
Olivia Michael Kimario1*, Alex Donasiano1, Cecilia Protas1, Fabian Massaga2 and Oscar Ottoman3
1Department of otorhinolaryngology, Catholic university of health and allied sciences p.0.box 1464 Tanzania.
2Department of General Surgery, Catholic university of health and allied sciences p.o.box 1464 Tanzania.
3Department of pathology , Catholic university of health and allied sciences p.0.box 1464 Tanzania.
*Corresponding Author: Olivia Michael Kimario, Department of otorhinolaryngology, Catholic university of health and allied sciences p.0.box 1464 Tanzania.
Received Date: December 21, 2023
Accepted Date: December 28, 2023
Published Date: January 02, 2024
Citation: Olivia Michael Kimario, Alex Donasiano, Cecilia Protas, Fabian Massaga and Oscar Ottoman. (2024) “Pattern of Head and Neck Malignancies and Associated Factors for Late Diagnosis at Bugando Medical Centre.”, Clinical Case Reports and Clinical Study, 11(1); DOI: 10.61148/2766-8614/JCCRCS/163.
Copyright: © 2024 Olivia Michael Kimario. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Head and neck cancer are among the most common cancers occurring worldwide.It has challenges in management as patient presents at late stage in our environment. This study was done to determine the pattern of head and neck malignancies and associated factors for late diagnosis for patient attending Bugando Medical Center Mwanza Tanzania.
Method: This was analytical cross section prospective study from February to June 2019.
Results: A total number of patient enrolled in the study was 60. The male were more by 1.4%. The median age was 56 years with the range of 12years to 89years. The leading area of head and neck malignancies was oropharyngeal malignant by 30%, followed by laryngeal and sinonasal by 25%, then nasopharyngeal and salivary glands by 8.33%, thyroid malignancies 3.5%, hypopharyngeal 3.33% and others 3.33%.A total number of 35(58.33%) patients were from rural areas and 25(41.67%) were from urban. Majority of the patients used local herb about 42% before been treated at the hospital. Patient did not rush to the hospital as soon as they saw the symptoms therefore they consultation ranged between 1 week to more than 50 weeks from the onset of symptoms. Most patients visited dispensary 25(41%) consulted higher levels of health care for their first time, 14 (31.82%) for hospital level and 11 (25.00%) for health center. From the study, 31patients have 2 referrals, 13 have only one referral and 16 have more than two referrals.
Conclusion: Major cause of delay presentation of head and neck cancer at Bugando Medical Center was attributed by patients themselves whereas health care had small contribution.
Introduction:
Cancers of the upper aerodigestive tract, collectively known as head and neck cancers (HNC), arise from a multiplicity of sites [1,2]. Head and neck cancer includes cancer of upper aerodigestive tract (including oral cavity, oralpharynx, nasopharynx, hypopharynx, larynx) paranasal sinuses and salivary glands [3]. They rank the sixth among the most common cancers worldwide. In 2002, World Health Organization estimated 600000 new cases of Head and Neck Cancer and 300000 death each year worldwide with most common site being oral cavity389000, larynx 160000 and pharynx 65000 [3]. The anatomical site affected have important functions such as speech, swallowing, taste and smell, and therefore the cancers and their treatment may have considerably function saquela which are importance to life [3].
The most important prognostic factor in head and neck cancer is the stage of the disease at presentation. Early cancer has an better prognosis following treatment [4] Therefore, public enlightenment, early diagnosis, and effective cost-effective treatment and follow-up are urgently needed to improve outcomes of these patients in our environment [5] Poverty, illiteracy, advanced stage at presentation, lack of access to health care, and poor treatment infrastructure pose a major challenge in management of these cancers. The annual GDP (gross domestic product) spent on health care is very low in developing countries compared to the developed countries [6]. The number of health care institutions dedicated to cancer care is woefully inadequate when compared with Western countries. [6]
Head and neck cancers are not uncommon at Bugando Medical Centre and show a trend towards a relative young age at diagnosis and the majority of patients present late with advanced stage cancer [5] It is found that, at least one new patient in a week visits Bugando Medical Center with head and neck cancer where majority are at advanced or late stage of the disease. This may be attributed by low education, poverty, delayed diagnosis or wrong treatment at primary health care. This study aims to find out what is the stage of disease at presentation at Bugando medical center and factor that made patient present at that stage.
Literature review:
Head and neck cancer includes cancer of upper aerodigestive tract (including oral cavity, oralpharynx, nasopharynx, hypopharynx, larynx) paranasal sinuses and salivary glands [3] World-wide, the head and neck cancers form the sixth most common cancer and is the most common ca In 2000, head and neck cancer was ranked as the eighth leading cause of cancer death worldwide. Approximately 481,100 new cases developed, and 320,000 persons died of this disease, resulting in an average mortality rate of 7.3 and 3.2 per 100,000 males and females, respectively [8] ncer in developing countries. [6]
In 2020, head and neck cancer (HNC) is expected to affect approximately 833,000 and 151,000 new patients worldwide and in Europe, respectively [12].Cancers are increasingly assuming a critical position as a public health problem in sub Saharan Africa [13] and are often diagnosed late ow Study done in western Uganda in 2016, recruited 51 particitants with SCC of head and neck, From the study, 31patients have 2 numbers of referrals, 13 have only one referral and 16 have more than two referrals these 6 had laryngeal cancer. [15]
HNC affected more males than females, the male to female ratio range from 1:1 to 2.3:1 [16] Occurrence of cancers at various sites in the body differs from one place to another even in the late presentation [13] the same country. Etiological factors associated with cancers vary according to major risk factors in different geographical areas and between genders. As demographic factors change, the pattern of cancers in a place may also change. [16]
In the study done by Mwaikasu et al showed that the commonest observed anatomical location was nasal and paranasal sinuses (23.9%) followed by the larynx (20%). Carcinoma accounted for 94% of head and neck cancers in which squamous cell carcinoma was the most frequent (74%). Lymphoma (2%) was the least frequent histological variant encountered. Nasal and paranasal sinuses had the most histological variations of all anatomical locations of head and neck cancer.
Study done at Kenyatta hospital by Onyango et al showed the larynx was the most common site affected followed by the tongue. In 61% of the cases the size of the tumours at presentation was unknown. [4]
Factors for early or late presentations of HNC:
The majority of the patients attended a public health facility nearest them. For most patients the facility lay within 5 km and could be accessed by walking. However, most of the patients went through multiple referrals to get to KNH. By the time the patients reached KNH, 35 patients (77%) had been treated with unspecified medications, two (4%) had had tooth extraction, and seven (16%) had had biopsies done [4].
Health care professional related factors:
Professional delay is defined as the time from first visit with a health care professional to the developed countries and developing countries [6]. professional delay includes, delay in diagnosis, referral delay, delay in appointment, remote located health care, and histopathology delay [23]
A study done by Onyango at Nairobi enrolling 44 cases of HNC, only two patients attended Kenyatta national hospital as their first visit. Majority attended the hospital as their 3rd or 4th level with average delay of up to 14 weeks, in this study, health professional related was the main cause of patient delay.The time lapse between onset of symptoms and first consultation ranged from zero to nine months, with only 45% of the patients seeking medical care within one month [4]
Study design and setting:
This is an analytical cross sectional prospective study done from February 2019 to June 2019. It was conducted at ENT clinic, wards and Dental clinic.
This includes all patients of all age groups and gender with histological confirmed to have cancer of head and neck attending or admitted at Bugando Medical Centre in the departments of otorhinolaryngology and dental over a period of study.
All patients of all age groups and gender confirmed by histology to have cancer of head and neck attending or admitted in the departments of ENT and Dental at Bugando Medical Centre over a period of study.
Patients who requested and consented for the study. (consent from relative, or patient or legally authorized person). There were 62 patients enrolled, 1 died before consent and excluded from the study, and 1 initially refused then accepted to participate and consented.
Unconscious patients without next of kin to consent for the study.
Patients whom primary tumors couldn’t be assessed.
Unstagable tumors
Metastatic from none head and neck (secondary tumor to the head and neck region)
Patients unable to afford CT scan for completion of staging.
Recruitment of patients to participate in the study was done in the ENT-HNS and dental departments by Principal investigator assisted by research assistants. Patients were screened for inclusion criteria and those who mate the inclusion criteria were enrolled into the study after informed consent to participate in the study.
Clinical staging was done by history taking, physical examination and radiological investigation. Primary tumour size was assessed by physical examination, during routine examination for direct accessible tumours. For those tumours which were not indirectly accessible like laryngeal tumours and nasopharyngeal tumours were assessed using nasopharyngoscopy or during surgery (examination under anaesthesia) for taking biopsy. Lymph nodes size were assessed during routine examination by palpating the regional level of nodes draining the respective area involved. Addition staging were done during radiological evaluation using CT scan X rays and ultrasound. Histopathology was used to confirm the diagnosis of malignancy.
Data were collected using a pre-coded structured questionnaire and were analysed using STATA version 13.0. Data were summarized in form of proportions and frequency tables for categorical variables.
Ethical approval:
Permission was sought from the head of department of Otorhinolaryngology. Patient’s refusal to consent or withdraw from the study didn’t alter or jeopardize their access to medical care. The approval to carry out the study was sought from the Joint CUHAS/BMC Research, Ethics and publication committee.
In this study patients signed a written informed consent for the study. For patient who were unconscious or under the age of 18 years, informant (parent for under 18 years or legally authorized person for those above 18 but unconseous) signed on his/her behalf.
Patients were assured that the information collected were maintained under strict confidentiality.
Results:
Patients’ demographic:
During the period of study, a total number of 61 patients with head and neck malignant were enrolled. One patient was excluded from the study because she died before consenting. So, 60 patients were available for final analysis. Among the 60 patients enrolled, male were 35(58.33%) and female were 25(41.67%) making male: female = 1.4:1. The median 56 years and ranged from 12 years to 89 years. A total number of 35(58.33%) patients were from rural areas and 25(41.67%) were from urban. Primary school education occupied the majority 31(51.67%) of patients, 17(28.33%) had no formal education, 10(16.67%) had secondary education and 2(3.33%) patients were university graduates (table 1).an age was
|
Patients characteristics |
Frequency |
|
Percent (%) |
|
|
Gender |
|
|
|
|
|
Male |
35 |
|
58.33 |
|
|
Female |
25 |
|
42.67 |
|
|
Total |
60 |
|
100 |
|
|
|
|
|
|
|
|
Age group |
|
|
|
|
|
10 - 19 |
2 |
|
3.33 |
|
|
20 - 29 |
3 |
|
5 |
|
|
30 - 39 |
6 |
|
10 |
|
|
40 - 49 |
5 |
|
8.33 |
|
|
50 – 59 |
14 |
|
23.33 |
|
|
60 – 69 |
16 |
|
26.67 |
|
|
70 – 79 |
9 |
|
15 |
|
|
80 - 89 |
5 |
|
8.33 |
|
|
Total |
60 |
|
100 |
|
|
|
|
|
|
|
|
Residence |
|
|
|
|
|
Rural |
35 |
|
58.33 |
|
|
Urban |
25 |
|
41.67 |
|
|
Total |
60 |
|
100 |
|
|
|
|
|
|
|
|
Education level |
|
|
|
|
|
No formal education |
17 |
|
28.33 |
|
|
Primary school |
31 |
|
51.67 |
|
|
Secondary school |
10 |
|
16.67 |
|
|
University |
2 |
|
3.33 |
|
|
Total |
60 |
|
100 |
|
Table 1: Demographical distribution of study population.
Patients related factor in presentation of head and neck cancer:
Patient from rural area presented with late disease stage 29(65.91%) as compared to those from urban area. This may show significant association between rural settlement and late stage presentation of HNC. From the study, large number of patients 42 patients (70%) have used traditional medicine.
cancer.
|
Patient characteristics |
Head and neck cancer stage |
|
p-value |
|||
|
Early stage N % |
Late stage N % |
|
||||
|
Age group |
|
|
|
|
||
|
10 -19 |
1 (6.25) |
1 (6.25) |
|
|
||
|
20 – 29 |
0 (0.00) |
3 (6.82) |
|
|
||
|
30 – 39 |
1 (6.25) |
5 (11.36) |
|
0.860 |
||
|
40 – 49 |
1 (6.25) |
4 (9.09) |
|
|
||
|
50 – 59 |
4 (25.0) |
10 (22.73) |
|
|
||
|
60 – 69 |
6 (37.50) |
10 (22.73) |
|
|
||
|
70 – 79 |
2 (12.50) |
7 (15.91) |
|
|
||
|
80 – 89 |
1 6 (25.0) |
4 (9.09) |
|
|
||
|
|
|
|
|
|
||
|
Area of residence |
|
|
|
|
||
|
Rural |
6 (37.50) |
29 (65.91) |
|
0.048 |
||
|
Urban |
10 (62.50) |
15 (34.1) |
|
|||
|
|
|
|
|
|
||
|
Altenative medicine |
6 (37.50) |
36 (81.82) |
|
0.001 |
||
|
No altenative medicin |
10 (62.50) |
8 (18.18) |
|
|||
|
|
|
|
|
|
||
|
|
||||||
|
Education level |
|
|
|
|
||
|
No formal education |
4 (25) |
13 (29.55) |
|
0.062 |
||
|
Primary school |
6 (37) |
25 (56. 82) |
|
|||
|
Secondary school |
6 (37) |
4 (9.09) |
|
|||
|
University/collage |
0 (00) |
2 (4.55) |
|
|||
|
Total |
16 (100) |
44(100) |
|
|||
|
|
|
|
|
|
||
|
Sex |
|
|
|
|
||
|
Male |
8 (50.00) |
27 (61.36) |
|
0.430 |
||
|
Female |
8 (50.00) |
17 (38.64) |
|
|
||
Table 2: patients associated factors in delay presentations of HNC.
Duration of symptoms before hospital consultation:
Hospital consultation ranged between 1 week to more than 50 weeks from the start of symptoms. Most patients (36) had their first consultation within 4 weeks of symptoms. But one patient delayed up to 2 years before visiting health care while on local medication, Fig 1.
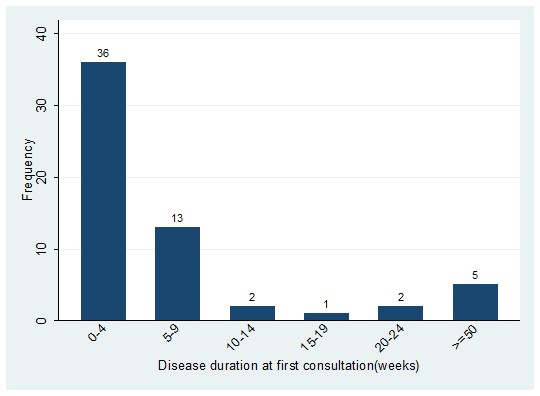
Figure 1: Time taken by patients with symptoms at first consultation.
Health care related factors in delay presentation of head and neck malignant
Most patients visited dispensary 25(41%) as their first health care facility to seek for treatment. This was followed by hospital level which comprised of district hospital, regional hospital and BMC. Patient with first visit to dispensary presented with late stage 19 (43.18%) than those who consulted higher levels of health care for their first time, 14 (31.82%) for hospital level and 11 (25.00%) for health center.
From the study, 31patients have 2 numbers of referrals, 13 have only one referral and 16 have more than two referrals. It shows that, with increase number of referrals, the number of patients presenting with late stage also increases. Table 3 below shows, of the patients with late stage, 22.75% had 1 number of referral, 47.73% had two referrals and 29.55% had more than two referrals. Table 3
|
Health care characteristics |
Stage at presentation |
P-value |
|
|
|
Early stage N (%) |
Late stage N (%) |
|||
|
Level of first health care visited |
|
|||
|
dispensary |
6 (37.50) |
19 (43.18) |
|
|
|
Health center |
5 (31.25) |
11 (25) |
0.876 |
|
|
hospital |
5 (31.25) |
14 (31.82) |
|
|
|
Total |
16 (100) |
44 (100) |
|
|
|
|
|
|
|
|
|
Level of health care patient referred from |
|
|
|
|
Dispensary |
0 (0.00) |
1 (2.27) |
|
|
Health center |
2 (12.50) |
2 (4.55) |
|
|
District hospital |
4 (25.00) |
15 (34.09) |
|
|
Regional hospital |
10 (62.50) |
26 (59.09) |
|
|
Total |
14 (100) |
44 (100) |
|
|
|
|
|
|
|
Number of referrals |
|
|
|
|
1 |
3 (18.75) |
10 (22.75) |
|
|
2 |
10 (62.50) |
21 (47.73) |
0.579 |
|
More than 2 |
3 (18.75) |
13 (29.55) |
|
|
Total |
16 (100) |
44 (100) |
|
Table 3: Health care related in late presentation of head and neck cancer.
Location of primary tumor and stage of disease presentation:
Oropharyngeal area constituted the majority of patients with HNC 18 (30%) and majority of them presented with advanced stage 14 (31.82%) followed by larynx. Contrary to oropharynx, t(31.25%) same as that found in sinonanasal area. Patient with cancer of thyroid, hypopharynx and salivary gland, all presented with advanced stage. Fig 2he larynx constituted large number of patients with early stage of the disease 5.
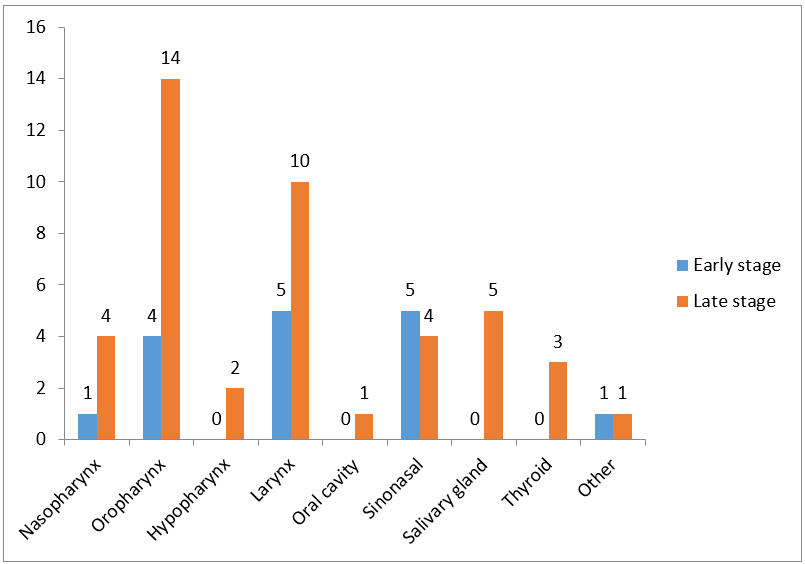
Figure 2: Distribution of primary tumor location.
Discussion:
Head and neck cancers are common cancers occurring at our local environment and its incidence is on rise as time goesby. Currently the trend is changing from old age to young age due to change in life style and viral infection. Majority of patients were presenting with oropharyngeal malignancies followed by the tongue which is difference from the study done at Kennyatta hospital as the laryngeal cancer was leading followed by tongue.Oropharyngeal cancer has increase due to the risk factors that contribute to this especial the oral sex.This matches the same with the study done at Mihimbili about pharyngeal malignancies whereby oral pharyngeal was leading.
In this study the median age at presentation was 56 years. This is keeping with other studies done in Africa and outside Africa (2,5,15). Male were more affected than women with ratio of men : women being 1.4:1.This is the same with other studies(2, 5), however, in this study the ration of male : female was slightly as it shows female are changing as compared to previous and there numbers will soon be high or the same as the males .Nearly two third of patients (73.3%) presented with late stage at diagnosis in our center. This shows that diagnosis of head and neck cancer, is still a challenge as late stage pose a challenge in management, this was found in previous other studies(10, 15). Of the patients presenting with late stage rural residents contributed 65.9% of the patients while urban population contributed 34.1% of all patients with late stage at diagnosis. This has the same result as that done in western Uganda and by Gilyoma et al(5, 15). The late stage at presentation may be due to poor health care facility, lack of professional doctors to diagnose and refer earlier for timely management in rural area which occupy majority of population in this study. Urban area is kept with many hospital with professional specialists that makes more people diagnosed at first visit.
In this study, patients using tradition medicine presented with an advanced (81.82%) stage compared to those not using them who contributed 62.5% of early stage (p value of 0.001), the same trend was seen in a study done in western Uganda(15). During an interview, it was found that, most of patients not using traditional medicine are those Christian who claim to be saved and the majority of this group were those coming from urban area than rural area.
In this study majority of patients had primary level of education followed by those without formal education and few had tertiary education. This keeps with other studies from Kenyatta Hospital and western Uganda(4, 15). Large number of patients with advance disease had no formal education and those with primary level of education by 29.55% and 56.89% respectively (p-value of 0.06). Though the difference in marginal(p=0.06) it could likely be more significant ii large sample size. Patients with secondary school education and university constituted few cases presented with advanced disease. With increasing level of education, the number of advanced cases of head and neck cancer can also be reduced. However, in this study there were only two patients with university education. All patients presented with late stage, one of them was diagnosed at early stage and refused treatment and came back after some time with already advanced stage of the disease.
Duration of symptoms ranged from 1 week to 101 weeks before first health care consultation. This is more similar with other studies done at Kenyatta national hospital, Mbarara Uganda and Muhimbili national hospital where patients delayed to visit health facility within equal interval (4, 5,15). Despite the fact that 60% had first consultation at health care facility within 4 weeks, a large number presented at our centre with advanced stage. This may be due to the majority were treated medically in the peripheral health facilities for wrong diagnosis.
A total of 25 (41%) patients preferred visiting dispensary at their first consultations, likely due to limited access to higher levels and national referral system. The same findings was seen in the study done at Kenyatta hospital(4). For patients who presented with late stage, the majority (43%) were those who visited dispensary at their first consultation. Majority of patients passed through at least one referral to several referrals before coming at BMC. Those who went through one referral and several referrals had no difference in terms of stage presented at our Center(23). This was quite different from the studies done in Kenya and Uganda (4, 15). This may be attributed by those looking for traditional medical care that presented to health care with advanced disease and referred to BMC directly for obvious disease. For those who had many referral, have been treated for none specific symptoms with wrong diagnosis until the disease is advanced. Whether patient first visited dispensary level or hospital level, there were no differences in stage presentation at our center. Large number of patients were referrals from regional hospital level (36), followed by district hospital (19) and health center (4) and only one from dispensary level. The regional hospital has majority of patients presented with early stage (62.5%) as compared to other levels. May this is because patients have to pass through regional hospital (referral hospitals) for being referred to our Center (consultant hospital).
Primary tumor location had different distributions within head and neck regions. The oropharyngel region was the leading (18) followed by larynx (15), sinonasal (9), salivary glands and nasopharynx (5) each. The oropharyngeal tumor has the largest number of patients with late stage. This keeps with other studies or nearly similar in distributions (2, 4,15). This may be explained by the fact that, this sub site has obscured symptoms and when symptoms present, the disease has already advanced. Among patients who presented with early stage, majority (31.25%), had laryngeal cancer. This was the same as that found in western Uganda(15), and likely explanation is fact that, glottis laryngeal symptoms presents early and alert’s them to present early.
Conclusion and recommendations:
Conclusion:
Ethical approval: Informed consent was verbal and was approved by the ethical committee.
Consent for publication:
Availability of data and material: Available anytime needed.
Funding: Not applicable
Acknowledgement:
It is not possible for a single person to cover all aspects that made this article into being and therefore, at the accomplishment of this article, I would like to express my sincere gratitude to all those who helped me to reach this stage.
Competing Interest:
The authors declare no competing.
Authors` contributions
OMK-drafting the manuscript,data collections and discussions
AD-data collection and discussion
CP-discussion of the manuscript and literature
FM- Literature review and discussion
OO-data collection and discussion