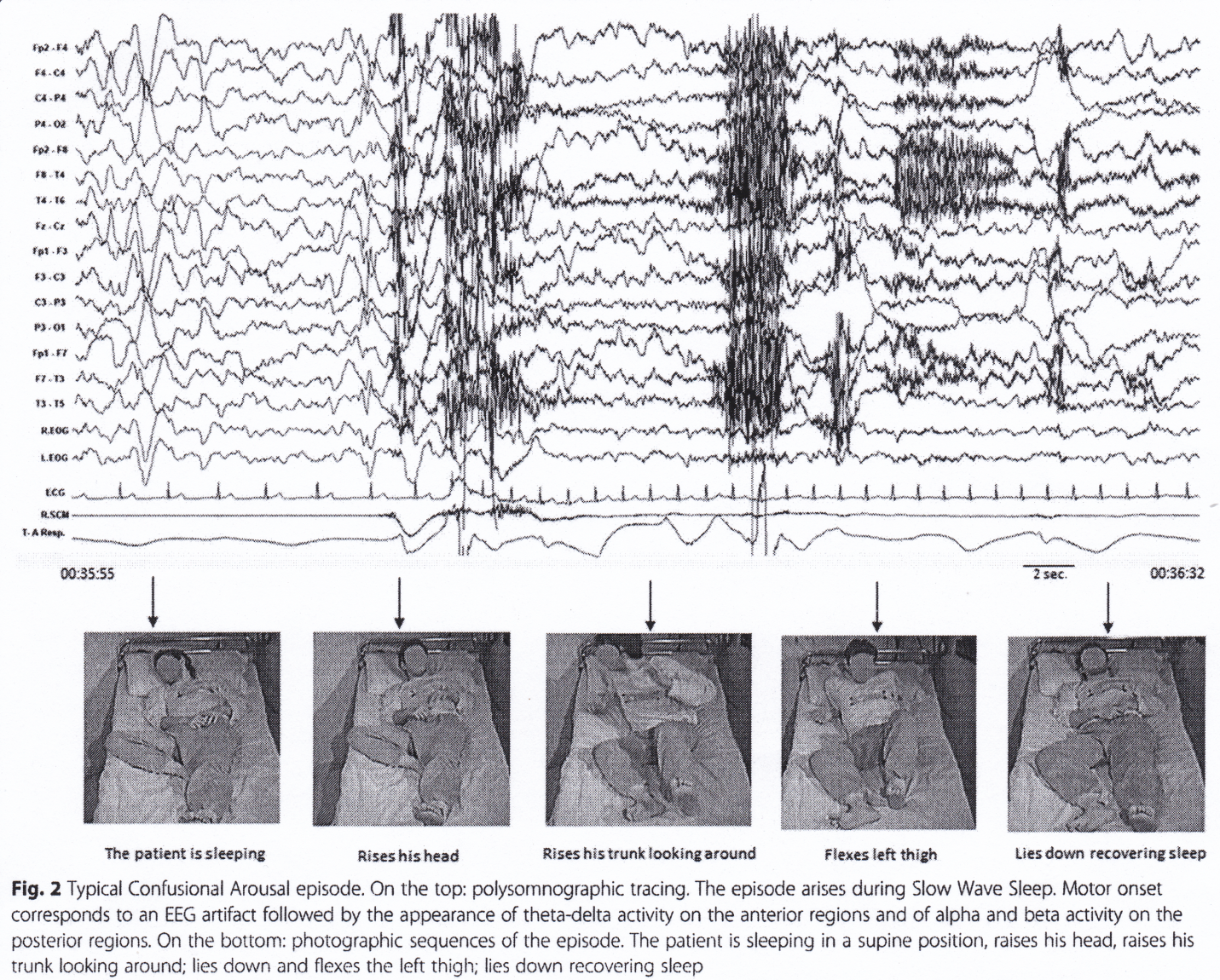
From: Loddo, Lopez, Cilea, Dauvilliers, Provini, 2019.
Therapeutic assistance with his diet and lifestyle recommendations from his PCP and substance use counseling (nicotine, alcohol). The patient agreed.
Discussion of Sleep Medicine Research and Concepts:
Confusional arousals are considered a parasomnia sleep disorder with higher prevalence in children (17%) than adults (34%). Clinical reports have identified the occurrence of confusional arousals to be as the sleeper wakes up or immediately following waking up or as they sleeping or falling asleep. The confusional arousal occurs as an abrupt interruption from nREM stage 3/4 sleep. Sleepers are either amnestic or unable to clearly state what they have experienced in a confusional arousal. Disruptions to the sleeper’s sleep cycle from episodes of sleep deprivation, substance use, sleep disorders of Sleep Apnea or Periodic Limb Disorders, Psychotropic Medicines, Substance Abuse and Mental Disorder symptoms such as Post Traumatic Stress Disorder. Markov, Jaffe and Doghram (2006) reported 6% of 16-24 year population experienced confusional arousals with the characteristic sustained period of impaired vigilance, thinking and performance. Confusional arousal as a break in the transition from nREM stage 3/4 sleep to REM stage 2 then nREM stage 1 then wake is triggered may also transition into a sleep terror as the case study sleep experienced (Markov, Jaffe & Doghram, 2006). Loddo, Lopez, Cilea, Dauvilliers and Provini (2019) recommend a diagnostic process of video-polysomnographic tools for more precise measurements and enhanced differential diagnosis (e.g., Confusional Arousals as measured in the laboratory with the specified settings of Loddo, Lopez, Dauvilliers, Provini (2019). Stores (2020) indicated the importance in considering diagnostic clinical interview and polysomnogram measures to consider “overlap” conditions and nocturnal epilepsies.
The Actigraphy measurement of sleep wake activity used in this assessment and treatment planning for this case is commonly done where son-compliance or uncertainty of the sleeper about their sleep behavior exists. This validated, non-invasive accelerometer device provides objective patient information in a naturalistic environment.
Itis noted that Actigraphy has a common use in the assessment of insomnia as a valid quantified measure of sleep behavior (Natale, Plazzi, & Martoni, 2009; Sexton-Radek, 2018). Insomnia is the most common sleep disorder with a 30% of adults and chronic insomnia by 10% (National Sleep Foundation).
The CBTi treatment was modified to include processing of the confusional disorder, explanation of stress factors and stress management. The emphasis in CBTi on sleep science basics, sleep hygiene, training n mindfulness, exploration of cognitive-emotional factors related to sleep and the resetting of the patient’s sleep pattern were useful to the case study patient. Mundt and Baron (2021) describe the utility of integrating behavioral health treatment for nREM parasomnias.
CBTi session summary: The patient used the session time for focused tasks of learning basics of sleep science, becoming more knowledgeable of his sleep schedule, using stimulus control techniques if it took him longer than thirty minutes to fall asleep. The patient used the reading of his microwave manual and re-reading car and motor magazines as his tasks to elicit sleepiness. The patient presented more information about himself in the session. During session 2 he brought in Figure 2 stating “something… somebody like this came at me.” He stated he was unable to recall other figures but stated that family members and bed partners have commented on his thrashing in bed for a few seconds was repeated five to six times a night and adjusting and picking at his bed shirt. The patient remarked that these reports have been since late teens but before that he sleepwalked and as a toddler would loudly scream and get scared his parents reported. The patient added that he also has a new current hobby of the last three months at his local tavern that he frequents of “travel club” nights. He related that these events, …? were to other taverns and involved various drinking games and contests that he participated in. The patient was compliant with session process and stimulus control work. He demonstrated difficulty in adjusting his sleep schedule The patient’s sleep efficiency by follow-up, based on recall during the session was 84% (adequate). Recommendations were made for continued supportive psychotherapy. The sleep hygiene component of the CBTi was expanded to include topics of patient safety, adhering to the sleep schedule to extinguish sleep deprivation. The case study patient agreed to continue therapy to focus on smoking cessation and discuss his substance-alcohol use. Sleep hygiene typically focuses on reduction of nicotine and alcohol use, particularly at pre-sleep (Sexton-Radek and Grace, 2021). Hypnosis, scheduled awakenings, psychotherapy and pharmacological interventions in severe symptomology cases has been recommended. Benzodiazepines reduce nREM stage 3/4 sleep (i.e., slow wave sleep) and have some efficacy with intense cases (George, Lentz, Beneciuk, Bhavsar, Mundt & Boissoneau, 2020; Wilson, Anderson, Baldwin, Dijk, Espie, Espie, Gringras & Krystal, 2019). An additional component that was added to the CBTi treatment was the discussion of…
In effect, the CBTi treatment process provided ongoing assessment of the case study patient’s sleep and response to treatment. The improvement in sleep efficiency which includes a reduction in sleep deprivation as well as the therapeutic process of sleep hygiene strategies, use of mindfulness and stress management lend to a reduction to zero of the confusional arousals. Determining the underlying factors providing the intrusion out of nREM sleep in parasomnias as essential start to working with the case.
Conclusion: