Clinical Case Reports and Clinical Study
OPEN ACCESS | Volume 13 - Issue 1 - 2026
ISSN No: 2766-8614 | Journal DOI: 10.61148/2766-8614/JCCRCS
Afsheen Ali1, Sasidharan PK2*
1Junior Resident Department of Medicine, PVS Hospital, Kozhikode, Kerala, India
2Senior Consultant, PVS Hospital & Aster MIMS Kozhikode, Kerala, India
Professor of Medicine and Former Head, Department of Medicine at Government Medical College, Kozhikode
*Corresponding author: Sasidharan PK, Av. Professor of Medicine and Former Head, Department of Medicine at Government Medical College, Kozhikode.
Received Date: November 24, 2021
Accepted Date: December 14, 2021
Published Date: January 06, 2022
Citation: Afsheen Ali, Sasidharan PK, (2022) “Impact of Diet and Lifestyle Modification and Weight Reduction on Essential Hypertension.” Clinical Case Reports and Clinical Study, 6(1); DOI: http;//doi.org/12.2022/1.114.
Copyright: © 2022 Sasidharan PK. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Objectives: This study was to assess the impact of diet and lifestyle modification with weight reduction on blood pressure in patients with essential hypertension and to impart awareness regarding the importance of dietary modifications, physical exercise, and weight reduction in controlling or reversing high blood pressure and prevention of end-organ damage.
Methods: This was a prospective observational study among overweight or obese hypertensives. We included 60 consecutive patients, who after sticking to the diet and lifestyle advice achieved weight reduction. They all were overweight, or had a history of weight gain, and had hypertension, or were newly diagnosed to have persistent hypertension. They were motivated to achieve weight reduction and educated about healthy eating habits using diet charts and tips for lifestyle modifications. Sixty such consecutive subjects, without any secondary causes for hypertension, and who complied with the diet and lifestyle advised, and thus achieved weight reduction only were subjected to statistical analysis. Those who did not achieve weight reduction were not taken for analysis
Results: 90 % of the subjects had their BMI above normal and the remaining 10% of subjects had an upper range of normal BMI, but all of them gave a history of weight gain. The majority of the subjects were having faulty dietary habits with increased carbohydrate intake as the primary reason for weight gain, besides having inadequate vegetables, fruits and protein intake, along with 15% consuming junk food on a daily basis. After lifestyle intervention, weight reduction was achieved in all the subjects studied, and there was a significant reduction in both systolic and diastolic blood pressures with the weight loss achieved, and it was statistically significant. The association of decrease in SBP with a decrease in weight was significant with a p-value of <0.001. The mean initial systolic blood pressure was 154.13 mmHg (SD 13.31), and the follow up mean was 137.33 mmHg (SD 12.87). The mean decrease in SBP was 16.8mmHg, and the mean change in weight was 9.4 Kg. Most of the hypertensives had their drug number or dose decreased and some of them had their drugs stopped completely.
Conclusions: Educating the subjects on balanced diet with restriction of carbohydrates with increased intake of vegetables, adequate fruits, ensuring adequate protein and adequate water intake was the key intervention. The results of the study strongly pointed towards the inevitable role diet, lifestyle and weight reduction had on the achievement of blood pressure control and even reversal of hypertension. Faulty dietary habits with excessive calorie intake, decreased vegetables and fruits, low physical activity and sedentary nature of work contributed to weight gain. Both systolic and diastolic BP decreased on weight reduction implying thereby weight gain as the primary cause for both. Awareness regarding the disease and its complications was very low. In addition, dietary malpractices were detected and halted, and this reinforced the positive results. It also had a favorable impact on the comorbidities they suffered from.
Introduction
Non-communicable diseases have overtaken infectious diseases as the world’s leading cause of mortality and morbidity. Hypertension continues to be a predominant modifiable risk factor for cardiovascular diseases. Globally, an estimated 26% of the world’s population (972 million) has hypertension, and the prevalence is expected to increase to 29% by the year 2025.⁽¹⁾ Lack of a balanced diet, decreased intake of vegetables and fruits, overeating, tobacco and alcohol consumption, physical inactivity, unmanaged stress, and increased salt intake mainly through fast foods, and unchecked consumerism have made hypertension a global epidemic. Because of the commonness of risk factors, hypertension coexists with obesity, fatty liver, dyslipidemia and diabetes mellitus, increasing the risk of complications like ischemic heart disease, stroke, liver and renal failure. Raised blood pressure is a serious warning sign for urgently implementing lifestyle changes. Control of hypertension is often achieved by pharmacological methods, but lifestyle modifications remain the cornerstone in the management. One study before showed high BMI as the single most important modifiable determinant of raised blood pressure⁽²⁾. There is a dearth of studies pertaining to lifestyle interventions in the management of hypertension from this part of the world. The present study was an effort to assess socio-demographic factors associated with hypertension and to highlight and emphasize the importance of patient education on diet and lifestyle modification and weight reduction in the managing hypertension.
Lack of a balanced diet, decreased intake of vegetables and fruits, overeating, tobacco and alcohol consumption, physical inactivity, unmanaged stress, and increased salt intake mainly through fast foods, and unchecked consumerism have made hypertension a global epidemic. Because of the commonness of risk factors, hypertension coexists with obesity, fatty liver, dyslipidemia and diabetes mellitus, increasing the risk of complications like ischemic heart disease, stroke, liver and renal failure. Raised blood pressure is a serious warning sign for urgently implementing lifestyle changes. Control of hypertension is often achieved by pharmacological methods, but lifestyle modifications remain the cornerstone in the management. One study before showed high BMI as the single most important modifiable determinant of raised blood pressure⁽²⁾. There is a dearth of studies pertaining to lifestyle interventions in the management of hypertension from this part of the world. The present study was an effort to assess socio-demographic factors associated with hypertension and to highlight and emphasize the importance of patient education on diet and lifestyle modification and weight reduction in the managing hypertension.
Objectives: 1) To assess the impact of diet and lifestyle modification with weight reduction on blood pressure in patients with essential hypertension. 2) To impart awareness regarding the importance of dietary modifications, physical exercise, and weight reduction in controlling high blood pressure
Materials and methods
We enrolled all consecutive patients with essential hypertension, during the period of January 2019 to June 2020. But included only those who were willing to participate and above the age of 20 to avoid inclusion of secondary hypertension. They were already on treatment for hypertension, or newly diagnosed with persistent hypertension, who were overweight or obese by BMI or gave history of weight gain from their previous normal weight. For our study purpose, the previous normal weight was taken as the lowest recorded weight after completion of skeletal maturity, or the weight at the age of 18 to 20 years when they were healthy and physically active. The final analysis was done on the sixty consecutive patients who were compliant to the strict lifestyle modifications, and had achieved weight reduction (at least 5% of body weight). All cases of secondary hypertension, subjects less than 20 years, pregnant or lactating mothers, those with organ damage, end-stage diseases and those subjects who were non-compliant to lifestyle modification and therefore failing to achieve weight reduction during follow up were excluded from the study. Subjects were informed about the study through an information sheet. An interview method using a semi-structured questionnaire was utilized. The weights of the subjects were assessed using an electronic weighing machine and height with a measuring rod. The baseline blood pressures were recorded using standard electronic BP apparatus and cross-checked with mercury apparatus when needed. The blood pressures were recorded each time with patients seated quietly in a chair with back support, with both feet flat on the floor for at least 5 minutes prior to obtaining a measurement. White coat effect on blood pressure was avoided by adequate precautions at each measurement. A baseline questionnaire was used to collect general information regarding the type of food intake, frequency of fruits, vegetables, and protein intake, salt intake per day, frequency of consuming junk food, salty food, and fried food. Dietary history was taken during the visit using a 24-hour dietary recall method on an average for a week’s period. Information regarding use of alcohol, smoking, other addictions, and their quantity, frequency, and duration of use was noted. Type, duration, and frequency of physical activity and sedentary nature of work were assessed using a physical activity questionnaire. Information regarding the duration of hypertension, antihypertensive drugs and complications if any were collected. Data on other comorbidities like type 2 diabetes, NAFLD, dyslipidemia, and hyperuricemia were collected. Evidence for end-organ damage like retinopathy, stroke, IHD, heart failure, renal dysfunction was assessed. All subjects were evaluated clinically and with necessary investigations to rule out any secondary causes and end-stage diseases or end-organ damage.
All enrolled subjects were given strict dietary advice. A diet plan with a pictorial representation of the proportions and quality of foods they were supposed to take (fig 1) was given for easy understanding. They were primarily advised to consume only half the capacity of their stomach and leave the rest empty on each meal. Calorie rich foods were asked to be reduced to one third to one fourth of what they used to consume or to avoid in entirety till weight reduction was achieved, and to replace them with fiber rich vegetables. They were instructed to restrict eating to a maximum of three times a day and to avoid snacking.
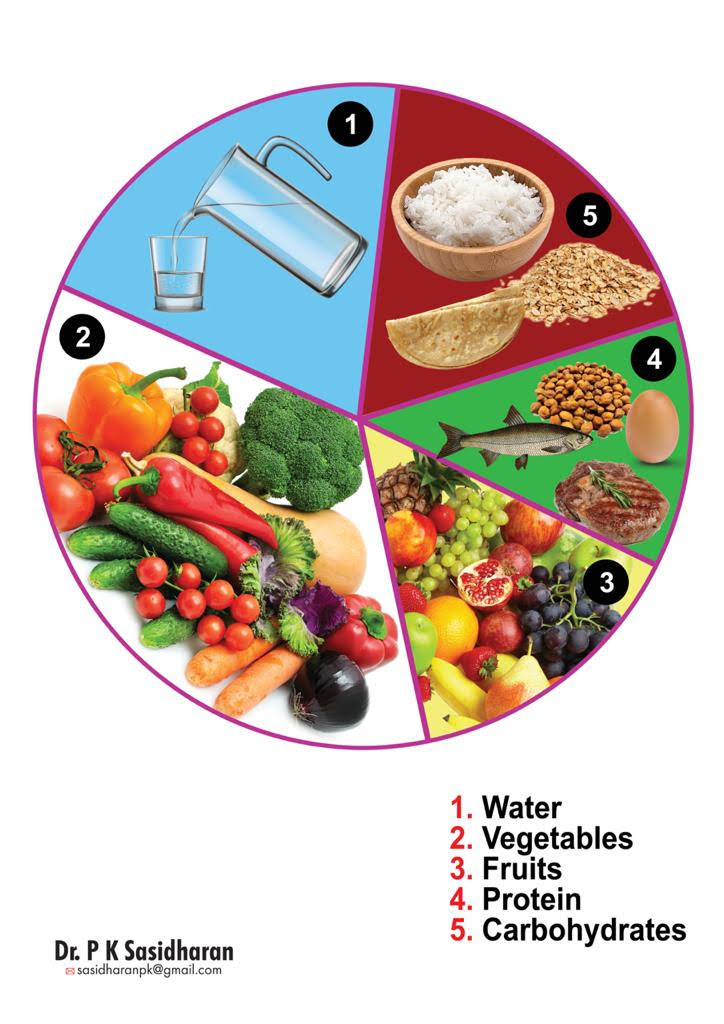
Fig 1

Fig 2
Figure 1 and Figure 2: Diet plan and quantity of food to be taken during each meal, given to each subject (developed by Dr. P.K Sasidharan)3,15
Balanced diet, with each meal containing all five components, were explained in detail (fig1, 2). Advised on liberal intake of high fiber vegetables (raw or steamed, but never overcooked), fresh whole seasonal fruits and adequate safe drinking water, adequate protein (eg: any one of the pulses, yogurt, fish, egg or meat), including one source of calorie (eg: any one cereal) in minimum amounts depending on the caloric requirements. Calorie requirement was modified for each individual depending upon the level of physical activity and their body weight. Protein intake was restricted to 1g/kg/day in three divided meals. The diet was advised in such a way that vegetables would constitute the major proportion of an individual meal (fig 1). They were instructed to reduce salt intake and to increase water consumption sufficient enough to produce 1.5 liters of urine (2-2.5L/day). All participants were given practical tips on modifying their diet at the time of enrollment into the study. Avoidance of all sorts of junk food, fried foods, and salted snacks was reemphasized at each visit. The structured exercises were not easy to accomplish. Hence, any level of exercise that could be incorporated into routine daily activities like avoiding elevators and the use of stairs, walking instead of using automobiles for short commutes, avoiding electrical appliances for household chores etc were advised. In addition, any physical activity requiring a moderate amount of physical exertion was advised to be carried out for at least 30 minutes a day. Levels of stress were assessed by asking questions pertaining to daily life, strain and stress at work, coping with day-to-day problems, marital conflicts and financial strain. Practical tips for stress management like adequate rest, adequate sleep, daily exercise, proper nutrition, meditation, speaking with concerned friends/relatives, were given.
All the subjects were followed up regularly for compliance and were reviewed every month in for blood pressure measurements and weight recording. The weight was monitored with the same weighing machine for easy comparison, and adherence to diet and physical activity was re-emphasized at each visit. Those with highly elevated blood pressures were reviewed weekly till control was achieved. Subjects who were compliant were periodically assessed for their blood pressure and weight loss for a period of at least six months and longer when possible. Only those who finally achieved weight reduction were taken up for analysis of the impact of weight reduction on their high blood pressure. Data were analyzed using SPSS 21.0 and graphs were depicted using Microsoft Excel. Continuous variables were summarized as Mean Standard Deviation or with median. The paired continuous variable was tested using paired t-test. Comparison of continuous variables between two groups was performed using an independent sample t-test. Categorical data were summarized in terms of the frequency with percentage. For all tests, p value <0.05 was considered statistically significant.
Results and discussion
Ninety percent of the enrolled hypertensive subjects had their BMI above normal. Even the 10% of subjects who apparently had normal BMI, gave history of weight gain, or they had put on more weight than their original weight. Interestingly, 31.7% of participants refused any history of weight gain, even when they were obviously overweight or obese. This is just due to the high prevalence of obesity in their surroundings, which makes them fail to notice their weight gain or which led them to believe that being obese meant being healthy, and being lean was equated to lack of health or even poverty. They failed to realize that obesity is another form of malnutrition.
Weight reduction achieved; Majority (46.7%) achieved a weight loss between 6 to 10.9 Kgs. The mean weight before intervention was 72.88 Kg, and after the intervention, it was 63.48 Kg. The average weight loss achieved in the entire group was 9.4 kg. The association was found to be statistically significant with a p value <0.05. The study documented that calorie restriction with decreased carbohydrate intake and increased intake of fiber rich vegetables and fruits, decreased intake of fast foods and junk foods, and moderate levels of physical activity led to significant weight reduction in the study subjects who were compliant. Several of these subjects in the past had tried weight loss strategies including high fat, low carbohydrate diets, and most of them had led to unwanted side effects. Our study supports the importance of a balanced diet and proper motivation in achieving weight reduction in a healthy way.
Change in systolic and diastolic blood pressure after weight reduction and lifestyle changes: We took only those who were compliant and achieved weight reduction for the analysis and observed that there was a significant decrease in blood pressure. Fifty out of the sixty (83.4%) subjects showed a decrease in either systolic blood pressure (SBP) or diastolic blood pressure (DBP) or both. The association of decrease in SBP with a decrease in weight was significant with a p-value of <0.001. The mean initial systolic blood pressure was 154.13 mmHg (SD 13.31), and the follow up mean was 137.33 mmHg (SD 12.87). The mean decrease in SBP was 16.8mmHg, and the mean change in weight was 9.4 Kg. Hence there was approximately 1.78mmHg drop seen per Kg body weight loss. One meta-analysis of 25 studies on this association concluded that a 1-Kg loss of body weight was associated with an approximately 1-mm Hg drop in blood pressure. (4) The better results we got could be due to the overall improvement in the quality of diet and the lifestyle changes. A similar significant association was seen with pre and post intervention diastolic blood pressure (DBP) too. The mean initial DBP was 91.47 mmHg (SD 8.16), and the mean follow up DBP was 83.37 mmHg (SD 8.46). The change in DBP with change in weight was also found to be statistically significant with a p value <0.001. Ten patients (16.6%) only had no significant decrease in SBP or DBP. Still, the minimal weight reduction they had achieved gave added health benefits, in the form of better control of comorbidities like diabetes and dyslipidemia and a general sense of well-being. This was possible due to the improved dietary patterns, increased physical activity, and reduced stress levels.
Change of medications after weight reduction: Before the intervention, 22 patients were on single antihypertensive medicine, 32 were on two or more antihypertensive medications and six were not on any medications. These included CCB, ACE inhibitors, ARBs, beta blockers, and diuretics, either alone or in combination. After intervention, among 19 patients (31.67%) who were on more than one medication, blood pressure control was achieved with the single medicine which was continued at the previous dose. For 9 patients (15%), the dose of their antihypertensives could be reduced. Most significantly, antihypertensive medicines could be stopped in 13 patients (21.67%) and the six (10%) newly detected patients were managed without medicines and they had dropped their blood pressures to normal. There was no change in drug therapy for 15 patients (25%). Even amongst those who had no change in drug therapy, they had better blood pressure controls with the medicines they were already on. When the change in drug therapy and weight loss achieved were compared, a significant association was observed with a p value <0.05. Those who had no change in drug therapy had shed lesser weights when compared to the others. The observations prove that weight reduction achieved with persistent diet and lifestyle changes can reverse or cure hypertension as we had seen in 19 patients (32%), who were either managed without drugs or had their drugs stopped.
There was some association between BMI and initial systolic blood pressure. Four subjects who had their SBP>= 180mmHg had their BMI more than 25 Kg/m2. Previous studies also have suggested the correlation between higher BMI and incidence of hypertension. A higher prevalence of hypertension among overweight/obese prompts an early intervention with diet and lifestyle to achieve weight reduction. (5,6) Higher values of BMI were also associated with diabetes and higher values of liver enzymes (SGPT) in our study, as had been observed earlier. (7) Obesity as a risk factor for NAFLD is well established and has been proved by previous studies. (8)
Physical activity levels: The majority (63.3%) had only low levels of activity and the rest had moderate levels. Only 8 individuals (13.3%) were involved in higher levels of physical activity. Those with higher levels of activity achieved more weight reduction and those with low levels of activity shed lesser kilograms, and this association was statistically significant too. The risk for hypertension decreased with an increasing total volume of physical activity or, there is a direct dose response relationship between physical activity and incident hypertension, as shown in one study before. (9)
Dietary practices: Gross dietary malpractices were noted when meticulous dietary history was taken. Excess carbohydrate intake was associated with higher BMI and higher values of systolic blood pressure, and this association was found to be statistically significant. Carbohydrate intake was excess in 81.67% of the subjects studied. This was attributed to the common wrong notion amongst them that food only meant carbohydrates, and that the vegetables and proteins were side dishes which may or may not be taken according to their likes and dislikes. It is the lack of vegetables in the diet only that led to increased carbohydrate intake for satisfying hunger. Vegetable intake was grossly deficient amongst the subjects with only 8.33% taking it in the required amounts of 2-3 times/day. Mis-concepts of roots and tubers like potato, cassava, tapioca, yam to be vegetables was the predominant cause of deficient consumption even amongst those who claimed to consume them. To be vegetarian meant avoiding fish, meat and egg amongst most, as many of the so-called vegetarians were not taking true vegetables in the required amounts. Undue fear of pesticides and insecticides had aggravated the problem. Fruits were considered only as a snack by most and were not recognized to be an indispensable component of food. Only a miniscule proportion of 3.33% were taking fruits 2-3 times per day. The fear of fruits worsening blood sugar control was another reason for not taking fruits among those who had coexisting diabetes. Whereas among those who had renal dysfunction, it was the fear of increase in potassium levels. In addition, most of them took dry fruits like dry dates instead of fresh fruits, adding on to the excess calories. All these were dealt by patiently convincing each and every patient in relation to their particular illness. Folic acid deficiency as a public health problem arises from these wrong practices. Junk foods, both the traditional homemade ones, as well as chips, chocolates, ice cream, biscuits, sweets and carbonated beverages were being regularly used by many of the subjects. People were unaware of the extra calories from this avoidable snacking habit, as well as about the adverse health effects from the preservatives, artificial colors and flavors. The same people were consuming fried foods as well, which were deep fried in oil. Some of the subjects (15%) were consuming these on a daily basis and even up to 2-3 times a day. One study before proved that a significant association existed between fast food consumption, BP levels, and anthropometric indices. (10) Similarly, the association between frequency of consumption of salted food and initial SBP was found to be statistically significant (p <0.0.5). Those who were consuming it on a daily basis were observed to have higher blood pressures. Studies before have reinforced the beneficial effects of decreasing dietary sodium for blood pressure reduction. (11) In the present study, 48% of the patients were taking proteins inadequately, ie <1gm/Kg/day, whereas 27% were taking them in excess. Knowledge about proteins and their role in a balanced diet were lacking among most of them. Some randomized controlled trials of protein supplementation strongly supported the inverse relationship between dietary protein and blood pressure. (12)
Addictions and Habits: Smoking of cigarettes, beedis and alcoholism were the main addictions seen among the subjects. Many of them (43.3%) were either active smokers or had a history of smoking and 21.7% individuals had a history of alcohol consumption. Smoking cessation and stopping alcohol intake were strictly advised to the study subjects.
Stress levels: Stress levels were deduced with the help of the PSS -4 scale questionnaire. Almost 18.3% of the subjects experienced high levels of stress and 35% suffered from moderate levels of stress. Despite this high prevalence, only 21.67% were aware of the techniques of stress management and their benefits. Persistent chronic stress translates into uncontrolled hypertension. In our study, those with higher levels of stress had higher initial SBP values and the association was statistically significant. Also, studies have suggested that higher perceived stress over time was associated with an increased risk of developing hypertension and that evaluating stress levels over time and intervening when stress is persistent may reduce hypertension risk. (13)
Comorbidities in the study subjects: Majority of the study group had, in addition to hypertension, diabetes (25%), dyslipidemia (18.3%), and NAFLD (18.3%). Studies have suggested that the coexistence of hypertension among diabetics increases the risk of macro and microvascular complications, and the presence of NAFLD aggravates cardiovascular complications. (14) Change in LDL and FBS with weight reduction were also looked at, and they were also found to be statistically significant.
Literacy and awareness: Even though the majority of the participants were well educated, their awareness regarding the disease and its risk factors were dismal with only 35% being aware of it, which itself is a marginalization. This observation emphasizes the importance of health education at all levels focusing at the PHCs and in the school health programs. Educating the younger generation is of critical importance because eating habits when changed early in life can prevent many lifestyle diseases which are growing exponentially due to faulty eating habits. These observations suggest that there is a dire need of family doctors to impart health education in the population represented by the study subjects.
Conclusions
Significant weight reduction was possible with diet and lifestyle interventions. Both systolic and diastolic BP could be reduced with weight reduction. It was possible to either stop or manage without antihypertensive medications after weight reduction in 19 subjects and could reduce medications in others. Individualized attention and care with persistent motivation are essential in achieving compliance, since all the subjects who were compliant to the lifestyle intervention had achieved weight reduction. The awareness regarding hypertension, its risk factors and complications were seen only in 35% of the subjects, in spite of high literacy rates, indicating the dire need for more awareness. Wrong dietary habits with excess carbohydrates in different forms, with less vegetables and fruits were the major reason for weight gain and the consequent development of hypertension. Physical activity was found to be low, and the majority had comorbidities like type 2 diabetes, NAFLD, dyslipidemia and hyperuricemia, substantiating that the fundamental cause is weight gain/obesity and the consequent insulin resistance. Thus, it could be concluded that weight reduction with diet and lifestyle is the definitive therapy for essential hypertension, and it controls comorbidities, like diabetes, dyslipidemia, and NASH too.
Recommendations: Literacy alone does not equate to awareness about healthy lifestyle practices and social interventions at several levels are needed to bring about the change. There should be improved primary education and a large number of primary care doctors to create awareness on these basic diet and lifestyle practices. All individuals should be made to practice and promote healthy eating and healthy lifestyle with regular exercise to prevent weight gain. Regular recreational or job-related exercises should be made a habit in every individual, especially the hypertensives. Weight reduction is mandatory in all with history of weight gain, including those who have gained a few kilograms more than their original baseline body weight. Focus of management should be on weight reduction rather than hiking antihypertensives, if they are overweight by any criteria. Everyday techniques such as use of steps instead of elevators, cycling to work, avoiding machineries for household chores should be emphasized. Stress reduction by proper counseling on stress management by family doctors and adequate social security measures is inevitable in the management of hypertension. The practice of eating junk food should be cut down to maximum, and leisure eating, eating in front of television should be avoided. All these interventions need good family doctors working as friends, philosophers and guides. Regular check-ups by family doctors and weight recording at every visit should be made mandatory. Health education regarding healthy diet and lifestyle should be imparted regularly in schools and colleges. Doctors should know all about diet and practical tips on diet, and they should give correct advice regarding diet and exercise to every patient and motivate them for the same. Instead of a rigid nutrition prescription, the dietary advice should be flexible and individualized to help the person achieve and maintain therapeutic goals.