Clinical Case Reports and Clinical Study
OPEN ACCESS | Volume 12 - Issue 5 - 2025
ISSN No: 2766-8614 | Journal DOI: 10.61148/2766-8614/JCCRCS
Vishnu Sharma, Arpita Digwal and Vansh Bagrodia3*
1(Hemato-oncology), Associate Professor, SMS Medical College, Jaipur.
2Final year MBBS student at SMS Medical College, Jaipur.
*3Final year MBBS student at SMS Medical College, Jaipur.
*Corresponding Author: Vansh Bagrodia, Final year MBBS student at SMS Medical College, Jaipur.
Received Date : September 09, 2023
Accepted Date: September 18, 2023
Citation: Vishnu Sharma, Arpita Digwal and Vansh Bagrodia.(2023) “Spontaneous Pneumopericardium in a young Patient with Acute Febrile Illness.”, Clinical Case Reports and Clinical Study, 9(5); DOI: 10.61148/2766-8614/JCCRCS/153.
Copyright: © 2023 Vansh Bagrodia. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
We present a case of a male patient in his late thirties who was admitted with high-grade fever, dyspnea, and chest pain. Clinical examination indicated shock, and a chest X-ray revealed pneumopericardium. Despite initial interventions, the patient deteriorated rapidly. While the primary cause remained uncertain, pneumopericardium is typically characterized by air-fluid levels in the pericardial sac. It can arise from various causes and often resolves spontaneously. This case underscores a notable and classical appearance of pneumopericardium on chest X-ray.
Case Presentation:
A male patient in his late thirties presented at our tertiary specialist unit with a five-day history of high-grade fever, worsening dyspnea mMRC (Modified Medical Research Council) grade 4 upon admission, and chest pain. Despite his consciousness, the patient appeared anxious.
Upon examination, several concerning signs were noted: tachypnea (48 breaths/minute), tachycardia (pulse rate - 138 beats/minute), and hypotension (74/52 mmHg). A modified shock index of 2.3 confirmed his state of shock. Room air oxygen saturation stood at 86%. Cardiac examination revealed distended neck veins and muffled heart sounds, along with the classical Hamman’s crunch heard upon auscultation. Systemic examination yielded no remarkable findings, including the absence of hepatomegaly or ascites, and pedal edema was absent. Electrocardiogram (ECG) showed low voltage QRS complexes. Chest X-ray demonstrated abnormal translucency around the cardiac silhouette, indicative of pneumopericardium (figure 1). In response to his hypoxia, he was administered oxygen via a mask at a flow rate of 6 L/min, and other stabilization measures were initiated. Unfortunately, the patient collapsed just two hours after admission, preventing further studies.
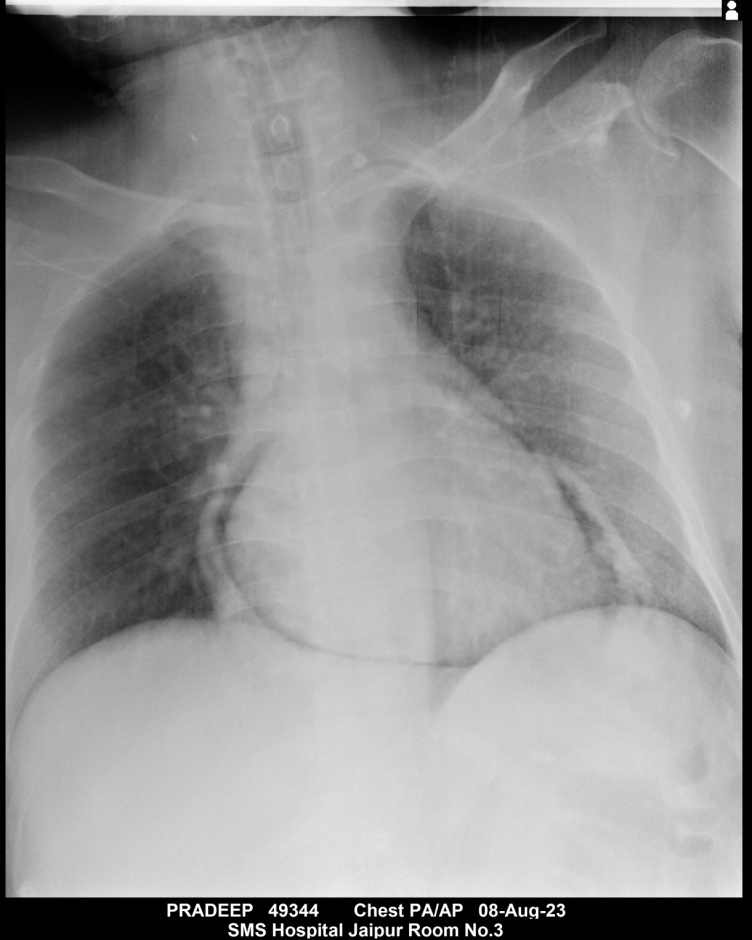
Figure 1: Pneumopericardium seen on Chest X-ray
Although the examination findings strongly suggested cardiac tamponade as the cause of his early demise, the primary underlying cause could not be definitively ascertained. However, the presence of prominent pneumopericardium on the CXR is noteworthy.
Pneumopericardium is a medical condition characterized by the presence of air-fluid levels in the pericardial sac. It is a rare condition that can occur due to various causes, including GI malignancy, asthma, infectious pericarditis, blunt or penetrating trauma, barotrauma, valsalva, thoracic surgery, or other medical procedures [1]. The most common cause is the formation of a fistula between the pericardium and a gas-containing cavity [1,2].
Pneumopericardium typically resolves spontaneously without further management, with monitoring of hemodynamic status and ECG. It can manifest with symptoms or remain asymptomatic. Dyspnea and chest pain are the most commonly reported symptoms. Chest radiographs reveal air-fluid levels in the pericardial sac, while CT scans provide better resolution of air within the pericardial sac [3].
In some cases, complicated pneumopericardium can progress to fatal conditions like cardiac tamponade. In symptomatic cases, physical examination may reveal the classic "Beck’s Triad" - hypotension, elevated JVP, and distant heart sounds, as was observed in our patient and ultimately led to his unfortunate demise [3].
The patient's chest X-ray displayed a classic appearance of pneumopericardium, which, coupled with the history of high-grade fever, chest pain, and dyspnea, points towards a pericardial inflammatory process, possibly pericarditis, as the most likely etiology. While trauma is a common cause of pneumopericardium, either accidental or iatrogenic, the absence of any such history reduces its likelihood [4].
However, the most common overall cause is idiopathic. The etiology of pericarditis can be broadly categorized into infectious and non-infectious causes. Viral infections are the most common cause of infectious etiology [5]. Gas-forming bacteria like Prevotella, Bacteroides, Streptococcus milleri, and Streptococcus viridans have been identified as causative organisms for infectious pericarditis leading to pneumopericardium, as seen in a case report by Carol et al. These findings align with the most likely cause of pneumopericardium in our patient. Unfortunately, conclusive evidence could not be obtained as aspiration and subsequent culture studies could not be conducted due to the patient's rapid deterioration [6].