Clinical Case Reports and Clinical Study
OPEN ACCESS | Volume 13 - Issue 1 - 2026
ISSN No: 2766-8614 | Journal DOI: 10.61148/2766-8614/JCCRCS
Jyoti Burad1*, Sonali Kodange1, Saba Al Wardi1, Tarun Sharma1, Fatema Al Lawati1, Arwa Al Fahdhi1, Jamal Al Aghbari1, Saif Al Mubaihsi1, Sachin Jose2
1Department of Anesthesia and Intensive Care Sultan Qaboos University Hospital, PO Box 38, PC 123 Muscat Oman.
2Statistics Specialist Research department Oman Medical Specialty Board Muscat, Oman.
*Corresponding Author: Jyoti Burad, Department of Anesthesia and Intensive Care Sultan Qaboos University Hospital, PO Box 38, PC 123 Muscat Oman.
Received Date : August 28, 2023
Accepted Date: September 04, 2023
Published Date: September 08, 2023
Citation: Jyoti Burad, Sonali Kodange, Saba Al Wardi, Tarun Sharma, Fatema Al Lawati, Sachin Jose (2023) “ Review of Barotrauma in Covid-19 Cases; A Retrospective Matched-Case-Control Study.”, Clinical Case Reports and Clinical Study, 9(4); DOI: 10.61148/2766-8614/JCCRCS/151.
Copyright: © 2023 Jyoti Burad. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction:
Barotrauma is associated with Covid-19, increasing its morbidity. A retrospective, matched-case-control study was done to find the incidence of barotrauma and inciting factors in Covid-19 patients.
Material and methods:
A total of 2519 Covid-19 admitted adult patients (>18 years of age) were scanned from March 2020-April 202, and 63 were found to have barotrauma (Cases). Out of these, 188 age and sex- matched controls were selected and studied. A total of 251 Covid-19 patients included 54% males and 46% females. Patients' demography, laboratory details, treatment, and course in the hospital were recorded. Outcomes included Incidence of barotrauma (primary), associated factors, mortality, ventilation days, and length of stay (secondary).
Results:
The mean age of the study population was 58.28 ±16.37. The incidence of barotrauma was 2.9% [95% CI= 2.3% to 3.7%, 63/2159]. Univariate analysis showed the following factors significantly associated with barotrauma: S:F ratio at presentation [P<0.001], positive pressure ventilation (PPV) [P<0.001], and steroids [P=0.003]. The multivariate analysis confirmed the association of the S:F ratio of 100-199 [OR= 2.328, 95% CI 1.006 to 5.389, P= 0.048] and PPV [OR 6.425, 95% CI 2.380 to 17.345, P<0.001]. Higher mortality [66.7% versus 31.4%, P<0.001], ventilation days (median of 9 versus 0 days, P<0.001), and length of stay (median 22 versus 11 days, P<0.001) were noted for cases versus controls.
Conclusions:
The incidence of 2.9% of barotrauma with Covid-19 disease was associated with low oxygenation, PPV, higher mortality, ventilation days, and hospital length of stay.
Introduction:
Covid-19 disease: Covid-19 is a recently emerged disease affecting the respiratory system primarily and later progresses to multisystem involvement. Most of the cases are mild and recover well. [1] However, those who develop moderate to severe symptoms requiring admission were found to have peak radiological findings two weeks after symptom onset. [2] Most of these patients start requiring respiratory support, and complications start to emerge as the inflammation and fibrosis of the lungs worsen. They receive different modalities of respiratory support as per the need and guidelines. [3] Bacterial superinfections, interleukin surge, and septic shock are common. Recently, rising episodes of barotrauma with Covid-19 have been observed. In the covid era, the hospital and ICU beds with respiratory and monitoring resources became scarce because of vast admissions. [4]
Mechanisms of barotrauma in Covid-19 cases can be many. Positive pressure ventilation (PPV) can lead to alveolar overdistension, a decrease in the caliber of pulmonary vessels increasing pressure gradient causing air leak to the sheath and Macklin phenomenon (occurrence of a large pressure gradient between marginal alveoli and lung interstitium leading to barotrauma) are few worthy mentions. [5] Barotrauma might lead to setbacks in a patient's recovery. Timely diagnosis and management of barotrauma in Covid-19 disease might lead to better outcomes. This research aimed to determine the incidence of barotrauma and highlight the associated factors and the outcomes.
Methods:
Study design: Ethical approval for this study was obtained from the Medical Research Ethical Committee of our institute on 23rd June 2021. This retrospective, observational, single-center, matched-case-control study was initiated and was registered at Clinicaltrials.gov (NCT05216523). The privacy of patients was respected, and the study procedure followed the protocol approved by medical research ethics committee and the Declaration of Helsinki (1975).
All adult inpatients admitted to ward/High dependency unit/Intensive care unit diagnosed with a covid infection [PCR (Polymerase Chain Reaction) positive] from March 2020-April 2021 at University Hospital in Oman were considered eligible for the study and were scanned. Covid infection was considered as exposure. The investigators collected the details of each patient from electronic patients' records (EPR). The patients were followed from admission till discharge. Those patients who developed barotrauma were labeled as "Cases," and those without barotrauma were "Controls'. The patient files were searched for keywords: pneumothorax/ pneumomediastinum/ pneumopericardium/ subcutaneous emphysema. The diagnosis was reconfirmed by radiological diagnostic modalities such as X-Ray and CT (Computerised Tomography) scan of the chest.
The primary outcome of this study was incidence of barotrauma in hospitalised Covid patients, and the secondary outcomes were the factors associated with barotrauma, mortality, and ventilation days of cases. The predictors were severity of the disease as measured by S:F ratio, CRP, ferritin, and D-dimer levels. Many potential confounders were studied mainly the comorbidities such as diabetes mellitus/chronic kidney disease/hypertension/asthma/ischemic heart disease and steroids. The effect modifier were the PPV - Non-invasive ventilation (NIV)/Invasive mechanical ventilation (IMV). The confirmation of barotrauma was done by X-ray or CT scan of the chest by radiologist report. All pertinent data were collected from the electronic patient record of the hospital information system.
Bias: There were few sources of bias in this study. The cases which were transferred outside the hospital were lost to follow-up and were excluded. Also, this is a single-center study with a limited case mix.
Study size: Since there were no previous studies on covid related barotrauma for sample size determination when this study started, all patients admitted to the hospital with covid infection during the study period were included.
Statistical methods:
Quantitative variables. These variables included length of stay (LOS), ventilation days, age, S:F ratio, levels of D-dimer, CRP (C-Reactive Protein), and ferritin.
Statistical methods: Continuous variables were presented as mean, median, and standard deviation, whereas categorical variables were presented as frequency and percentage. As appropriate, the comparison of means between two groups was assessed using the independent samples t-test or the Mann-Whitney U test. Association between two categorical variables was calculated using an appropriate χ2 test (Likelihood ratio test or Fisher's exact test). The severity of hypoxia was divided into three categories based on the S:F ratio. A multivariate binary logistic regression analysis was applied to determine the independent predictors for the development of barotrauma. The odds ratio and 95% CI were reported for all the predictors. A P-value less than 0.05 was considered statistically significant. All the analysis was carried out using the IBM SPSS statistics version 26.0, and the figures were made using the STATA SE17.
Sub-group analysis was done for Cases with mortality and the highest respiratory support and the severity of hypoxia, steroids, and type of barotrauma. There were missing data for the following: S:F ratio (3 patients), CRP (12 patients), D-dimer (38 patients), ferritin (49 patients), and hospital length of stay (1 patient). Multiple mutations were applied to replace the missing values of the quantitative variables: CRP, D-dimer, and Ferritin. Other missing data were minimal and hence were ignored. The controls were matched with cases for age and gender in a ratio of 3:1, respectively.
Results
Participants: A total of 2159 Covid-19 PCR-positive patients were identified from hospital records during the study period. Out of these, 63 patients developed barotrauma. Age and sex-matched, 188 controls were studied. (Figure 1)
The overall mean age was 58.28(+/-16.37), 46% were females, and 54% were males. Both the groups had similar comorbidities. The group-wise baseline demographics have been detailed in Table 1. The CRP values were not significantly different, but median D-dimer was 1.95(IQR 1- 4.05) versus 1.2(IQR 0.7-3.2) (P=0.049), and median ferritin was 1364(IQR 949-2549), versus 841(IQR 400-1908) (P<0.001) for cases and controls respectively. Most of the cases [56 (89%)] received steroids (either Dexamethasone 6 mg or Dexamethasone 20 and 10 mg or Methylprednisolone regimens) as per the treating physician's discretion, whereas only 129 (69%) of controls received them. (Table1) The ventilation days significantly differed between the two groups. For cases, it was a median of 9 days (IQR 1.5-18), and for controls, it was a median of 0 (IQR 0-6) (P <0.001).
The overall hospital incidence of Barotrauma was found to be 2.9% (95% CI= 2.3% to 3.7%, 63/2159). Mortality was significantly high among the cases as compared to controls (66.7% versus 31.4%, P <0.001) (Figure 2b). There was a significant difference between the two groups for other outcomes: median ventilation days (9 for cases versus 0 for controls, P <0.001) and median length of stay (22 days for cases versus 11 days for controls, P <0.001). (Table 1)
Univariate analysis showed a significant difference between the two groups concerning S:F ratio at presentation (P<0.001) (Figure2c), steroids received (56/63, 89% in cases versus 129/188; 69% in controls; P<0.003), and PPV (56/63, 89% in cases versus 86/188, 46% in controls; P<0.001). (Table2) The multivariate analysis showed that the S:F ratio at admission and PPV are the statistically significant independent predictors of barotrauma among Covid-19 patients. Patients with an S:F ratio of 100 to 199 are two times more likely to develop barotrauma than patients with an S:F ratio more than or equal to 200 (OR= 2.328, 95% CI= 1.006-5.389, P=0.048). Patients who received PPV are six times more likely to develop barotrauma than patients who did not receive PPV (OR= 6.425, 95% CI= 2.380-17.345, P<0.001). Though the variable use of steroids was significant in the unadjusted analysis, it became not significant in the adjusted multivariate analysis. (Table 2) The S:F ratio was categorised into three categories: <100, 100-199, and >200.
Sub-group analysis: Highest respiratory support at the time of barotrauma showed that most cases received PPV (93%), 5% were on FM (face mask), while only 2% had no respiratory support. Amongst the different types of respiratory support received, PPV was associated with the highest mortality (39/63, 62%). A total of 89% received steroids. The appearance of barotrauma was up to 11 days for most of the cases (43/63, 68%) (Figure 2a). Male sex (44/63, 70%) developed more barotrauma than females, P=0.564. Pneumothorax was present in 33/63, 52%, Pneumomediastinum in 38/63, 60%, Surgical emphysema in 32/63, 51%, and Pneumopericardium was present in 6/63, 9.5% of cases (Figure 2d). The association of these variables with mortality in barotrauma cases is reported in Table 3.
Table 1: Characteristics of the Covid PCR positive patients by barotrauma status |
PCR, Polymerase Chain Reaction; DM, Diabetes; HTN, Hypertension; COPD, Chronic Obstructive Pulmonary Disease; S:F, Oxygen saturation/Fraction of inspired oxygen; CRP, C-Reactive Protein; PPV, Positive Pressure Ventilation; NP, Nasal Prong; FM, Face Mask; NIV, Non-invasive Ventilation; IMV, Invasive Mechanical Ventilation.
|
Variable |
Unadjusted Odds Ratio (OR) |
95% CI for unadjusted OR |
P-value |
Adjusted Odds Ratio (OR) |
95% CI for adjusted OR |
P- value |
||
|
Lower |
Upper |
Lower |
Upper |
|||||
|
S:F ratio at admission |
||||||||
|
200-300 (Reference) |
||||||||
|
100-199 |
5.609 |
2.767 |
11.371 |
<0.001 |
2.328 |
1.006 |
5.389 |
0.048 |
|
<100 |
2.833 |
1.296 |
6.193 |
0.009 |
1.005 |
0.404 |
2.498 |
0.992 |
|
Heart Disease |
||||||||
|
Yes |
0.405 |
0.151 |
1.087 |
0.073 |
0.408 |
0.136 |
1.226 |
0.110 |
|
Asthma |
||||||||
|
Yes |
3.193 |
0.991 |
10.288 |
0.052 |
2.750 |
0.690 |
10.956 |
0.152 |
|
Kidney Disease |
||||||||
|
Yes |
0.326 |
0.095 |
1.119 |
0.075 |
0.313 |
0.061 |
1.591 |
0.161 |
|
CRP on admission |
1.002 |
0.999 |
1.005 |
0.178 |
0.998 |
0.995 |
1.002 |
0.320 |
|
D-dimer on admission |
1.009 |
0.986 |
1.033 |
0.452 |
1.005 |
0.977 |
1.035 |
0.707 |
|
Ferritin on Admission |
1.000 |
1.000 |
1.000 |
0.093 |
1.000 |
1.000 |
1.000 |
0.260 |
|
Received steroid |
|
|
|
|
|
|
|
|
|
Yes |
3.659 |
1.573 |
8.509 |
0.003 |
2.411 |
0.853 |
6.814 |
0.097 |
|
PPV Yes |
9.488 |
4.111 |
21.901 |
<0.001 |
6.425 |
2.380 |
17.345 |
<0.001 |
Table 2: Binary logistic regression analysis to determine the independent predictors of barotrauma among Covid PCR positive patients.
S:F, Oxygen saturation/Fraction of inspired oxygen; CRP, C-Reactive Protein; PPV, Positive Pressure Ventilation.
Table 3: Mortality amongst Cases S:F, Oxygen saturation/Fraction of inspired oxygen; FM, Face Mask; NIV, Non-invasive Ventilation; IMV, Invasive Mechanical Ventilation. |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
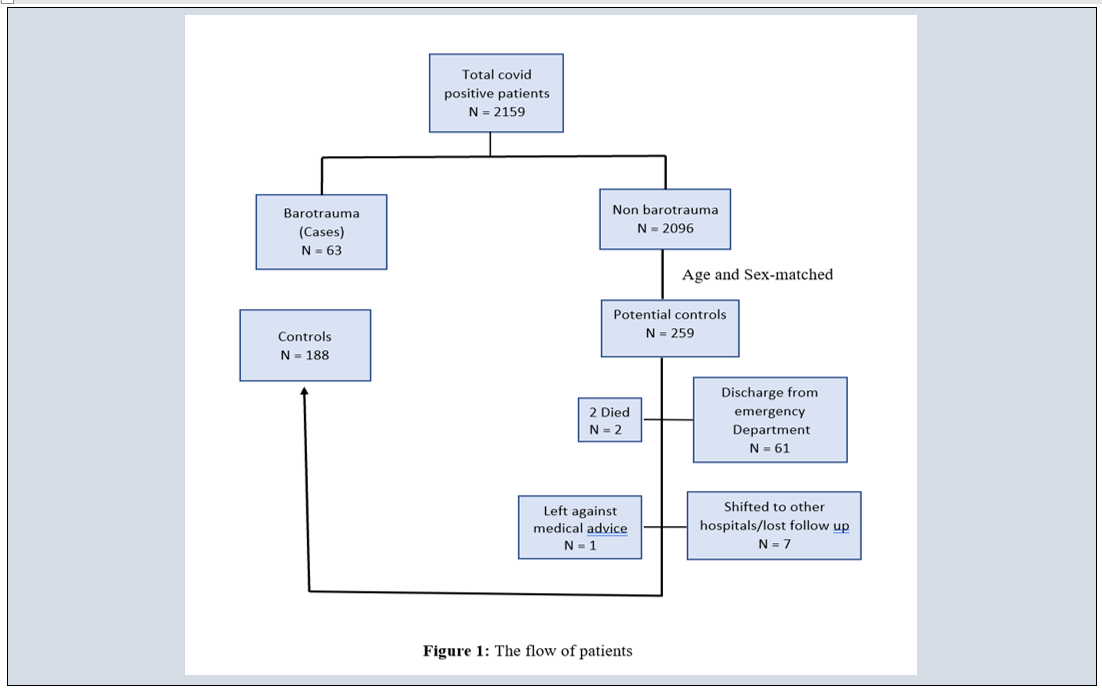
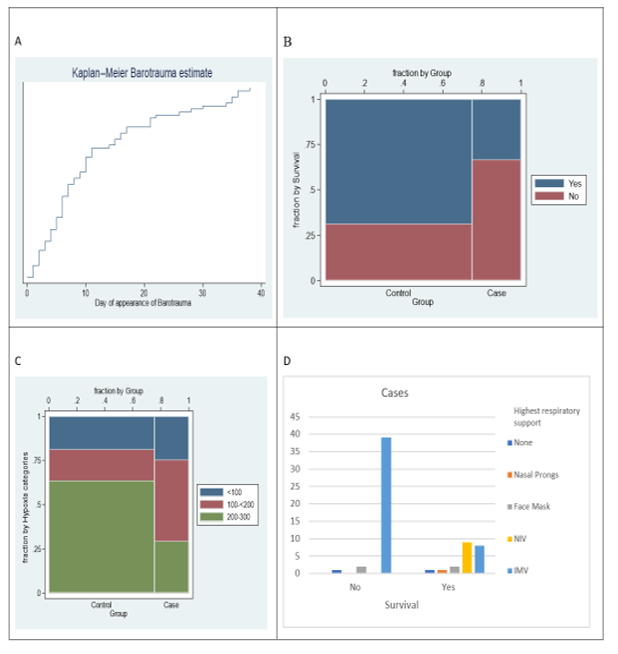
Figure 2: Characteristics of barotrauma cases and controls
A: Day of appearance of barotrauma, B: Survival for cases versus controls, C: S: F ratio for cases versus controls, D: Type of respiratory support at the time of barotrauma in cases.
Discussion:
The incidence of barotrauma was found to be 2.9%, and it was significantly associated with PPV and moderate hypoxia with an S:F ratio between 100-199. There was an association of barotrauma with higher mortality, ventilation days, and length of hospital stay.
Many researchers have reported barotrauma in Covid-19, but most of them have been with moderate to severe ARDS, which involves a higher risk of barotrauma with stiff lungs, PPV, and high PEEP. The incidence of barotrauma has been reported for Covid-19 patients to be 40% on IMV with severe respiratory failure. [6] In severe acute respiratory syndrome-coronavirus 1 (SARS-CoV1), it was seen in 34% of patients receiving IMV and around 15% for those receiving NIV. [7, 8, 9, 10] In the Middle East Respiratory Syndrome coronavirus (MERS-CoV), it was reported to be 30%, 44% with influenza A H7N9, and 8% with influenza A H1N1 when treated with IMV. [11, 12] The present study reports a lower incidence as all Covid-19 patients are studied irrespective of the presence or absence of PPV.
Thus, it brings up the fact that there can be other mechanisms contributing to the etiology of barotrauma in Covid-19 as some of the cases never experienced PPV.
As depicted by higher ferritin levels in cases, the severity of the disease might have contributed to barotrauma. It has been shown that increased ferritin levels could predict the severity of disease and a worse clinical prognosis. [13] The correlation of significant local inflammatory changes has been demonstrated by hyperactivation of macrophages, neutrophils, and natural effect of reduction of lymphocytes and rising severity of Covid-19. [14] The cause of the culprit high-pressure gradient or raised intrathoracic pressure causing barotrauma is not fully proven. Barotrauma has been reported despite lung-protective mechanical ventilation and patients who did not receive PPV. This raises a possibility of an association between disease severity and barotrauma. [15] The median day of barotrauma since admission to hospital in this study was eight days {Inter-quartile range (IQR) 4-16}, and the earliest report of barotrauma was on day 1 (without PPV), suggesting that in addition to PPV, the disease severity, viral pneumonia, Valsalva maneuver or some other mechanism might have contributed to barotrauma.
Hypoxia: As the disease progresses, the body's inflammatory response to hypoxia increases. [16] It is proposed that the neuroinvasive effect [17] or blunted respiratory system response to low oxygen and high carbon dioxide levels give rise to "happy hypoxia", a characteristic of the covid-19 disease. [18] Happy hypoxia explains the unawareness of disease severity by the patient and the incidence of barotrauma even without higher respiratory support (PPV). The incidence of barotrauma was lower S:F ratio<100 compared to that with the S:F ratio of 100-<200. This can be explained by the fact that mortality was significantly high with an S:F ratio<100.
Positive pressure ventilation: Once the hypoxia worsens, the chances of requiring PPV are high. PPV has been implicated in causing barotrauma. This study showed a higher association of barotrauma with PPV like many others. [19] Association of IMV with barotrauma and higher incidence in APRV mode of ventilation has also been reported. [8]
Steroids: A higher percentage of cases received steroids in this study. The results of the Recovery trial were released midway in the study period; hence, the physician's decision was influenced towards steroid administration. Dexamethasone might have increased lung frailty, or it could have been given in more severe diseases (who required oxygen supplementation), and hence there was a higher association with barotrauma, though found insignificant in multivariate analysis. A similar finding was also observed by Palumbo et al., but it needs more evidence. [20]
Outcomes: The outcomes of the cases were worse than controls. The ventilation days, length of stay, and mortality; all of them were significantly higher.
Limitation: It is a single-center retrospective study. Details of positive pressure ventilation like airway pressure at the time of barotrauma were not available because of the limitation of documentation during the covid era. Due to resource constraints, markers of severity like IL6 were not available for many patients.
Interpretation: This study finds a barotrauma incidence of 2.9% in Covid-19 disease, its association with PPV and S:F ratio between 100-199 and poor prognosis.
Generalizability: This study analyzed all admitted covid-19 barotrauma cases during the study period, not limiting to a single grade of severity and type of respiratory support. It also brings up the overall incidence of barotrauma with the disease Covid-19. Furthermore, as this disease has spread worldwide across all population types, it can be easily replicated.
Conclusion:
This study finds an incidence of 2.9% barotrauma with Covid-19 disease during March 2020-April 2021. The S:F ratio of 100-199 and PPV were strongly associated with the development of barotrauma. Barotrauma in Covid-19 disease is strongly associated but not limited to positive pressure ventilation. Outcomes like a higher length of stay, ventilation days, and mortality were significantly higher with barotrauma. Barotrauma should be suspected in event of sudden deterioration of respiratory status whether patient is intubated or no.
Acknowledgment relating to this article.
Assistance with the article: None
Financial support and sponsorship: None
Conflicts of interest: None
Presentation: None
Data availability: The data used to support the findings of this study is deposited on Mendeley and will be embarked after publication of this article.