
Robert Skopec
Free-Lance Science Writer, Dubnik, Slovakia
*Corresponding Author: Robert Skopec, Free-Lance Science Writer, Dubnik, Slovakia.
Received: July 19, 2021
Accepted: August 16, 2021
Published: August 18, 2021
Citation: Robert Skopec. “Pathophysiology of The Covid-19”. Clinical Psychology and Mental Health Care, 3(2); DOI: http;//doi.org/03.2021/1.10043.
Copyright: © 2021 Robert Skopec. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
During the recent weeks, anosmia without nasal or other symptoms has been recognized as an alarming sign of early-stage COVID-19 [1]. This might indicate that SARS-CoV-2, when entering the body via the nose, may be neurotropic, have affinity for the olfactory epithelium and advance along the olfactory nerve into the CNS, causing early-stage CNS infection. This route is a known shortcut for influenza and other viral diseases into the CNS [1]. Viral infection of the CNS can lead to damage from infection of the nerve cells, from an immune response, or from combination of both. Anosmia has also occurred in a few patients with SARS and MERS and, during the 2002/2003 SARS epidemic, SARS-CoV was reported in brain tissues in both patients and experimental animals with a heavily infected brainstem. Considering the great similarities between SARS-CoV and SARS-CoV-2, it is likely that their infective characteristics are highly comparable as well. The early CNS symptoms, such as headache, nausea, and vomiting have also been reported in patients with COVID-19, leading Li et al. (2020) to conclude that coronaviruses are not confined to the respiratory tract but may also invade the CNS and induce neurological diseases [2].
Viral invasion to CNS
It is likely that the pathogenesis of SARS-CoV-2 mimics that of other respiratory viruses. Therefore, it is not surprising that there are reports of COVID-19 cases with only mild upper respiratory tract symptoms [3]. The virological analysis by Wölfel et al. showed that the highest viral replication occurred in the upper respiratory tract at day 4. They found no virus in circulation.
Convincing prior research using animal disease models has shown, that not only is the olfactory nerve a shortcut for several viral diseases into the CNS [4], but also that the specific SARS-CoV-2 receptor, ACE2, is abundantly and widely expressed in brain neurons, including olfactory and motor cortical areas and also in the medullary vagal complex both in normal healthy mice [5] and in mice and hamsters intranasally inoculated with SARS-CoV [6]. Furthermore, the extensive neuronal infection was the main cause of death with only minor infection in the lungs [6]. These studies on mouse models revealed that intranasally administered SARS‐CoV enters the brain primarily via the olfactory bulb, followed by rapid transneuronal spread to connected areas, including the thalamus and the brainstem.
In humans, however, the mechanisms of possible viral transport via the olfactory nerve and subsequent spread in the CNS are poorly understood. The viruses could travel within olfactory neurons by axonal flow, by travel within axons ensheathing cells or transcellularly through the tight junctions between ciliated epithelial (brush) cells. The brush cells of the olfactory epithelium resemble the pseudostratified columnar respiratory epithelial cells of the nasal cavity. Both types of cells are innervated by the anterior ethmoid branch of the trigeminal nerve. Therefore, the trigeminal pathway may form an alternative route for the transmission of a virus from the nasal cavity into the CNS. The trigeminal route is particularly interesting as it leads directly to the caudal brain regions, to the trigeminal nuclei in the brain stem, and thus to the vicinity of the respiratory nuclei. Prior work utilizing radiolabeled proteins in rats and primates has shown that intranasally applied macromolecules may be transported via the olfactory pathway to the rostral brain regions or via the trigeminal pathway to the trigeminal nuclei and caudal brain regions within 30–60 min of administration [7]. It was speculated that this rapid transport was likely taking place along the perivascular or lymphatic paths. It may be that the virus invades along the ‘higher’ olfactory route that primarily leads to dysfunction of the central autonomous network (CAN) and further to respiratory problems. On the other hand, viral invasion along the ‘lower’ trigeminal pathway could directly affect the respiratory nuclei. It is to be noted that the CNS spread could also result from the nasopharynx that is innervated by the glossopharyngeal nerve (CN IX). A putative glossopharyngeal pathway would also lead directly to the brainstem – and to the vicinity of respiratory nuclei.
Dysfunction of the Central autonomic network (CAN)
When causing anosmia SARS-CoV-2 might enter the CNS via the olfactory or trigeminal route. Initially, the CNS infection or inflammation could be relatively mild and cause olfactory damage and imbalance of the autonomic nervous system (ANS). It is known that the regulation of ANS occurs via the interaction of various brain structures, which contribute to CAN. It is now known that the parasympathetic vagal system (through CAN) effectively regulates respiration and that the vagus nerve contains sensory neurons that critically regulate respiration rate, the airway tone and defense, and in some species, evokes cough [8]. Therefore, all early-stage extrapulmonary symptoms in COVID-19 could be due to sympathetic dominance (and reduced parasympathetic function). Imbalance of CAN (with sympathetic dominance, as detected by the heart rate variability (HRV) test, has been seen in viral CNS infections, for example in tick-borne encephalitis [9].
Early respiratory distress and hypoxia may be of Central origin
The most prominent symptom of hospitalized COVID-19 patients is dyspnea often associated with hypoxia. According to published reports, most often the dyspnea presents as ‘difficult breathing’ or sensations of chest tightness and air hunger, which are the classic definitions of dyspnea [10]. However, there are also reports of COVID-19 patients presenting with asymptomatic hypoxia and many have described early dyspnea as a ‘cessation of spontaneous breathing’ [2]. These features may suggest a central apnea or failure in the feedback loop from the pulmonary receptors to the respiratory centers, mediated by the vagus nerve [8]. Hypoxia may also result from a combination of these two. Furthermore, patients experiencing dyspnea along with high fever may, boosted by a fear of the corona infection, be driven to experience stress, panic and forced breathing (tachypnea > 30 cycles/min). Such stress may further reduce parasympathetic activity, thus worsening the situation. In addition, forced breathing or hyperpnea may lead to lesions in the lungs (alveolar micromechanics), specifically to the epithelium-endothelium barrier [11], and could ultimately cause pulmonary damage. Alveoli are normally protected from over-distention by a reflex (Hering–Breuer, which normally protects from overdistention but is now absent because of non-functioning CAN/vagal system) and two stabilizing factors: a connective tissue fiber network and the surfactant system. The backbone of this stabilizing system is the network of elastic fibers which become strained and stressed at larger lung volumes. Increased strain at the cellular level particularly to the elastic components of this network might occur even under physiological conditions, e.g. upon deep inspirations, during physical exercise or sighs [12]. It is to be noted that tolerance to stresses related to the elastic recoil pressure has been shown to be significantly reduced, not only in COPD, smokers and exercise but also in aged individuals [12]. The damaged lungs are easily infected by a virus descending to the lungs from the upper airways, or by a virus simply penetrating the alveolar epithelia in the same pattern as in the nose. It is this damage to the alveolar micromechanics and barrier function that makes some individuals (about 5%) vulnerable and spurs the development of ARDS. Therefore, if lungs that are already damaged are mechanically (invasively) ventilated, the prognosis seems to be poor. It is well established that in the pathogenesis of ARDS, a contribution of ventilator-associated lung injury (VALI), even if ventilation is performed in full accordance with current recommendations, may play a role in vulnerable patients [11].
Nasal respiratory and olfactory epithelia have specific receptors for SARS-CoV-2
The current novel COVID-19 pandemic has stimulated numerous research groups to investigate the pathogenetic features of the SARS-CoV- 2 spike (S)-protein that binds ACE2 and, in concert with host proteases, principally TMPRSS2, promotes cellular entry. The latest reports state that ACE2 and TMPRSS2 are co-expressed cells in epithelial type II pneumocytes in the lungs, but also in ciliated and goblet cells of the nasal epithelium [13]. One study reported that nasal respiratory epithelium has a higher expression of CoV-2 entry genes than that of the lungs [14]. In addition, Brann et al. [15] demonstrated that the CoV-2 receptor ACE2 and the spike-protein protease TMPRSS2 are expressed not in the olfactory sensory neurons but in support cells, stem cells, and perivascular cells of the olfactory epithelium.
Many COVID-19 patients with early hypoxia and neurological symptoms show normal CT scans
Several clinical and radiological studies report normal chest imaging findings despite severe illness. Guan et al. [16] reported >1000 COVID-19 patients requiring hospital care or ICU admission, of whom up to 23% and 12% had a normal chest radiograph and CT scans, respectively. Similarly, Goh et al. [17] described a patient with, despite rapid clinical deterioration, only subtle chest CT changes. The ensuing likely diagnosis was septic encephalopathy. Furthermore, in reports from the 2002/2003 SARS epidemic, chest radiography on admission was normal in approximately 25% of individuals. This indicates that in about one quarter of patients, early symptoms, including respiratory distress, could not be explained by pulmonary changes.
Long-term outcome studies of many SARS survivors show debilitating neurological sequelae but normal lung function
Multiple studies report on the one-year and long-term outcomes of SARS survivors in Toronto 2003, (where 273 people were identified as being confirmed SARS cases, of which 44 died). Most had persistent functional disability due to extrapulmonary conditions one year after discharge from the intensive care unit. These patients were young (median age 45 years) and their lung volume and spirometric measurements were already normal within 6 months. In a cohort of 22 post-SARS patients (21 were hospital workers) who remained disabled and unable to return to their work, the long-term outcome (>1 year) showed persisting debilitating physical symptoms including variable musculoskeletal pain, profound weakness, easy fatigability, shortness of breath that accompanied psychological distress and major sleep problems [18,19]. These neurological long-term sequelae strongly suggest that they had been caused by an infection or inflammation in the CNS, not in the lungs.
Discussion
It seems evident that the earliest COVID-19 symptoms, including respiratory distress and hypoxia, are best explained by primary replication of SARS-CoV-2 in the nasal and/or olfactory epithelia, followed by invasion of the virus into the CNS, and that the ARDS is a later complication. Our proposed theory differs from the predominant views of COVID-19 pathogenesis being primarily a pulmonary one-organ disease, with pneumonia and bronchiolitis leading to dyspnea, and in the most severe cases, to ARDS and septic shock. According to our concept, the early dyspnea and/or hypoxia often, if not in most cases, are not of pulmonary but of central origin.
It is well established that currently COVID-19 lacks curative therapy. However, if our concept holds and the early dyspnea and hypoxia are due to a dysfunction of the central regulatory mechanisms of respiration, it shifts the main focus of therapeutic efforts to the stage of early hypoxia. Our pathophysiological concept suggests that therapeutically the most important step would be to use all possible means to correct the hypoxemia by optimizing the efficacy of spontaneous breathing in affected individuals.
We also wish to stress, that the role of ANS and particularly the CAN part of that in the disease process of COVID-19, appears to be crucial from the first symptoms to the final stage. Therefore, returning autonomic imbalance back to normal might be important as part of the therapeutic regimen. Such adjunctive treatment modalities might provide various means aimed for improving the parasympathetic system activity. All the early extrapulmonary symptoms of COVID-19 can be due to sympathetic dominance (and reduced parasympathetic function). In addition, both the CNS and pulmonary disease are probably caused, and the pulmonary infection accentuated through inflammatory reflex mechanism due to inadequate immunological defense by the neuro-immune axis [20]. Excessive inflammation plays an important role in the pathogenesis of common and debilitating diseases including septic shock.
In conclusion, as the COVID-19 lacks curative therapy, we propose that the probable dysfunction of the central regulation of respiration and the ensuing respiratory distress should be considered in planning treatment strategies.
Naphazoline Nitrate, Bisacodyl and Guttalax Treat Microwave Sonic Effects
At the end of the December 2018 we have found a medicine fully treating the damages caused the Frey Effect of Microvawe and other types of Sonic Weapons in Human’s internal, endogenous organs. I am proposing to use Naphasoline nitrate, (former) nasal decongestatnt, to treat Carcinogenesis of the Human’s internal, endogenous organs caused by Sonic Weapons through the release and cleaning of the Lymphatic ways in patients with colorectal, colon, pancreatic, breast, etc., cancer. I have proved this healing effect of the Naphazoline nitrate on Myself during treatment in last months of the year 2018. Naphazoline Nitrate, Bisacodyl and Guttalax are clearing the Pylorus in human digestive system and treat so the Microwave Sonic Effects.
Sonic Weapons
Exposure to microwave, infrasound, etc., sonic weapons has been demonstrated to affects recipients with symptoms including fear, sorrow, depression, anxiety, nausea, chest pressure and hallucination. It can cause objects to move through vibration and the body’s internal organs can be affected. [21, 22]
Materials and Methods
The term infrasonic applied to sound refers to sound waves below the frequencies of audible sound. Nominally includes frequencies under 20 Hz. Sources of infrasound in nature includes volcanoes, avalanches, earthquakes and meteorites.
The healthy human ear can hear frequencies ranging from 20 Hz to 20,000Hz. Over time, the hair-like stereocilia may get damaged or broken. If enough of them are damaged, hearing loss results. The high frequency area of the cochlea is often damaged by loud sound.
Infrasound is sound which extends below the range of human hearing (from 20 Hz to 0.001 Hz), and it emitates from many natural and man-made sources. For example, some animals, such as whales, elephants and giraffes communicate using infrasound over long distances.
Sonic and ultrasonic weapons (USW) are weapons of various types that use sound to injure, incapacitate, or kill a target. New personal communications shows that infrasound can cause trough vibrations, resonance frequency about 7 Hz with internal organs of humans cause also cancer, such as colorectal cancer, colon cancer, pancreatic cancer, etc. [22, 23, 24]
Some of these weapons have been described as sonic bullets, sonic grenades, sonic mines, or sonic cannons. Some USWs make a focused beam of sound or ultrasound, some made an area field of sound.
As an example of used sonic weapon we can use The LRAD Sound Cannon as an acoustic weapon and communication device. Developed by the LRAD Corporation to broadcast messages and pain-inducing deterrent tones over long distances. LRAD devices come in various iterations that produce varying degrees of sound. They can be mounted to a vehicle or handheld.
Protests in Fergusson, Missouri have reached a terrifying fever pitch, and the ludicrously armed Fersguson Police Department is bringing all its crowd-control weapons to bear, tear gas, stun grenades, rubber bullets. One of the most controversial of those is the LRAD Sound Cannon. The device produces a sound that can be directed in a beam up to 30-degress wide, and the military-grade LRAD 2000X can transmit voice commands at up to 162 dB up to 5.5 miles away.
The LRAD Corporation says that anyone within a 100 meters of the device’s sound path will experience an extreme pain. The version generally utilized by Police Departments (the LRAD 500X) is designed to communicate at up to 2000 meters during ideal conditions. In a typical outdoor environment, the device can be heard for 650 meters. The 500X version is also capable of short bursts of directed sound that cause headaches in anyone within a 300 meter range. Anyone within 15 meters of the device’s audio path can experience permanent hearing loss. LRAD claims the device is not a weapon, but a directed-sound communication device. [23, 24]
Developing a new class of weapons
Allan H. Frey, has lived at his home outside Washington. In 1960, he stumbled on an acoustic effect of microwaves that was eventually named after him. Microwaves are ubiquitous in modern life. The short radio waves power radars, cook foods, relay messages and link cellphones to antenna towers. They’re a form of electromagnetic radiation on the same spectrum as light and X-rays, only at the opposite end.
While radio broadcasting can employ waves a mile or more in length, microwaves range in size from roughly a foot to a tiny fraction of an inch. They’re seen as harmless in such everyday uses as microwaving foods. But their diminutive size also enables tight focusing, as when dish antennas turn disorganized rays into concentrated beams.
The dimensions of the human head, scientists say, make it a fairly good antenna for picking up microwave signals. Mr. Frey, a biologist, said he stumbled on the acoustic effect in 1960 while working for General Electric’s Advanced Electronics Center at Cornell University. A man who measured radar signals at a nearby G.E. facility came up to him at a meeting and confided that he could hear the beam’s pulses — zip, zip, zip. Intrigued, Mr. Frey traveled to the man’s workplace in Syracuse and positioned himself in a radar beam. “Lo,” he recalled, “I could hear it, too.”
Mr. Frey’s resulting papers — reporting that even deaf people could hear the false sounds — founded a new field of study on radiation’s neural impacts. Mr. Frey’s first paper, in 1961, reported that power densities 160 times lower than “the standard maximum safe level for continuous exposure” could induce the sonic delusions. His second paper, in 1962, pinpointed the brain’s receptor site as the temporal lobes, which extend beneath the temples. Each lobe bears a small region — the auditory cortex — that processes nerve signals from the outer and inner ears. Investigators raced to confirm and extend Mr. Frey’s findings. At first they named the phenomenon after him, but eventually called it the microwave auditory effect and, in time, more generally, radio-frequency hearing.
Tinnitus: Ringing in the ears and what to do about it
Tinnitus (pronounced tih-NITE-us or TIN-ih-tus) is sound in the head with no external source. For many, it's a ringing sound, while for others, it's whistling, buzzing, chirping, hissing, humming, roaring, or even shrieking. The sound may seem to come from one ear or both, from inside the head, or from a distance. It may be constant or intermittent, steady or pulsating. [23, 24]
Almost everyone has had tinnitus for a short time after being exposed to extremely loud noise. For example, attending a loud concert can trigger short-lived tinnitus. Some medications (especially aspirin and other nonsteroidal anti-inflammatory drugs taken in high doses) can cause tinnitus that goes away when the drug is discontinued. When it lasts more than six months, it's known as chronic tinnitus. As many as 50 to 60 million people in the United States suffer from this condition; it's especially common in people over age 55 and strongly associated with hearing loss. Many people worry that tinnitus is a sign that they are going deaf or have another serious medical problem, but it rarely is.
Most tinnitus is subjective, meaning that only you can hear the noise. But sometimes it's objective, meaning that someone else can hear it, too. For example, if you have a heart murmur, you may hear a whooshing sound with every heartbeat; your clinician can also hear that sound through a stethoscope. Some people hear their heartbeat inside the ear — a phenomenon called pulsatile tinnitus. It's more likely to happen in older people, because blood flow tends to be more turbulent in arteries whose walls have stiffened with age. Pulsatile tinnitus may be more noticeable at night, when you're lying in bed and there are fewer external sounds to mask the tinnitus. If you notice any new pulsatile tinnitus, you should consult a clinician, because in rare cases it is a sign of a tumor or blood vessel damage.
The course of chronic tinnitus is unpredictable. Sometimes the symptoms remain the same, and sometimes they get worse. In about 10% of cases, the condition interferes with everyday life so much that professional help is needed.
While there's no cure for chronic tinnitus, it often becomes less noticeable and more manageable over time. You can help ease the symptoms by educating yourself about the condition — for example, understanding that it's not dangerous. There are also several ways to help tune out the noise and minimize its impact.
Auditory pathways and tinnitus
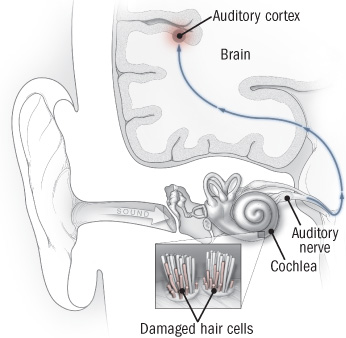
Sound waves travel through the ear canal to the middle and inner ear, where hair cells in part of the cochlea help transform sound waves into electrical signals that then travel to the brain's auditory cortex via the auditory nerve. When hair cells are damaged — by loud noise or ototoxic drugs, for example — the circuits in the brain don't receive the signals they're expecting. This stimulates abnormal activity in the neurons, which results in the illusion of sound, or tinnitus.
|
Auditory pathways and tinnitus
Sound waves travel through the ear canal to the middle and inner ear, where hair cells in part of the cochlea help transform sound waves into electrical signals that then travel to the brain's auditory cortex via the auditory nerve. When hair cells are damaged — by loud noise or ototoxic drugs, for example — the circuits in the brain don't receive the signals they're expecting. This stimulates abnormal activity in the neurons, which results in the illusion of sound, or tinnitus. |
What's going on?
Most people who seek medical help for tinnitus experience it as subjective, constant sound like constant ringing in the ears or a buzzing sound in the ear, and most have some degree of hearing loss. Things that cause hearing loss (and tinnitus) include loud noise, medications that damage the nerves in the ear (ototoxic drugs), impacted earwax, middle ear problems (such as infections and vascular tumors), and aging. Tinnitus can also be a symptom of Meniere's disease, a disorder of the balance mechanism in the inner ear.
Tinnitus can arise anywhere along the auditory pathway, from the outer ear through the middle and inner ear to the brain's auditory cortex, where it's thought to be encoded (in a sense, imprinted). One of the most common causes of tinnitus is damage to the hair cells in the cochlea (see "Auditory pathways and tinnitus"). These cells help transform sound waves into nerve signals. If the auditory pathways or circuits in the brain don't receive the signals they're expecting from the cochlea, the brain in effect "turns up the gain" on those pathways in an effort to detect the signal — in much the same way that you turn up the volume on a car radio when you're trying to find a station's signal. The resulting electrical noise takes the form of tinnitus — a sound that is high-pitched if hearing loss is in the high-frequency range and low-pitched if it's in the low-frequency range. This kind of tinnitus resembles phantom limb pain in an amputee — the brain is producing abnormal nerve signals to compensate for missing input.
Most tinnitus is "sensorineural," meaning that it's due to hearing loss at the cochlea or cochlear nerve level. But tinnitus may originate in other places. Our bodies normally produce sounds (called somatic sounds) that we usually don't notice because we are listening to external sounds. Anything that blocks normal hearing can bring somatic sounds to our attention. For example, you may get head noise when earwax blocks the outer ear.
Some drugs that can cause or worsen tinnitus
Aspirin and other nonsteroidal anti-inflammatory drugs, including ibuprofen (Motrin) and naproxen (Aleve, Naprosyn)
Certain antibiotics, including ciprofloxacin (Cipro), doxycycline (Vibramycin, others), gentamicin (Garamycin), erythromycin (Ery-Tab, others), tetracycline (Sumycin), tobramycin (Nebcin), and vancomycin (Vancocin)
Antimalarial drugs such as chloroquine and quinine
Certain anticonvulsants, including carbamazepine (Tegretol, others) and valproic acid (Depakote, others)
Certain cancer drugs, including cisplatin (Platinol) and vincristine (Oncovin, Vincasar)
Loop diuretics (when given intravenously in high doses), including bumetanide (Bumex), furosemide (Lasix), and torsemide (Demadex)
Tricyclic antidepressants such as amitriptyline (Elavil, others), clomipramine (Anafranil), and imipramine (Tofranil)
Evaluate and treat underlying problems
If you develop tinnitus, it's important to see your clinician. She or he will take a medical history, give you a physical examination, and do a series of tests to try to find the source of the problem. She or he will also ask you to describe the noise you're hearing (including its pitch and sound quality, and whether it's constant or periodic, steady or pulsatile) and the times and places in which you hear it. Your clinician will review your medical history, your current and past exposure to noise, and any medications or supplements you're taking. Tinnitus can be a side effect of many medications, especially when taken at higher doses (see "Some drugs that can cause or worsen tinnitus").
Musculoskeletal factors — jaw clenching, tooth grinding, prior injury, or muscle tension in the neck — sometimes make tinnitus more noticeable, so your clinician may ask you to tighten muscles or move the jaw or neck in certain ways to see if the sound changes. If tight muscles are part of the problem, massage therapy may help relieve it. [25, 26]
Tinnitus that's continuous, steady, and high-pitched (the most common type) generally indicates a problem in the auditory system and requires hearing tests conducted by an audiologist. Pulsatile tinnitus calls for a medical evaluation, especially if the noise is frequent or constant. MRI or CT imaging may be needed to check for a tumor or blood vessel abnormality.
Your general health can affect the severity and impact of tinnitus, so this is also a good time to take stock of your diet, physical activity, sleep, and stress level — and take steps to improve them. You may also be able to reduce the impact of tinnitus by treating depression, anxiety, insomnia, and pain with medications or psychotherapy.
If you're often exposed to loud noises at work or at home, it's important to reduce the risk of hearing loss (or further hearing loss) by using protectors such as earplugs or earmuff-like or custom-fitted devices.
|
Selected resources American Academy of Audiology American Tinnitus Association National Institute on Deafness and Other Communication Disorders |
Managing tinnitus
In addition to treating associated problems (such as depression or insomnia), there are several strategies that can help make tinnitus less bothersome. No single approach works for everyone, and you may need to try various combinations of techniques before you find what works for you. If you have age-related hearing loss, a hearing aid can often make tinnitus less noticeable by amplifying outside sounds.
There is no FDA-approved drug treatment for tinnitus, and controlled trials have not found any drug, supplement, or herb to be any more effective than a placebo. That includes ginkgo biloba, which is sometimes promoted for this purpose. Some patients believe that acupuncture helps, but it too has been found to be no better than a placebo. [27, 28]
The most effective approaches are behavioral strategies and sound-generating devices, often used in combination. They include the following:
Cognitive behavioral therapy (CBT). CBT uses techniques such as cognitive restructuring and relaxation to change the way patients think about and respond to tinnitus. Patients usually keep a diary and perform "homework" to help build their coping skills. Therapy is generally short-term — for example, weekly sessions for two to six months. A 2010 review of six studies by the Cochrane Collaboration (an international group of health authorities who evaluate randomized trials) found that after CBT, the sound was no less loud, but it was significantly less bothersome, and patients' quality of life improved.
Tinnitus retraining therapy (TRT). This technique is based on the assumption that tinnitus results from abnormal neuronal activity (see "What's going on?"). The aim is to habituate the auditory system to the tinnitus signals, making them less noticeable or less bothersome. The main components of TRT are individual counseling (to explain the auditory system, how tinnitus develops, and how TRT can help) and sound therapy. A device is inserted in the ear to generate low-level noise and environmental sounds that match the pitch, volume, and quality of the patient's tinnitus. Depending on the severity of the symptoms, treatment may last one to two years.
When TRT was developed in the 1980s by neuroscientist Dr. Pawel Jastreboff (now at Emory University in Atlanta), it was designed to be administered according to a strict protocol. Today, the term TRT is being used to describe modified versions of this therapy, and the variations make accurate assessment of its effectiveness difficult. Individual studies have reported improvements in as many as 80% of patients with high-pitched tinnitus. In a Cochrane review of the one randomized trial that followed Jastreboff's protocol and met the organization's standards, TRT was much more effective in reducing tinnitus severity and disability than a technique called masking (see below). [29, 30]
Masking. Masking devices, worn like hearing aids, generate low-level white noise (a high-pitched hiss, for example) that can reduce the perception of tinnitus and sometimes also produce residual inhibition — less noticeable tinnitus for a short time after the masker is turned off. A specialized device isn't always necessary for masking; often, playing music or having a radio, fan, or white-noise machine on in the background is enough. Although there's not enough evidence from randomized trials to draw any conclusions about the effectiveness of masking, hearing experts often recommend a trial of simple masking strategies (such as setting a radio at low volume between stations) before they turn to more expensive options.
Biofeedback and stress management. Tinnitus is stressful, and stress can worsen tinnitus. Biofeedback is a relaxation technique that helps control stress by changing bodily responses. Electrodes attached to the skin feed information about physiological processes such as pulse, skin temperature, and muscle tension into a computer, which displays the output on a monitor. Patients learn how to alter these processes and reduce the body's stress response by changing their thoughts and feelings. Mindfulness-based stress reduction techniques may also help.
Other therapies. Other treatments that have been studied for tinnitus include transcutaneous electrical stimulation of parts of the inner ear by way of electrodes placed on the skin or acupuncture needles, and stimulation of the brain using a powerful magnetic field (a technique called repetitive transcranial magnetic stimulation, or rTMS). Transcutaneous electrical stimulation has been shown to be no more effective than a placebo. In two small trials, rTMS compared with a sham procedure helped improve the perception of tinnitus in a few patients.
A solution for constant ringing in your ear
It might not work for everyone, but it could mean precious silence for a lot of tinnitus patients. [31, 32]
Apparently, around 2 million Americans can't work because of tinnitus, and it's also the most common service-connected disability in veterans. The condition doesn't have a cure yet, but those suffering from it might not have to endure all the phantom ringing, clicking and hissing for life, thanks to a device developed by researchers from the University of Michigan. Their creation treats tinnitus by using precisely timed sounds and weak electrical pulses designed to persuade damaged nerves in the region of the brainstem called dorsal cochlear nucleus into working correctly again.
Team leader and U-M Medical School professor Susan Shore explained:
"When the main neurons in [the dorsal cochlear nucleus], called fusiform cells, become hyperactive and synchronize with one another, the phantom signal is transmitted into other centers where perception occurs. If we can stop these signals, we can stop tinnitus. That is what our approach attempts to do..."
The team tested the small, box-like device on guinea pigs first before testing it on 20 tinnitus patients who used it 30 minutes every day for four weeks. It played a sound into the ears and alternated it with precisely timed, mild electrical pulses to the cheek or neck for half the patients. The other half only received sounds. They found that the loudness of the phantom sounds decreased by 12 decibels in some of the patients who received both sounds and electrical pulses. A couple of subjects even said their tinnitus disappeared completely. However, those who only received sounds didn't report a change in their condition.
Due to the way their device works, it can only treat somatic tinnitus. People who have this variant can modulate the phantom ringing/hissing they hear by pressing a part of their face and forehead or clenching their jaw. Thankfully, studies say two-thirds of tinnitus patients suffer from somatic forms of the condition, making their device a promising treatment for most people. The researchers are trying to find a way to make it work just as well for nonsomatic patients, though. They're also conducting more studies and tests to figure out how to make its effects last longer, since the testers' symptoms came back after a couple of weeks.
Shore said:
"We're definitely encouraged by these results, but we need to optimize the length of treatments, identify which subgroups of patients may benefit most, and determine if this approach works in patients who have nonsomatic forms of the condition that can't be modulated by head and neck maneuvers."
Results
Naphasoline Nitrate, Guttalax and Dulcolax treat microwave sonic weapons
The use of naphazoline nitrate may result in an analgesic effect upon first use, through activation of adrenergic and opioidergic systems, followed by a pro-migraine effect via a late induction of an inflammatory cascade, modulated by nitric oxide and arachidonic acid. The observation that naphazoline detoxification relieved the patient’s headache, indicates that prolonged use of naphazoline may cause chronic headaches. Therefore, physicians should ask for details on the use of nasal decongestants in patients complaining of chronic headache, as they could potentially be suffering from a headache caused be the Frey effect of Sonic Weapons use against him. [33, 34]
The headache experienced by the patient was bilateral, throbbing, sometimes very severe, and associated with nausea, vomiting, photophobia, osmophobia and worsened by head movements.
The patient had been treated by his general practicioner (GP) with medication to relieve the headache (metamizole, rizatriptan, zolmitriptan, acetylsalicylic acid, nimesulide, ibuprofen, naproxen sodium), consumed more than once a day, until the age of 24. Since then, he had stopped the consumption of such painkillers because he found that naphazoline nitrate nasal spray was more effective. He began with 2 shots (0,14 mg of drug for any shot) for each nostril 3 times a day, and at the time of presentation, due to pain recurrence, was using the spray 5–6 times a day, and experiencing immediate, yet temporary, relief of the symptoms every time. When asked, the patient said that he had used naphazoline nitrate nasal spray on an occasional basis since the age of 16, in order to self-medicate for self-diagnosed chronic rhinitis.
The chronic headache of the Frey effect disappeared following the treatment suggested by otolaryngologist. After three months of headache diary recording and clinical re-evaluation, the clinical picture was dramatically changed: patient presented only sporadic attacks of migraine without aura (ICHD-II 1.1). By an anamnesis re-evaluation it emerged that an episodic headache arose in childhood and worsen over the years, until it became chronic by the age of 18. One year after naphazoline detoxification, the patient has suffered from a few attacks during the year, treated with triptans.
Naphazoline is a sympathomimetic drug, an imidazolinic derivate with marked alpha-adrenergic activity. It enhances the release of noradrenaline from adrenergic termination, immediately relieving the nasal congestion thanks to its vasoconstricting action on the vessels of nasal mucosa. Because of its adrenergic activity, this drug can also produce adverse effects, like rhinitis medicamentosa, hypertension, headache and acute depression of central nervous system with marked sedation. Moreover, cases of ischemic and hemorrhagic stroke secondary to naphazoline have also been reported, mediated by the alpha1 and alpha2 adrenergic vasoconstrictive effect that is also exerted on brain vessels.
Naphazoline can trigger headaches because of its adrenergic activity Alpha1 receptors are associated with G-proteins that generate a cascade of events leading to the production of arachidonic acid (AA) and nitric oxide (NO). AA and NO release leads to a late inflammatory vasodilatation that could induce a migraine attack. Moreover, it is also possible that the same naphazoline nitrate, consumed by our patient, could have contributed to the production and release of further NO by a chemical reduction of the naphazoline salt. In fact, NO donors are currently used to induce migraine attacks in clinical and experimental settings.
Events induced by naphazoline caused by the Frey effect’s headache.
a. Naphazoline activates α1 receptors that are associated with G-proteins that cause the activation of phospholipase C. Phospholipase C cleavesphosphatidyl-inositol 4,5-bisphosphate (PIP2) into two second messengers, inositol 1,4,5-trisphosphate (IP3) and diacylglycerol (DAG) which in turn cause an increase in the level of calcium and protein kinase C. Diacylglycerol, by DAG lipase, takes part in the creation of arachidonic acid which is a precursor in the production of prostaglandins (PGs), mediated by cyclooxygenase (COX). The higher concentration of intracellular calcium allows an increase in the complex of calcium-calmodulin and therefore the activation of constitutive nitrous oxide synthetase (cNOS) with the generation of nitric oxide. b. Naphazoline nitrate can contribute to the production and release of further NO by a chemical reduction of the naphazoline salt. Prostaglandins and nitric oxide contribute to the activation of nociceptors and the transmission of the pain pulse from the periphery to the centre. Consequently there is a release of substances such as potassium ions, P-substance, bradykinin, histamine, serotonin and CGRP that keep nociceptors active and result in vasodilatation and extravasation of plasma proteins from the vessels. [27-32]
However, despite the late effect as a migraine trigger factor, naphazoline might also have an early action as an anti-migraine agent acting on alpha receptors of muscle, immune cells, Locus Coeruleus and spinal cord. In fact, alpha2 adrenergic receptors have a peripheral analgesic effect, thanks to the activation of opioidergic receptors, via endogenous opioid release. Moreover, both alpha1 and alpha2 adrenergic receptors agonists have been proposed to be specifically useful for the treatment of migraine by mechanisms that mediate the early vasoconstrictive effect related to their activation, similarly to triptans that carry out an analgesic action through the serotoninergic agonism that also mediates vasoconstriction.
Possible early events that induce peripheral analgesic effect.
a. Naphazoline activates alpha1 receptors that are associated with G-proteins that cause the activation of phospholipase C. Phospholipase C cleaves phosphatidyl-inositol 4,5-bisphosphate (PIP2) into inositol 1,4,5-trisphosphate (IP3). Consequently there is a smooth muscle contraction due to an increase of intracellular calcium. b. Alpha-Receptors on immune cells release β-endorphins that cause opioid analgesia. c. Activation of alpha2 adrenoceptors in the Locus Coeruleus and spinal cord provokes the depression of nociceptive transmission.
We could therefore presume that in our patient, in a similar manner to the "triptans effect", naphazoline could exert an antimigraine action but also induce a rebound chronic headache due to medication overuse and/or a proinflammatory cytokine-mediated headache induction. Indeed, our patient had experienced such a sudden analgesic effect; otherwise he would not have continued to take naphazoline. [23, 24]
Bisacodyl (INN) is an organic compound that is used as a stimulant laxative drug. It works directly on the colon to produce a bowel movement. It is typically prescribed for relief of episodic and chronic constipation and for the management of neurogenic bowel dysfunction, as well as part of bowel preparation before medical examinations, such as for a colonoscopy.
Bisacodyl is a derivative of triphenylmethane. It was first used as a laxative in 1953 because of its structural similarity to phenolphthalein.
Bisacodyl is marketed under the trade names Dulcolax/Durolax, Muxol, Fleet, Nourilax, Alophen, Correctol, and Carter's Little Pills (formerly Carter's Little Liver Pills), as well as being available generically. It is usually sold as 5 mg tablets, 10 mg suppositories, or 5 mg pediatric suppositories. It is also available as a 1.25 US fluid ounces (37 ml) pre-packaged enema containing a 10 mg delivered dose of liquid bisacodyl.
When bisacodyl is administered orally, it is usually taken at bedtime. Oral administration is known to produce no action for more than eight hours and then to work suddenly and relatively quickly. This is especially true if more than 10 mg is taken at one time. Normally, the dosage is 5 or 10 mg, but up to 30 mg can be taken for complete cleansing of the bowel before a procedure. [35, 36]
When administered rectally in suppository form, it is usually effective in 15 to 60 minutes. For optimal use, if used as a suppository, it is recommended that bisacodyl be given after breakfast to synchronize with the gastrocolic reflex. Two suppositories can be inserted at once if a very strong, purgative, enema-like result is needed. A few hours after the initial evacuation, there can be a secondary action which will continue as long as there is unexpelled bisacodyl present in the rectum. As a commercially prepared micro-enema, it is usually effective in 5 to 20 minutes.
Bisacodyl works by stimulating enteric nerves to cause peristalsis, i.e., colonic contractions. It is also a contact laxative; it increases fluid and salt secretion. The action of bisacodyl on the small intestine is negligible; stimulant laxatives mainly promote evacuation of the colon.
Guttalax Dosage form, composition and packaging
Drops for internal use in the form of a clear, slightly viscous solution, from colorless to slightly yellowish or slightly yellowish brown.
|
|
100 ml |
|
sodium picosulphate monohydrate |
750 mg |
Guttalax Pharmacological action
Laxative. The active ingredient - sodium picosulphate - is a laxative of the triarylmethane group.
As a locally acting laxative, sodium picosulphate after bacterial cleavage in the colon has a stimulating effect on the mucosa of the colon, increasing motility, and promotes accumulation of water and electrolytes in the colon. This leads to the stimulation of defecation, reduction of evacuation time and stool softening. In case of simultaneous use of Guttalax in high doses and diuretics or GC the risk of electrolyte imbalance (hypokalemia) is increased. Simultaneous administration of antibiotics may reduce the laxative effect of Guttalax. Electrolyte imbalance may increase sensitivity to cardiac glycosides. Symptoms: in case of high doses administration there may be diarrhea, dehydration, decreased blood pressure, disruption of water and electrolyte balance, hypokalemia, cramps. In addition, there were reports of ischemia of the colon associated with administering Guttalax in doses greatly exceeding recommended ones for routine treatment of constipation. [37, 38]
Guttalax, like other laxatives, in case of a chronic overdose may cause chronic diarrhea, abdominal pain, hypokalemia, secondary hyperaldosteronism, urolithiasis. Due to the chronic laxative abuse renal tubular damage, metabolic alkalosis and muscle weakness associated with hypokalemia may develop. [39, 40, 41]
As a laxative in the following cases:
During the II and III trimester of pregnancy (the same is true about other laxatives) the drug can only be prescribed by a doctor. Active metabolite and its glucuronides are not excreted in breast milk. Thus, the drug can be used during breastfeeding.
Treatment: to reduce the absorption of the drug after ingestion one can induce vomiting or perform gastric lavage. Fluid replacement and correction of electrolyte balance may be required, as well as prescription of antispasmodics. It is not recommended to take the drug every day without consulting a doctor for more than 10 days. Long term administration of the drug in high doses can lead to dehydration, electrolyte imbalance, hypokalemia.
In case of simultaneous use of Guttalax in high doses and diuretics or GC the risk of electrolyte imbalance (hypokalemia) is increased. Simultaneous administration of antibiotics may reduce the laxative effect of Guttalax. Electrolyte imbalance may increase sensitivity to cardiac glycosides. Data on reliable and well-controlled studies in pregnant women are not available. Long experience in the application did not reveal any adverse effects of the drug on pregnancy. Taking the drug in the I trimester of pregnancy is contraindicated. Studies on the effect of the drug on fertility have not been conducted. Preclinical studies did not reveal any teratogenic effects on reproduction.
Conclusion
I am proposing to use Naphazoline Nitrate, Guttalax and Dulcolax to treat Carcinogenesis of the Human’s internal, endogenous organs caused by Sonic Weapons through the release and cleaning of the Lymphatic ways in patients with colorectal, colon, pancreatic, breast, etc., cancer. I have proved this healing effect of the Naphazoline nitrate on Myself during treatment in last months of the year 2018. Naphazoline Nitrate, Bisacodyl and Guttalax are clearing the Pylorus in human digestive system and treat so the Microwave Sonic Effects.
Acknowledgments
The author gratefully acknowledge the assistance of Dr. Marta Ballova, Ing. Konrad Balla, Livuska Ballova and Ing. Jozef Balla.
1. Lechien JR, Chiesa-Estomba CM, De Siati DR, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Otorhinolaryngol. 2020. https://doi.org/10.1007/s00405-020-05965-1 [Epub ahead of print]. [Crossref], [Web of Science ®], [Google Scholar]
2. Li Y-C, Bai W-Z, Hashikawa T. The neuroinvasive potential of SARS‐CoV2 may play a role in the respiratory failure of COVID‐19 patients. J Med Virol. 2020;92(6):552–555. [Crossref], [PubMed], [Web of Science ®], [Google Scholar]
3. WöLfel VM, Corman W, Guggemos M, et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020. [Epub ahead of print] [Crossref], [PubMed], [Web of Science ®], [Google Scholar]
4. van Riel D, Verdijk R, Kuiken T. The olfactory nerve: a shortcut for influenza and other viral diseases into the central nervous system. J Pathol. 2015;235(2):277–287. [Crossref], [PubMed], [Web of Science ®], [Google Scholar]
5. Doobay MF, Talman LS, Obr TD, et al. Differential expression of neuronal ACE2 in transgenic mice with overexpression of the brain renin-angiotensin system. Am J Physiol Regul Integr Comp Physiol. 2007;292(1):R373–81. [Crossref], [PubMed], [Web of Science ®], [Google Scholar]
6. Netland J, Meyerholz DK, Moore S, et al. Severe acute respiratory syndrome coronavirus infection causes neuronal death in the absence of encephalitis in mice transgenic for human ACE2. J Virol. 2008;82(15):7264–7275. [Crossref], [PubMed], [Web of Science ®], [Google Scholar]
7. Lochhead JJ, Thorne RG. Intranasal delivery of biologics to the central nervous system. Adv Drug Deliv Rev. 2012;64(7):614–628. [Crossref], [PubMed], [Web of Science ®], [Google Scholar]
8. Chang RB, Strochlic DE, Williams EK, et al. Vagal sensory neuron subtypes that differentially control breathing. Cell. 2015;161(3):622–633. [Crossref], [PubMed], [Web of
Science ®], [Google Scholar]
9. Neumann B, Schulte-Mattler W, Brix S, et al. Autonomic and peripheral nervous system function in acute tick-borne encephalitis. Brain Behav. 2016;6(8):e00485. [Crossref], [PubMed], [Web of Science ®], [Google Scholar]
10. Mazzone SB, Undem BJ. Vagal afferent innervation of the airways in health and disease. Physiol Rev. 2016;96(3):975–1024. [Crossref], [PubMed], [Web of Science ®], [Google Scholar]
11. Matthay MA, Zemans RL, Zimmerman GA, et al. Acute respiratory distress syndrome. Nat Rev Dis Primers. 2019;5(1):18. [Crossref], [PubMed], [Google Scholar]
12. Knudsen L, Ochs M. The micromechanics of lung alveoli: structure and function of surfactant and tissue components. Histochem Cell Biol. 2018;150(6):661–676. [Crossref], [PubMed], [Web of Science ®], [Google Scholar]
13. Ziegler C, Allon SJ, Nyquist SK, et al. SARS-CoV-2 Receptor ACE2 is an Interferon-Stimulated Gene in Human Airway Epithelial Cells and Is Enriched in Specific Cell Subsets Across Tissues. Cell. 2020. [Crossref], [PubMed], [Google Scholar]
14. Sungnak W, HCA Lung Biological Network, Huang N, Becavin C, et al. SARS-CoV-2 entry genes are most highly expressed in nasal goblet and ciliated cells within human airways. Nat Med. 2020;26(5):681–687. [Crossref], [PubMed], [Web of Science ®], [Google Scholar]
15. Brann D, Tsukahara T, Weinreb C, et al. Non-neural expression of SARS-CoV-2 entry genes in the olfactory epithelium suggests mechanisms underlying anosmia in COVID-19 patients. bioRxiv. 2020. [Google Scholar]
16. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. [Crossref], [PubMed], [Web of Science ®], [Google Scholar]
17. Goh KJ, Choong MC, Cheong EH, et al. Rapid progression to acute respiratory distress syndrome: review of current understanding of critical illness from COVID-19 infection. Ann Acad Med Singapore. 2020;49:1–9. [Web of Science ®], [Google Scholar]
18. Herridge MS, Canadian Critical Care Trials Group, Cheung AM, Tansey CM, et al. One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med. 2003;348(8):683–693. [Crossref], [PubMed], [Web of Science ®], [Google Scholar]
19. Moldofsky H, Patcai J. Chronic widespread musculoskeletal pain, fatigue, depression and disordered sleep in chronic post-SARS syndrome; a case-controlled study. BMC Neurol. 2011;11:37. [Crossref], [PubMed], [Web of Science ®], [Google Scholar]
20. Pavlov VA, Tracey KJ. Neural circuitry and immunity. Immunol Res. 2015;63(1-3):38–57. Review. [Crossref], [PubMed], [Web of Science ®], [Google Scholar]
21. Myers, More Americans Evacuated From Chins Over Mysterious Ailments, N.Y. Times (June 30, 2018). See also previous posts to dwkcommentaries.com: U.S. Establishes Task Force To Coordinate Response to Health Problems of U.S. Diplomats in Cuba and China (June 5, 2018); Comment: More U.S. Diplomats Report Illness in China (June 6, 2018);Comment: China Pledges to Investigate Sonic Attacks on U.S. Diplomats (June 7, 2018); Comment: U.S. Broadens Health Alert to All Americans in China (June 8, 2018).
22. See posts to dwkcommentaries.com listed in the “U.S. Diplomats Medical Problems in Cuba, 2017-18” section of List of Posts to dwkcommentaries—Topical: CUBA.
23. U.S. Embassy & Consulates in China, Secretary Pompeo’s Call with Chinese State Councilor and Foreign Minister Wang Yi (June 28, 2018).
24. Skopec R: “Darwinian Selection Transforms Organisms to Bio-Robots“, World Journal of Biology and Medical Sciences, 2018.
25. Z – Skopec – Darwinian selection – 57-77- 16.5.2018
26. Skopec R: “Science Has a Solution for Sonic Weapons Caused Cancer“, Research Trends in Hematology and Oncology, 2018. – Z – Skopec – RTHO – 101 – 6.6.2018
27. ERA GLONASS is the modern Russian system of emergency response, similar to the European standard eCall/E112. The system is designed for use with the Russian global satellite navigation system GLONASS.
28. Nappi G, Perrotta A, Rossi P, et al. : Chronic daily headache. Expert Rev Neurother. 2008;8(3):361–84 10.1586/14737175.8.3.361 [PubMed] [CrossRef]
29. International Classification of Disorders, Committee of the International Headache Society. Classification and diagnosis criteria for headache disorders, cranial neuralgia and facial pain. Cephalalgia. 2004;24(Suppl 1):1–150 Reference Source
30. .Johnson DA, Hricik JG: The pharmacology of alpha-adrenergic decongestants.Pharmacotherapy. 1993;13(6 Pt 2):110S–115S- 143S-146S. 10.1002/j.1875-114.1993.tb02779.x [PubMed] [CrossRef]
31. Willems EW, Valdivia LF, Villalón CM, et al. : Possible role of alpha-adrenoceptor subtypes in acute migraine therapy. Chephalalgia. 2003;23(4):245–257 10.1046/j.1468-2982.2003.00547.x [PubMed] [CrossRef]
32. Munaron L: Shuffling the cards in signal transduction:
Calcium, arachidonic acid and mechanosensitivity. World J Biol Chem. 2011;2(4):59–66 10.4331/wjbc.v2.i4.59
[PMC free article] [PubMed] [CrossRef]
33. Romero TR, de Castro Perez A, de Francischi JN, et al. : Probable involvement of alpha(2C)-adrenoceptor subtype and endogenous opioid peptides in the peripheral antinociceptive effect induced by xylazine. Eur J Pharmacol. 2009;608(1–3):10.1016/j.ejphar.2009.02.019 [PubMed] [CrossRef]
34. Wexner, S. D.; Beck, D. E.; Baron, T. H.; Fanelli, R. D.; Hyman, N.; Shen, B.;Wasco, K. E.; American Society of Colon and Rectal Surgeons; American Society for Gastrointestinal Endoscopy; Society of American Gastrointestinal and Endoscopic Surgeons (2006). Gastrointestinal Endoscopy. 63 (7): 894–909. doi:10.1016/j.gie.2006.03.918.
35. Wald, A (January 2016). "Constipation: Advances in Diagnosis and Treatment"JAMA (Review). 315 (2): 185–91. doi:10.1001/jama.2015.16994.
36. Stiens SA; Luttrel W; Binard JE (November 1998). "Polyethylene glycol versus vegetable oil based bisacodyl suppositories to initiate side-lying bowel care: a clinical trial in persons with spinal cord injury". Spinal Cord. 36 (11): 777–81. doi:10.1038/sj.sc.3100702.
37. Evans, I. Lynn, , Gut, British Medical Journal, 1964, 5, 271 "Medicine: Cut Out the Liver". Time. 1951-04-16. Retrieved 2010-04-26.
38. Robert Engelhorn, Ernst Seeger and Jan H. Zwaving "Laxatives" in Ullmann's Encyclopedia of Industrial Chemistry, Wiley-VCH, Weinheim, 2000.b doi:10.1002/14356007.a15_183