Clinical Psychology and Mental Health Care
OPEN ACCESS | Volume 7 - Issue 1 - 2025
ISSN No: 2994-0184 | Journal DOI: 10.61148/2994-0184/CPMHC
Akm Monjurul Hoque1*, Somaya Buckus2, Maariyah Hoque3, ABM Mahbub ul Alam4, Nisha Singh5, ME Hoque6
1Medical Manager, KwaDabeka Community Health Centre 21 Pitlochry Road, Westville 3629, South Africa.
2Medical Officer, KwaDabeka Community Health Centre.
3Psychology, South African College of Applied Psychology.
4Associate Professor, National Institute of Kidney Diseases and Urology, Dhaka, Bangladesh.
5School of Life Sciences, University of Kwa-Zulu Natal Durban, South Africa.
6Senior Research Associate, Management College of Southern Africa Durban, South Africa.
*Corresponding Author: Akm Monjurul Hoque, Medical Manager, KwaDabeka Community Health Centre 21 Pitlochry Road, Westville 3629, South Africa.
Received: July 02, 2021
Accepted: July 14, 2021
Published: July 16, 2021
Citation: Akm Monjurul Hoque, Somaya Buckus, Maariyah Hoque, ABM Mahbub ul Alam, Nisha Singh et al “Psychological Impact of Covid-19 on Out-Patients Attending A Primary Health Care Facility Durban, South Africa”. Clinical Psychology and Mental Health Care, 3(1); DOI: http;//doi.org/03.2021/1.10039.
Copyright: © 2021 Akm Monjurul Hoque. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
Aim: To determine the psychological impact of COVID-19 epidemic among out-patient attending KwaDebeka Community Health Centre, Durban, South Africa.
Materials and Methods: Self-administered questionnaire-based cross-sectional study design was adapted to out-patient attendees of KwaDebeka Community Health centre, Durban, South Africa. Binary logistic regression analysis was carried out to determine the significant predictors for anxiety, depression and overall psychological problem.
Results: Only 10% had anxiety disorder, 43% had depression disorders and 26% had overall psychological problems. Multiple logistic analysis showed that respondents ages (38 to 47 years) were 51% less likely to to have anxiety disorder (p<0.05), respondents were regularly performing > 150 minutes physical exercise per week were 63% less likely to have anxiety disorder (p<0.05). On the other hand, respondents did not have funding during the epidemic were 2.5 time more likely to have anxiety disorder (p<0.05). Respondents not living with pregnant women in the household were 60% less likely to have depression disorder (OR=0.396, 95% CI 0.221 to 0.709, P< 0.05) and respondents having sufficient funding during COVID-19 were 58% less likely to have depression disorder (OR=0.42, 95% CI 0.224 to 0.484, P<0.05). Respondents having highest level of education were found with 35% less likely to have overall psychological problem (p<0.05). Respondents having sufficient funding were 58% less likely to have overall psychological problem (P<0.05).
Conclusion: Higher rates of depression and overall psychological problems were found among black African out-patients of KwaDabeka community. It is therefore imperative that appropriate and timely mental health care supports are provided to avert adverse psychological health outcomes.
Introduction
Coronavirus disease of 2019 known as COVID-19 has emerged as the most pressing global health issue. The virus has spread to almost every country in the world. It is evident that local transmission of SARS-CoV-2 is occurring in most countries (World Health Organization, 2020). Earlier studies have focused on describing the clinical characteristics and outcomes of COVID-19 in the general population, suggesting that the majority of infections cause a mild form of infection (Zhou, Yu, Du et al., 2020). However, older adults and people with comorbidities, including cardiovascular, respiratory diseases and diabetes are at increased risk of severe illness and death, with men potentially at higher risk than women (Wu & McGoogan, 2020; Istituto Superiore di Sanità, 2020). This notion can cause a great amount of fear and anxiety among the older population group (Dubey, Biswas at al., 2020). Prior studies have elucidated to the adverse psychological effects that the pandemic can produce from fear of COVID-19 which is now termed ‘corona phobia’ on the general population (Asmundson & Taylor, 2020). This rapidly rising infectious disease resulted in erratic changes in peoples’ lives leaving the general public alarmed and scared. Previous outbreaks such as MERS and SARS were found with negatively impacted the emotional wellbeing of the general population (Brooks & Webster, 2020).
In absence of vaccination or community immunization and in order to halt the spread of the infection during the peak of the pandemic in March- June 2020, several governments have imposed movement restrictions and social distancing measures. Many countries across the globe have implemented early quarantine measures as the fundamental COVID-19 pandemic control tool (Rubin & Wessely, 2020). A substantial number of the population was and are still restricted to their homes, owing to nationwide lockdowns and home-confinement strategies to prevent or slow transmission of the disease implemented in the majority of the COVID-19 hit countries resulting in a situation of socioeconomic crisis and emotional distress (Rubin & Wessely, 2020; Pulla, 2020; Serafini, Parmigiani, Amerio et al, 2020). Reports from previous outbreaks have showed that psychological impact of quarantine alone can cause irritability, fear of contracting and spreading infection to family members, anger, confusion, frustration, loneliness, denial, anxiety, depression, insomnia, despair, to extreme consequences like suicide (Brooks, Webster, Smith et al., 2020; Robertson, Hershenfield, Grace et al., 2004; Barbisch, Koenig & Shih, 2015; Jeong, Yim, Song et al., 2016; Liu, Kakade, Fuller et al., 2012). Imposed mass quarantine was applied on the 26 March 2020 by the nationwide lockdown program in South Africa (SA). The consequences of this lockdown may have economic and psychological impact such as mass hysteria, anxiety and distress which may be attributed to a sense of confinement and loss of self-control. The effect of lockdown and the pandemic may cause dysfunctional emotional consequences not only short-term but over the long-term period as well (Dubey, Biswas, Ghosh et al., 2020). Previous studies have highlighted that the mental and psychological well-being of the general population and vulnerable groups including healthcare workers had been adversely affected (Brooks, Webster, Smith et al., 2020; Sim & Chua, 2004; Wu, Fang, Guan et al., 2009; Maunder, Hunter, Vincent et al., 2003; Hawryluck, Gold, Robinson et al., 2004). According to a study on 1210 Chinese citizens living across 194 cities in China, more than half (53.8%) of the participants reported the adverse psychological impact caused by COVID-19 as being moderate to severe, 16.5% of the participants reported moderate to severe depression, more than a quarter (28.8%) of participants reported moderate and 8.1% severe stress (Wang, Pan, Wan et al., 2020). Three quarter (75.2%) of the study population were worried that their family members will contract COVID-19. The study further showed that in the first two weeks following the outbreak, females were reported to experience a higher degree of the psychological impact of the outbreak, stress, anxiety, and depression than males (Wang, Pan, Wan et al., 2020).
The COVID-19 outbreak has impacted significantly on the general population of SA as there is a total of 715 411 cases and 17 863 deaths due to COVID-19 as of 12 October 2020 (Department of Health, 2020). The National government of South Africa has taken commendable interventions as address measures against the COVID-19 pandemic based on the WHO recommendations. In addition to lockdown and home quarantine, SA has also engaged in media campaigns to disseminate information on preventive measures to the general population including pregnant women, health care workers as has been done in other countries; regular hand washing with water and soap, social distancing, covering the hand and mouth while coughing and avoid touching the eyes, nose and mouth initiative (World Health Organisation, 2020).
However, to our knowledge, studies that investigate the psychological problems surrounding COVID-19 are lacking. The study aimed to determine the prevalence and degree of self-reported psychological symptoms and identify demographic, environmental, and individual risk factors.
We hypothesized that national lock-down measures, along with the current COVID-19 epidemic, will have a significant effect on psychological well-being of the black population of SA. We also anticipated that factors, such as demographic, living conditions, and financial concerns, would be significant predictors of psychological and mental well-being. Therefore, the aim of the present study was to determine the prevalence and degree of anxiety, depression and the overall psychological impact inflicted by COVID-19 on the outpatients attending a primary health care setting in South Africa.
Method and Materials
Study design: A descriptive cross-sectional study was conducted among adults attending KwaDabeka Community Health Center (KCHC), a primary health care (PHC) facility in Durban, KwaZulu-Natal Province (KZN) at the initial phase of the COVID-19 epidemic in SA. This report was a part of a comprehensively study that assessed: 1) knowledge, attitude and practices (KAP) of the participants, 2) willingness to accept the COVID-19 vaccine and 3) psychological problems. The survey settings, sample size, sample selection, data collection is reported elsewhere (Hoque, Buckus, Hoque et al., 2020).
Data collection and measurements
Data were collected using a questionnaire composed of i) demographic and personal risk factors, ii) KAP questions iii) acceptance of COVID-19 vaccine and iv) psychological problems of the respondents. The following demographic data were collected: age, gender, education, employment and marital status. Regarding personal and medical risk factors, the following information were gathered: physical exercise of minimum 150 minutes per week, smoke 10 or more cigarettes per day for one or more years, drink more than 14 units of alcohol per week (equivalent to six pints of beer or six glasses of wine), and known vulnerable medical co-morbidity) (WHO, 2020; Department of Health, 2016). We also collected household (HH) risk factors such as number of people living in a HH, respondent living with children under 5 years, respondent living with elders of > 60 years and pregnant women, whether the HH had adequate funding for daily living before and during the epidemic were obtained.
The Generalized Anxiety Disorder-7 (GAD-7) for anxiety symptoms and the Patient Health Questionnaire-9 (PHQ-9 items) for depression symptoms were used in the study to measure anxiety and depression respectively (Spitzer, Kroenke, Williams et al., 2006; He, Li, Qian et al., 2010; Que, Le Shi, Liu et al., 2020 ). Both questionnaires were designed and have been validated in the general population and in primary care settings (Löwe, Decker, Müller et al., 2008; Kroenke, Spitzer & Williams, 2001; Spitzer, Kroenke & Williams, 2001; Löwe, Kroenke, Herzog et al., 2004; Spitzer, Kroenke, Williams et al., 2006). Responses to each of the questions had 4 options: “not at all,” “several days,” “more than half of the days,” and “nearly every day,” coded as 0, 1, 2, and 3, respectively for all questions to measure anxiety, depression and overall psychological problems. Following the analysis of the responses, those respondents who were identified to be experiencing anxiety and, or, depression problems were referred to the social workers' clinic for intervention.
Data analysis
Microsoft excel was used to capture and code and SPSS (version 22.0) was used to analyse data. Descriptive statistics such as means with standard deviation (SD) for continuous variables and frequency distribution for categorical variables were determined. The prevalence of anxiety, depression and overall psychological problems of respondents were also determined. The total score of anxiety was divided into 0–4 normal, 5–9 mild anxiety, 10–14 moderate anxiety 15–21 severe anxiety (Moghanibashi-Mansourieh, 2020).
The Patient Health Questionnaire (PHQ-9) comprising a 9-item depression scale based on the diagnostic criteria of DSM IV. The PHQ-9 has a dual purpose to establish provisional depressive disorder diagnoses as well as to grade depressive symptom severity. The PHQ-9 score ranges from 0 to 27. PHQ-9 shows adequate reliability and convergent/discriminant validity (Titov, Dear, McMillan et al., 2011). The suggested cut off points for mild, moderate, moderate, and severe depression were 5, 10, 15, and 20, respectively (Kroenke, Spitzer, Williams et al., 2001).
The diagnostic threshold of the GAD-7 being 10 and PHQ-9 score ≥10 was previously reported to have a sensitivity of 88% and specificity of 88% for major depression (Löwe, Decker, Müller et al., 2008; Kroenke, Spitzer & Williams, 2001). The combined GAD-7 and PHQ-9 scores > 20 were used to measure the overall psychological problem. Pearson’s correlation test was conducted to determine the relationship between anxiety, depression and overall psychological problems of the respondents. Cross table analysis with Chi-square test was used to identify associated factors for anxiety, depression and overall psychological problem. The GAD-7 (score > 10 =1 and < 9=0), PHQ-9 (scores >10=1 and < 9=0) and overall psychological scores (> 20 = 1 and <19=0) were treated as dichotomous variables for the logistic regression analysis. Binary logistic regression (backward) analysis was undertaken to identify the predictors of demographic vaiables for anxiety, depression and overall psychological problem and reported the results had p values < 0.05. The results are reported as OR (Odds Ratio) with 95% CI. All tests were two-tailed, with a significance level of p < 0.05.
Ethical consideration
Ethical approval was obtained from Umgungundlovu Health Ethics Review Board (Reference no. UHERB 006/2020). Permission from the KCHC management was obtained to undertake the study (reference no. 02/2020). Anonymity and confidentiality of the respondent was maintained at all times. Participation in the study was voluntary. The study obtaied informed consent from the participants after explaining the purpose, nature and objectives of the study.
Results
Table 1: Demographic variable of the respondents.
|
Variables |
Frequency |
Percentage |
|
Gender (n=343) |
|
|
|
Male |
168 |
49 |
|
Female |
175 |
51 |
|
Marital status (n=340) |
|
|
|
Single |
218 |
64.1 |
|
Married |
86 |
25.3 |
|
Others (Living together, widow) |
36 |
10.6 |
|
Age (n=300) |
|
|
|
18 to 27 years |
82 |
23.9 |
|
28 to 37 years |
103 |
30 |
|
38 to 47 years |
58 |
16.9 |
|
>=48 years |
100 |
29.2 |
|
Mean age in years |
39.8 (SD=15.5) |
|
|
Employment Status(n=334) |
|
|
|
Full- time |
99 |
29.6 |
|
Part- time |
49 |
14.7 |
|
Unemployment |
186 |
55.7 |
|
Education level (n=341) |
|
|
|
No education |
17 |
5 |
|
1- 5 years schooling |
29 |
8.5 |
|
6-11 years schooling |
116 |
34 |
|
Matric |
131 |
38.4 |
|
Higher education |
48 |
14.1 |
|
HH with pregnant women (n=344) |
63 |
18.3 |
|
No. of people in the HH (n=343) |
|
|
|
Between 1-3 people |
165 |
48.1 |
|
Between 4-7 people |
133 |
38.8 |
|
> 7 people |
45 |
13.1 |
|
HH with children < 5 years (n=342) |
136 |
39.8 |
|
HH with people > 60 years old (n=342) |
122 |
35.7 |
|
Presence of comorbidity (n= 344) |
186 |
54.1 |
|
Adequate household funding before lockdown (n=339) |
180 |
53.1 |
|
Adequate household funding during lockdown (n=338) |
114 |
33.7 |
|
Usually drink alcohol (n=344) |
59 |
17.2 |
|
Drink alcohol during epidemic/lockdown (n=344) |
9 |
2.8 |
|
Usually smoke tobacco (n=344) |
48 |
14.2 |
|
Smoke tobacco during epidemic/lockdown (n=344) |
33 |
10.5 |
|
Before COVID-19 Exercise > 90 minutes per week (n=285) |
177 |
61. 7 |
|
During Epidemic Exercise > 90 minutes per week (n=287) |
138 |
48.4 |
A total of 345 out-patients participated in the study. There was near equal representation of male (51%) and female respondents (Table 1). The mean age of participants was 40 year with the minimum of 18 and maximum of 65 years. The majority were single (64.1%) and unemployed (55.7%) with low levels of education (only 14.1% had post matric diploma or degree). Most of the HH (52%) were found with > 4 people. Respondents living with vulnerable population like children < 5 years, people > 60 years and pregnant women were found among 40%, 36% and 18% respectively. A higher rate of comorbidity (54.1%) was found with the respondents. Only half (53.1%) of the HH had adequate funding for living before COVID-19 which was reduced to 34% during the COVID-19 pandemic. Among these respondent’s regular alcohol drinker was 17.2% that reduced to 2.8% during the epidemic. The regular smokers were 14% and reduced to 10.5% during the epidemic. Only 40% of the respondents reported that they were undertaking regular physical exercise (> 150 minutes per week).
Prevalence of anxiety, depression and overall psychological problems
The anxiety measures during the COVID-19 pandemic, using the GAD-7, revealed a sample mean score of 5.83 (SD = 3.0). Of all the respondents, 34.8% were found to have a low GAD score (Figure 1) and within the healthy ranges (score: 0–4), the majority (64.2%) had symptoms of anxiety problems (total score > 5). However, half (51.6%) of all respondents were categorised as mild anxiety symptoms or problem (GAD score 5–9), 13.0% moderate (GAD score 10-14) and only 0.6% with severe anxiety symptoms or problem (GAD score 15–21). With regard to the depression symptoms and problems, PHQ-9 revealed a sample mean score of 9.13 (SD = 5.0). Less than a quarter 21.2% of them scored within the normal ranges (total PHQ scores: 0–4 ), 34.8% reported mild (total PHQ score: 5–9), 25.5% moderate (score 10-14) and 18.6% severe depression (PHQ score : 15–27).
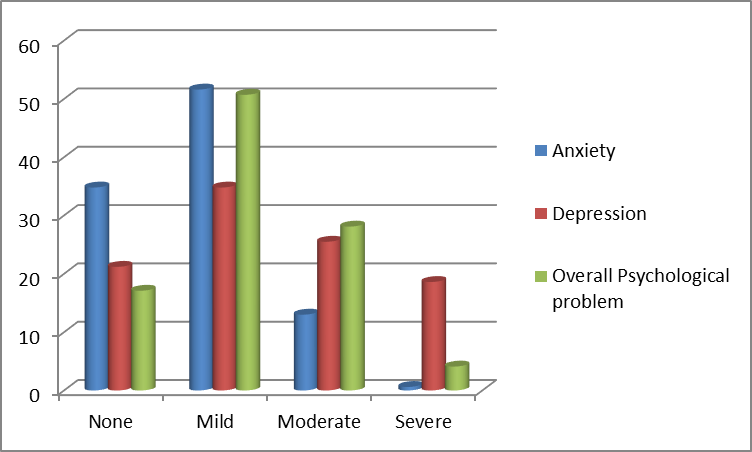
Figure 1: Frequency distribution in percent of anxiety, depression and overall psychological problems of the respondents in percentage.
Combining GAD-7 and PHQ-9 scores, 17.1% of the respondents were found with no (total combined score: 0-9) psychological problem and 82.9% had mild to severe psychological problems. Half (50.7%) of them had mild (total score: 10-28), more than a quarter (28.1%) moderate (total score: 19-28) and 4.1% s had severe (total score > 29) psychological problem. However, considering the GAD-7 and PHQ-9 scores for general population score > 10 was considered to be anxiety and depression disorders and therefore 13.6% and 43.1% respectively were having anxiety and depressive disorders respectively. Using the total scores of anxiety and depression, (score > 29) 32.2% of the respondents were found with overall psychological disorder.
Pearson correlation test (Table 2) was undertaken to establish the correlation between anxiety, depression and overall psychological problem and showed that total anxiety scores were significantly positively correlated with total depression scores (r=0.379; p<0.05) and strongly positively correlated with overall psychological problem (r=0.725 ;p<0.05). Depression scores were significantly strongly correlated to overall psychological problems (r=0.912; p<0.05).
|
|
||||
|
|
Total anxiety |
Total Depression score |
Total Overall Psychological |
|
|
Total anxiety |
Pearson Correlation |
1 |
.379** |
.725** |
|
Sig. (2-tailed) |
|
.000 |
.000 |
|
|
N |
345 |
345 |
345 |
|
|
Total Depression score |
Pearson Correlation |
.379** |
1 |
.912** |
|
Sig. (2-tailed) |
.000 |
|
.000 |
|
|
N |
345 |
345 |
345 |
|
|
Total Overall Psychological scores |
Pearson Correlation |
.725** |
.912** |
1 |
|
Sig. (2-tailed) |
.000 |
.000 |
|
|
|
N |
345 |
345 |
345 |
|
|
**. Correlation is significant at the 0.01 level (2-tailed). |
||||
Table 2: Pearson Correlations of anxiety, depression and overall psychological disorders
Cross table analysis with Pearson Chi-Square test of association was undertaken to identify the demographic variables significantly associated with anxiety, depression, and overall psychological disorders or problems (results not shown). Variables those found significant (p<0.05) were; age, gender, regular drinking of alcohol, undertake regular exercise, respondents living with pregnant women and respondents had adequate fund before and during the COVID-19 epidemic were used in regression analysis to develop models of risk factors separately for anxiety, depression and overall psychological disorder.
Results of regression analysis:
Binay logistic regression analysis was performed to identify demographic, personal and household risk factors those were associated with anxiety (GAD-7 score >10), depression (PHQ-9 score >10) and overall psychological problems (scores >20). On the final step of the logistic analysis (Table 3) age and physical exercise had positive effect on anxiety. Ages (38 to 47 years) were 51% less likely to to have anxiety disorder (OR=0.49, 95% CI: 0.26:0.94, p<0.05) and respondents were regularly performing > 150 minutes physical exercise per week were 63% less likely to have anxiety disorder (OR=0.372; 95% CI .156;.887, p<0.05). On the other hand, respondents did not have funding during the epidemic were 2.5 time more likely to have anxiety disorder (OR= 2.5, 95%CI; 1.3:5.1, p<0.05).
|
|
|||||||||
|
|
B |
S.E. |
Wald |
df |
Sig. |
Exp(B) |
95% C.I.for EXP(B) |
||
|
Lower |
Upper |
||||||||
|
Step 5a |
Age category |
|
|
6.331 |
3 |
.097 |
|
|
|
|
Age category (1) |
-.651 |
.375 |
3.012 |
1 |
.083 |
.522 |
.250 |
1.088 |
|
|
Age category (2) |
-.703 |
.320 |
4.808 |
1 |
.028 |
.495 |
.264 |
.928 |
|
|
Age category (3) |
-.641 |
.371 |
2.988 |
1 |
.084 |
.527 |
.255 |
1.090 |
|
|
Before COVID19 had sufficient funding to cover monthly cost (1) |
-.549 |
.334 |
2.714 |
1 |
.099 |
.577 |
.300 |
1.110 |
|
|
Currently do not have sufficient funding cover monthly cost (1) |
.948 |
.350 |
7.345 |
1 |
.007 |
2.580 |
1.300 |
5.119 |
|
|
perform physical exercise > 150 min per week (1) |
-.988 |
.443 |
4.976 |
1 |
.026 |
.372 |
.156 |
.887 |
|
|
Constant |
-.391 |
.270 |
2.108 |
1 |
.147 |
.676 |
|
|
|
|
Variable(s) entered on step 1: Category Age, Gender, Living with pregnant women, Before COVID19 had sufficient funding to cover monthly cost, Currently had sufficient funding to cover my monthly cost, drink alcohol, perform physical exercise > 150 min per week (1). |
|||||||||
Table 3: Multiple logistic regression analysis output for anxiety disorder
The respondents ages (38 to 47 years) were 53% less likely to to have depression disorder (OR=0.47, 95% CI; 0.24:0.90, p<0.05). The respondents not living with pregnant women in the HH were 60% less likely to have depression disorder (OR=0.396, 95% CI 0.221 to 0.709, P< 0.05) (Table 4). Respondents having sufficient funding during COVID-19 were 58% less likely to have depression disorder (OR=0.42, 95% CI 0.224 to 0.484, P<0.05). Respondents having highest level of education were 35% less likely to have overall psychological problem (Table 5) (OR=0.65, 95% CI; .45:.95, p<0.05). Respondents having sufficient funding were 58% less likely to have overall psychological problem (OR=.42, 95%CI; .18:.99, P<0.05).
|
|
B |
S.E. |
Wald |
df |
Sig. |
Exp(B) |
95% C.I.for EXP(B) |
||
|
Lower |
Upper |
||||||||
|
|
Not Living with children <5 years in HH (1) |
.452 |
.238 |
3.614 |
1 |
.057 |
1.571 |
.986 |
2.503 |
|
Category Age |
|
|
6.122 |
3 |
.106 |
|
|
|
|
|
Category Age (1) |
-.638 |
.392 |
2.654 |
1 |
.103 |
.528 |
.245 |
1.138 |
|
|
Category Age (2) |
-.756 |
.337 |
5.033 |
1 |
.025 |
.470 |
.243 |
.909 |
|
|
Category Age (3) |
-.654 |
.380 |
2.960 |
1 |
.085 |
.520 |
.247 |
1.095 |
|
|
Not Living with pregnant women at home (1) |
-.927 |
.297 |
9.716 |
1 |
.002 |
.396 |
.221 |
.709 |
|
|
Before COVID-19 outbreak had sufficient fund to cover monthly cost |
.582 |
.300 |
3.753 |
1 |
.053 |
1.789 |
.993 |
3.223 |
|
|
Have sufficient funding to cover monthly cost currently |
-.867 |
.320 |
7.327 |
1 |
.007 |
.420 |
.224 |
.787 |
|
|
Constant |
.182 |
.315 |
.334 |
1 |
.563 |
1.200 |
|
|
|
|
a. Variable(s) entered on step 1: Age category, Marital status. Level of education, Living with children < 5 years living in your house (yes/No), HH with pregnant women (yes/no), Before COVID19 outbreak had sufficient funding to cover my monthly cost, Currently I have sufficient funding to cover my monthly cost, Before COVID-19 lockdown On average how many glasses of alcohol do you drink. |
|||||||||
Table 4: Multiple logistic regression analysis output for depression disorder.
|
Variables |
B |
S.E. |
Wald |
df |
Sig. |
Exp(B) |
95% C.I.for EXP(B) |
||
|
Lower |
Upper |
||||||||
|
|
HH with pregnant women |
.560 |
.916 |
.373 |
1 |
.541 |
1.750 |
.291 |
10.543 |
|
Highest level of education |
-.418 |
.187 |
4.988 |
1 |
.026 |
.658 |
.456 |
.950 |
|
|
Employment status |
.018 |
.195 |
.008 |
1 |
.927 |
1.018 |
.694 |
1.493 |
|
|
Before COVID-19 had sufficient fund to cover monthly cost |
.521 |
.402 |
1.684 |
1 |
.194 |
1.684 |
.766 |
3.702 |
|
|
Currently have sufficient fund to cover monthly cost |
-.857 |
.436 |
3.873 |
1 |
.049 |
.424 |
.181 |
.997 |
|
|
BeforetheCOVID19outbreakHowoftendoyouusetobaccocigeratte |
.110 |
.437 |
.063 |
1 |
.801 |
1.116 |
.474 |
2.629 |
|
|
Constant |
.251 |
1.286 |
.038 |
1 |
.845 |
1.285 |
|
|
|
|
a. Variable(s) entered on step 1: Category of age, Gender, Marital status, Living with pregnant women, Highest level of education, BeforetheCOVID-19 outbreak had sufficient funding to cover my monthly cost, Currently I have sufficient funding to cover my monthly cost, Regular alcohol drinker before COVID-19 and now. Before and currently perform physical. |
|||||||||
Table 5: Multiple logistic regression analysis output for overall psychological disorder
Discussion
The findings of the current study contributes to the growing body of knowledge on the mental or psychological health of people during the COVID-19 pandemic in SA. To date this first report from SA represents a sample of homogenous people attending a PHC facility. Similar studies on COVID-19 related psychological effects are conducted on-line and in the developed world. On-line survey are regarded as more appropriate given the nature of the transmission of the pandemic However, for the purpose of this study, face to face in person interviews were conducted due the lack of access to on-line digital technologies by our respondents who are financially poor with low literacy levels. The findings of this study have identified important considerations for public health management and policy development, such as the creation of programs in the wider community to manage the psychosocial problems arising from the pandemic as measures to prevent secondary persistent effects. However, caution in the interpretation of the results is advised, as the respondents in this study were patients who attended the out- patient PHC facility at a clinic. As such all respondents either had acute or chronic medical conditions and were there seeking treatment. Although the respondents of this study were part of the community, the findings apply only to them, and not the community at large.
The demographic indicators of the respondents were as follows: low level of education (only 22% had post matric education), high unemployment rate (52%), not having adequate funding before COVID-19 epidemic (57%) and during the pandemic (only 27.7% had funds) are indicative of a poor socio-economic standing. This translates to a reduction of 35.5% of HH funding which was found among the respondents. In addition, nearly half of the respondents (44%) were living with children less than 5 years (44.5% ) and a quarter of them with adults over 60 years of age, both groups considered vulnerable, and the latter with medical comorbidities (48.3%)
The reduction (83.7%) of regular consumption of alcohol from 17.2% before the epidemic to 2.8% during the epidemic is significant (p<0.05) and was attributed to the national lockdown and the banning of the sale of alcohol and tobaco products in SA during this period. There was a moderate reduction (26%) of smoking from 14.2% to 10.5% of the respondents . This could be regarded as an immediate and positive effect of national regulation. However, due to the illegal trading of cigarettes in this period, the overall result was a minimum reduction of smoking in the respondents (3.7%). Only 40% of the respondents reported that they undertook regular physical exercise (defined as exercise > 150 minutes per week) before the epidemic.
While measures such as the complete lock down and community isolation were deemed necessary and successful in managing the spread of COVID-19 in SA, these measures had widespread negative effects on mental health and well-being as demonstrated by the study findings.The prevalence of anxiety, depression and overall psychological disorders were 13.1%, 44.1% and 32.2% respectively.
Firstly, we found significantly higher rates of anxiety problems. More than half (51.6%) of the respondents were diagnosed with mild anxiety. Importantly, the prevalence of anxiety disorder in the respondents was considered to be similar to findings across the world during the COVID-19 pandemic, where it was estimated to be between 14.6%- 50.9% in countries such as China, Spain, Italy, Iran, the US, Turkey, Nepal, and Denmark (Alari, Hosseinian-Far, Jalali et al., 2020; Jiaqi, Orly, Flora et al., 2020). Furthermore, when compared with a national survey conducted in Cyprus, our findings on anxiety problems was higher than that reported (41% mild anxiety and 23.1% moderate-severe anxiety (anxiety disorder) using the same measurement tool (GAD-7), but on different study populations (Ioulia & Fofi, 2020). The rate of moderate to severe anxiety (13.6%) is comparable to that of the general population in China (8.1%) at the initial stage of the pandemic (Wang, Pan, Wan et al., 2020). This could possibly be linked to the of timing of this study as well, as it was conducted in the early stage of pandemic in SA..
Notably, a higher rate (44.1%) of depression disorder (moderate to severe depression) compared to mild depression (21.2%) was found in the respondents of this study. Similar findings were reported where the range was 14.6% to 48.3% in other countries as stated above/earlier (Jiaqi, Orly, Flora et al., 2020; McCracken, Badinlou, Buhrman et al., 2020). This higher rate of depression disorder is inevitable due to its association with anxiety as a comorbid condition and other compounding socio-economic and environmental factors due to COVID-19 (Choi, Kim, Jeon et al., 2020). It was found that respondents have a low level of education, do not have adequate funding for HH needs, and live with pregnant women (considered a vulnerable group).
The data revealed that respondents beteen the ages of 38 to 47 had a protective effect on anxiety and depression compared to other age groups. Similar to ours, other studies also reported higher levels of anxiety, depression and stress among respondents between 21-40 years of age (Moghanibashi-Mansourieh, 2020; Ahmed, Ahmed, Aibao et al., 2020). It may therefore be assumed that younger people are more likely to be concerned about economic challenges caused by the pandemic, and the associated negatives effects, as they are the key active working forces of the families and communities and thus affected by the conditions due to COVID-19 epidemic. Concomitantly, older people with lower levels of education older population are less likely to involve themself to access to web based information through social media which may have attributed to less stress and depression experienced by them (Jiaqi, Orly, Flora et al., 2020; Cheng, Jun, Liang, 2014).
As the pandemic ramified in SA, concerns regarding health, economy and livelihood increased on a daily basis among the communities. Respondents having or not having sufficient funding during this period is predictive of psychological disorder. In this study, respondents who indicated that they have sufficient funding for household needs during the pandemic were less likely (58%) to have depression and overall psychological disorders. Conversely, respondents not having funding were 2.5 times more likely to experience anxiety disorder. The risk factors associated with financial instability for the development of psychological problems, were highlighted in other studies as well (McCracken, Badinlou, Buhrman et al., 2020). Overall, funding relates to economic activities such as employment, business etc. Unemployment is established as a predictor for anxiety, depression and psychological distress (Jiaqi, Orly, Flora et al., 2020). Our study subjects were largely unemployment and poverty-stricken, thus higher levels of psychological problems are therefore indicated/inevitable.
Strengths and limitations
The associated factors of good or poor psychological health were assessed using bivariate and multivariate logistic regression analysis. These statistical methods are appropriate and best suited for determining associations between dependent and independent variables. However, a limitation is that this was a single centre study which prevents the generalization of the study findings to the study area. We used a small size convenience sample with selective recruitment of respondents. As such, we did not use a random sample, and the distribution of data in our sample cannot be applied as descriptive of all patients in other settings. A multi-centre study would have been ideal. Furthermore, the data were collected cross-sectionally, which restricted the examination of causal relations between the study variables and the levels of anxiety and depression with prospective studies, needed to explore the relationship between the pandemic and anxiety and depression levels. Due to the cross-sectional design used, we are unable to account for or comment on potential changes in psychological status over time.
Conclusion
The impacts of COVID-19 on mental or psychological health in Kwadabeka are comparable to impacts shown from in other studies. The results of this study provide important data on the effects of the COVID-19 outbreak on mental health and identified a variety of personal and social determinants that serve as risk and protective factors. COVID-19 epidemic did not only cause physical health concerns but also resulted in a number of psychological disorders. Thus, it is essential to preserve the mental health of individuals and to develop psychological interventions that can improve the mental health of the general population and vulnerable groups during the COVID-19 pandemic.
Acknowledgement
None
Conflict of interest
The authors declare no conflict of interest
Author Contributions
Conceptualization: AMH, MEH, MH, AMA
Data curation: SB, MH, AMH
Formal analysis: MH, AMH, AMA
Writing and finalizing the manuscript: AMH, AMA, MEH, MH, SB, NS
Funding
No funding was received for this research.