Clinical Case Reports and Clinical Study
OPEN ACCESS | Volume 12 - Issue 5 - 2025
ISSN No: 2766-8614 | Journal DOI: 10.61148/2766-8614/JCCRCS
Ram B Singh1, Germaine Cornelissen2, Ghizal Fatima3, Kapil Kumar Sharma4
1Halberg Hospital and Research Institute, Moradabad, India.
2Halberg Chronobiology Center, University of Minnesota, Minneapolis, MN, USA.
3Era Medical College, Ghizal Fatima.
4Homeopathic Institute, Moradabad, India.
*Corresponding Author: Ghizal Fatima, Era Medical College, Ghizal Fatima.
Received: March 14, 2023
Accepted: May 05, 2023
Published: July 05, 2023
Citation: Ram B Singh, Germaine Cornelissen, Ghizal Fatima, Kapil Kumar Sharma (2023) “Our Approach to Anesthesia in Knee and Hip Arthroplasty”, Clinical Case Reports and Clinical Study, 2(9); DOI: http;//doi.org/07.2023/1.170.
Copyright: © 2023 Ghizal Fatima. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
A male physician, 77 years of age, presented with COVID-19 on April 17, 2021. He had severe insomnia and increase in night-time blood pressure (BP) as shown by self-measurements. He was administered Natrum Salicylicum 30 C (3 pills thrice daily) and a tincture (Gelsemium 200 C, once daily; 5 drops in 50 ml water at mid-day). This regimen allowed him to sleep within 48 hours of administration, hence he is continuing this treatment. After a week, BP measurements showed that BP was reduced, notably at night. Systolic(S) and diastolic(D) BP, which averaged 127.2/84.9 mmHg in April, decreased to 113.5/79.5 mmHg in June (P<0.001). It doubled in the case of SBP and DBP and increased by 85% in the case of heart rate (HR). The difference between daytime (09:00 and 13:00) and night-time (02:30 and 05:30) measurements also increased between April and June: from 1.8 to 3.4 mmHg in the case of SBP, from 0.5 to 2 mmHg in the case of DBP, and from 2.2 to 7.6 beats/min in the case of HR. The day vs. night difference, which was absent in April (P>0.10) reached statistical significance in June in the case of DBP (P=0.038) and HR (P=0.021). However, during recovery, SBP is significantly decreased overall (P<0.001). The decrease in SBP is statistically significant at all six sampling times: at 02:30 (P<0.001), 05:30 (P<0.001), 09:00 (P=0.007), 13:00 (P=0.012), 16:30 (P=0.036) and 20:00 (P=0.041). The somewhat larger decrease during nighttime as compared to daytime accounts for a 107% increase in the day-night excursion in SBP. The findings indicate that treatment with homeopathic medication may have been helpful in the decrease in nocturnal hypertension with improvement in dipping.
Introduction
Our planet earth revolves around its axis, causing the light and dark cycles of 24-Hours. resulting in to day and night (Figure 0.). These rotations of the planet are associated with alteration in physiological functions which vary according to time structure of 24 hours [1-5]. Environmental degradation may cause changes in climate, space and weather as well as in day and night cycles, which can influence physiology and biology leading to alterations in cardiovascular functions [4,5].
Figure 0.Revolving of earth around sun causing day and night with changes in circadian functions.(Adapted from Google).
Our understanding of the remarkably large intra-individual and inter-individual variations in blood pressure (BP) and heart rate (HR) may also be partly explained by changes in climate, space and weather [5]. This knowledge has improved mainly due to the use of ambulatory BP monitors (ABPM) to characterize systolic (S) and diastolic (D) BP in humans [1-7]. However, mercury manometer for measuring BPs is continuing because of its reliability and availability.
Adverse effects of high BP on the heart correlate better with 24-hour means of BP than with casual BP readings, to which nocturnal BP plays a particularly important role [8-10]. Under usual conditions, nighttime BP is typically lower than daytime BP. Elevated nocturnal BP (nocturnal hypertension) and disrupted circadian variation in BP emerged as independent risk factors for cardiovascular disease (CVD) and all-cause mortality [11, 12]. Variability in BP and HR stem from an endogenous circadian rhythm, which persists under constant conditions, and from a host of external factors, including an influence from space weather and climate [13-16]. Determinants of the circadian rhythm in BP are still poorly understood. It is not well known whether they are similar or different during the day or night and how that may interact with sleep [17]. While hypertensive patients with COVID-19 appear to have a poor prognosis, there is no evidence that hypertension increases the risk of new infection or adverse outcomes independent of age and other risk factors [18]. It has been suggested, however, that hypertension and BP variability are exacerbated by acute SARS-CoV-2 immune reactions [19]. Herein, we present a case report, indicating a new discovery, related to increased nocturnal BP, in a patient diagnosed with COVID-19 who self-measured his BP, HR and oxygen saturation (SpO2) for assessment of circadian patterns in these variables while hospitalized and during recovery.
CASE REPORT
A physician, 77 years of age, male, presented with COVID-19 on April 17, 2021, as manifestation of side effect of Kovishield vaccination. Details of the case regarding clinical presentation and treatment received during the acute stage have been reported earlier [20]. After recovery from acute phase COVID-19 pneumonia, this patient developed chronic hypoxia with SpO2 between 91% and 93%. In the first week of June 2021, 6 weeks after the acute phase, his total and differential blood counts and platelet counts were within acceptable limits;. Hb 11.2 g/dl. SGOT 42.0 IU/L (normal, up to 0-40 IU), and ferritin 305.60 ng/ml. His C-Reactive Protein (CRP) was 7.41 mg/L (normal, 0.00 to 10 mg/L), D Dimer 248.2 ng/ml (normal, <500 ng/ml), IL-6, 4.21 pg/ml ( normal, 0.0 to 0.5 pg/ml). His LDH was elevated, indicating increased inflammation and cardiac damage (250I U; normal, <225 IU). His plasma cortisol concentration at 8.00 AM was 845 ng/L (normal,e 140-690 nmol/L).
He recorded his BP, HR, and SpO2 at 02:30, 05:30, 09:00, 13:00, 16:30, and 20:00 for about 3 days from April 20 to 22, 2021, and again from June 1 to 3, 2021. BP was measured by mercury sphygmomanometer (systolic BP and diastolic BP phase V Korotkoff) on the right arm after 5 minutes of rest in the supine position. BPs were also recorded by automatic multipara monitors for confirmation of accuracy of BPs. Since he had chronic respiratory failure, SpO2 at rest was 92% to 93%. His echocardiogram showed an ejection fraction above 65% with no evidence of cardiac dilatation. A nebulizer with asthalin+budicort+evolin was continuously available and regularly administered twice daily. A marked recovery was noted after 6 weeks of treatment, but his computerized tomography showed haziness in lower lung zones, indicating post-COVID-19 fibrosis. Due to the presence of persistent fibrosis of the lung, he was administered tablets of Nintedanib soft gelatin capsules, 100 mg twice daily for 45 days.
Apart from the above treatment, he was administered hydrogen-rich water (HRW) by dissolving H2 magnesium tablets (3 tablets in the morning and 2 in the evening). Treatment with H2 was associated with significant increases in SpO2 measured by oximeter. Despite the above treatment, he had severe insomnia and increase in night-time BP as shown by self-measurements (Figures 1-4).
He was administered Natrum Salicylicum 30 C (3 pills thrice daily) and a tincture (Gelsemium 200 C, once daily; 5 drops in 50 ml water at mid-day). This regimen allowed him to sleep within 48 hours of administration, hence he is continuing this treatment. After a week, BP measurements showed that BP was reduced, notably at night.
SBP and DBP, which averaged 127.2/84.9 mmHg in April, decreased to 113.5/79.5 mmHg in June (P<0.001 for both SBP and DBP). HR also decreased from 106.2 to 98.7 beats/min (P<0.001). A small increase in SpO2 from 93.8% to 94.5% was also noted (P=0.017). Whereas a circadian variation cannot be documented by one-way analysis of variance based on the few measurements collected in this study, the difference between the maximal and minimal time-point means generally increased from April to June. It doubled in the case of SBP and DBP and increased by 85% in the case of HR. The difference between daytime (09:00 and 13:00) and night-time (02:30 and 05:30) measurements also increased between April and June: from 1.8 to 3.4 mmHg in the case of SBP, from 0.5 to 2 mmHg in the case of DBP, and from 2.2 to 7.6 beats/min in the case of HR. The day vs. night difference, which was absent in April (P>0.10) reached statistical significance in June in the case of DBP (P=0.038) and HR (P=0.021).
Student t tests were also applied to data collected at each separate time-point. The decrease in SBP was found to be statistically significant at all six sampling times: at 02:30 (P<0.001), 05:30 (P<0.001), 09:00 (P=0.007), 13:00 (P=0.012), 16:30 (P=0.036) and 20:00 (P=0.041). The somewhat larger decrease during nighttime as compared to daytime accounts for a 107% increase in the day-night excursion in SBP. The decrease in DBP was also statistically significant at 4 of the six sampling times: at 02:30 (P=0.003), 05:30 (P=0.002), 09:00 (P=0.031), and 16:30 (P=0.005). The somewhat larger decrease during nighttime as compared to daytime accounts for a 112% increase in the day-night excursion in DBP. The decrease in HR was statistically significant at 09:00 (P=0.046) and reached borderline statistical significance at 02:30 (P=0.057), 05:30 (P=0.050), and 20:00 (P=0.065). The larger decrease from evening to morning as compared to daytime accounts for an 85% increase in the day-night excursion in HR.
These results indicate that the circadian variation in BP and HR, which was practically absent in April, increased in prominence in June, albeit not to the extent that a circadian rhythm could be documented with statistical significance by ANOVA.
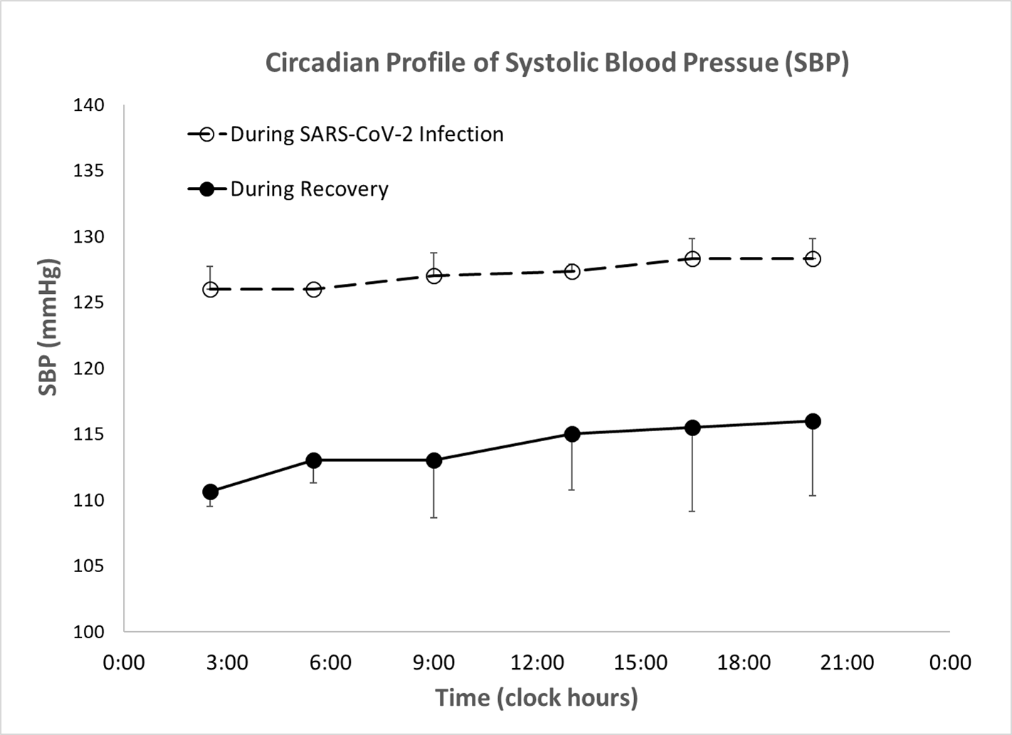
Figure 1. During recovery, SBP is significantly decreased overall (P<0.001). The decrease in SBP is statistically significant at all six sampling times: at 02:30 (P<0.001), 05:30 (P<0.001), 09:00 (P=0.007), 13:00 (P=0.012), 16:30 (P=0.036) and 20:00 (P=0.041). The somewhat larger decrease during nighttime as compared to daytime accounts for a 107% increase in the day-night excursion in SBP. A time-of-day effect, however, is not documented by one-way ANOVA during either hospitalization or recovery (P>0.15).
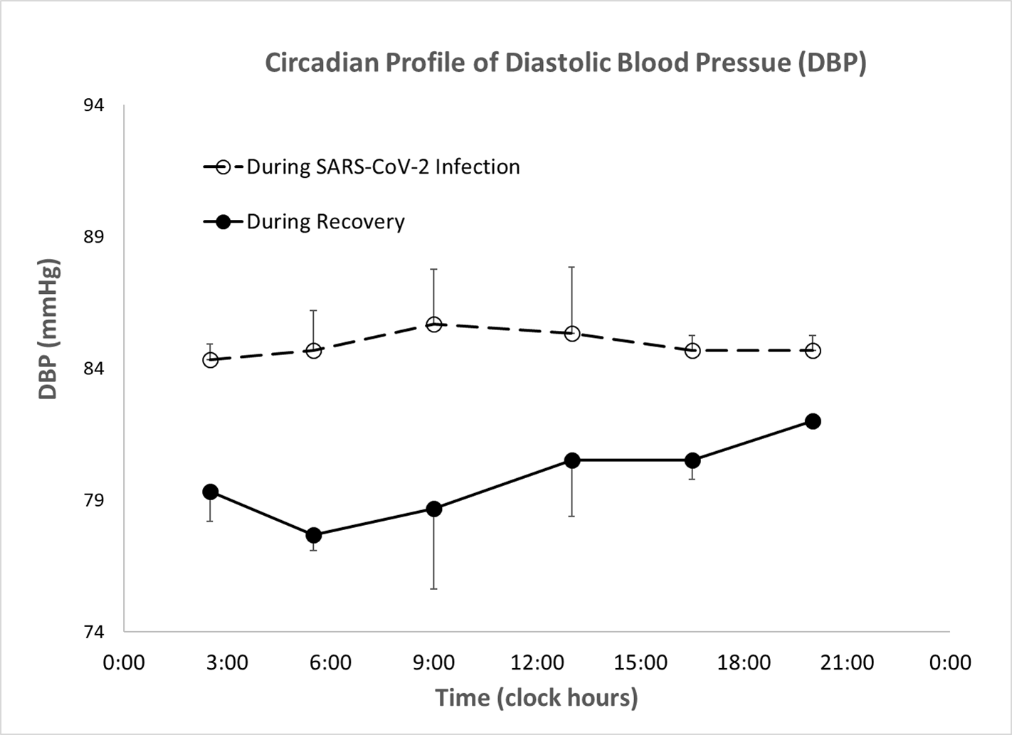
Figure 2. During recovery, DBP is significantly decreased overall (P<0.001). The decrease in DBP is statistically significant at 4 of the six sampling times: at 02:30 (P=0.003), 05:30 (P=0.002), 09:00 (P=0.031), and 16:30 (P=0.005). The somewhat larger decrease during nighttime as compared to daytime accounts for a 112% increase in the day-night excursion in DBP. A time-of-day effect, however, is not documented by one-way ANOVA during either hospitalization or recovery (P>0.70).
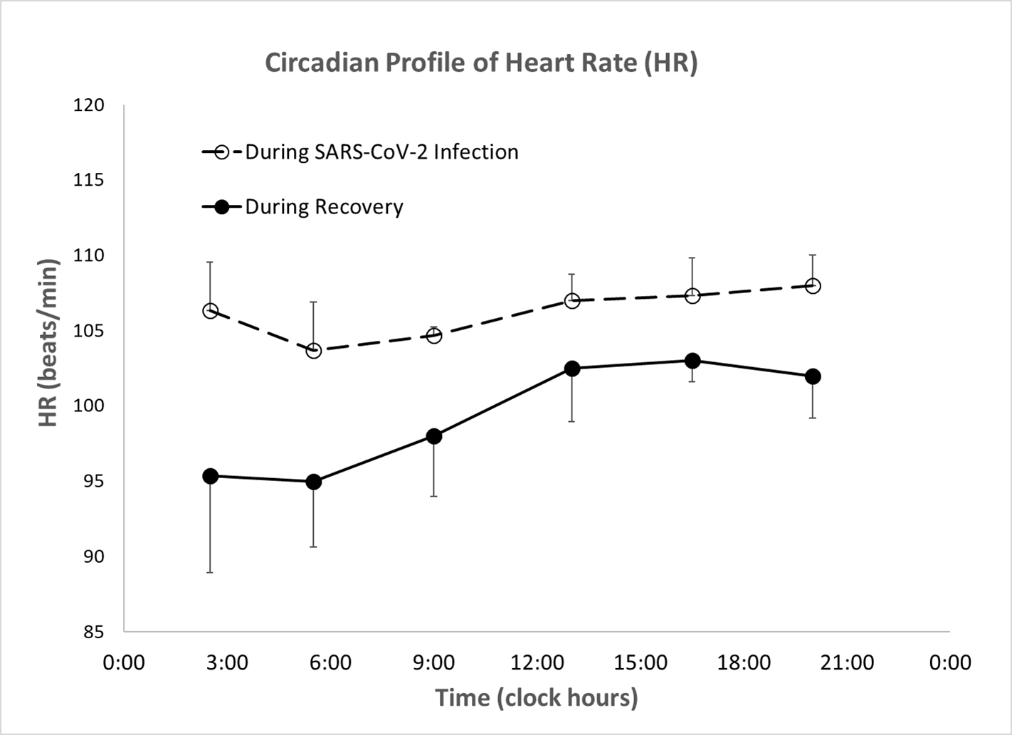
Figure 3. During recovery, HR is significantly decreased overall (P<0.001). The decrease in HR is statistically significant at 09:00 (P=0.046) and reaches borderline statistical significance at 02:30 (P=0.057), 05:30 (P=0.050), and 20:00 (P=0.065). The larger decrease from evening to morning as compared to daytime accounts for an 85% increase in the day-night excursion in HR. A time-of-day effect, however, is not documented by one-way ANOVA during either hospitalization or recovery (P>0.20).
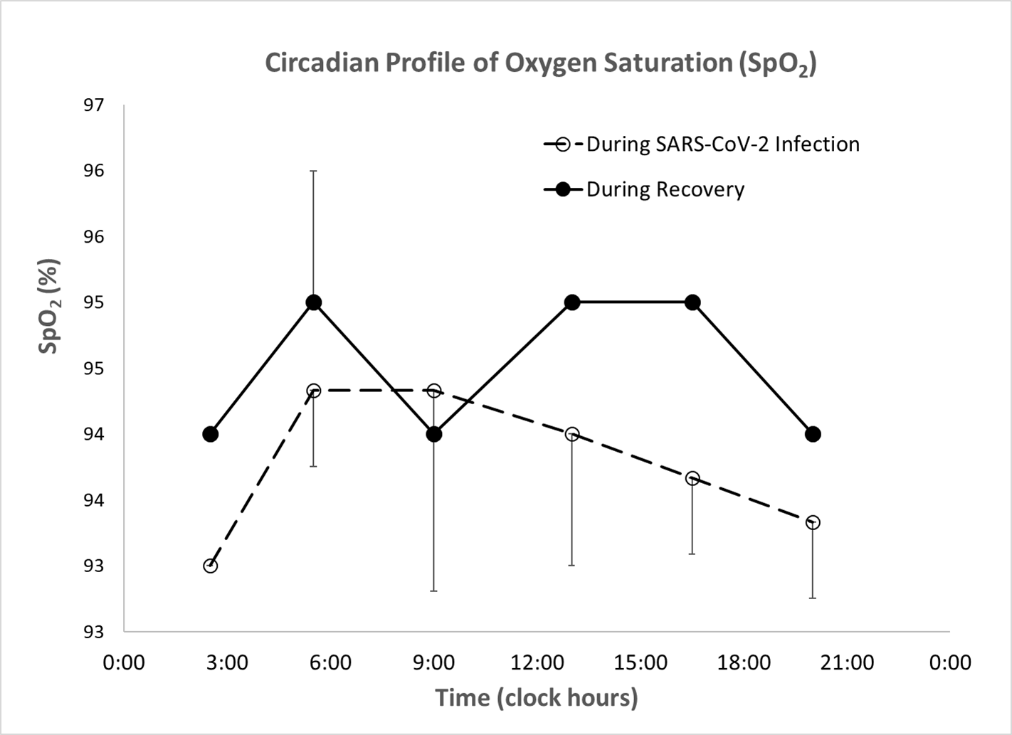
Figure 4. During recovery, SpO2 is slightly increased overall (P=0.017). The increase in SpO2 only reaches borderline statistical significance at 16:30 (P=0.053). A time-of-day effect is not documented by one-way ANOVA during hospitalization (P>0.30), but reaches borderline statistical significance during recovery (P=0.055).
COMMENTS
BP is normally lower during the night, starting to increase slightly after mid-sleep [21] with a larger increase after awakening in the morning, along with HR. The day-night difference in SBP, DBP and HR in this case was small but significant; it remained small even in June, when the nightly decrease became accentuated by a factor of about 2 (Figures 1-3).
The difference in BPs’ day vs. night, which was absent in April (P>0.10) reached statistical significance in June in the case of DBP (P=0.038) and HR (P=0.021). However, during recovery, SBP is also significantly decreased overall (P<0.001). The decrease in SBP is statistically significant at all six sampling times: at 02:30 (P<0.001), 05:30 (P<0.001), 09:00 (P=0.007), 13:00 (P=0.012), 16:30 (P=0.036) and 20:00 (P=0.041). The somewhat larger decrease during nighttime as compared to daytime accounts for a 107% increase in the day-night excursion in SBP. The findings indicate that treatment with homeopathic medication may be helpful in the decrease in nocturnal BPs and HR with improvement in dipping.
A blunted day–night difference in BP is an independent cardiovascular risk factor, although there is limited information on determinants of circadian variation in BP [12]. Musameh et al. [12] analyzed the association of mean daytime, mean night-time and mean day–night difference, defined as (mean daytime−mean night-time)/mean daytime in SBP and DBP, with clinical, lifestyle and biochemical parameters from 1,562 adult individuals (mean age 38.6 years) from 509 nuclear families recruited in the GRAPHIC Study. These authors estimated the heritability of the various BP phenotypes. Statistically significant associations of daytime or night-time SBP and/or DBP were found by multivariate analysis with age, sex, markers of adiposity (body mass index and waist–hip ratio), plasma lipids (total and low-density lipoprotein cholesterol and triglycerides), serum uric acid, alcohol intake and current smoking status. Of these, only age (P=4.7 × 10−5), total cholesterol (P=0.002), plasma triglycerides (P=0.006) and current smoking (P=3.8 × 10−9) were associated with the day–night difference in SBP, and age (P=0.001), plasma triglyceride (P=2.2 × 10−5) and current smoking (3.8 × 10−4) were associated with the day–night difference in DBP. Daytime, night-time, and 24-hour SBP and DBP showed substantial heritability (ranging from 18 to 43%). By contrast, the day–night difference in SBP showed a lower heritability (13%), while heritability of the day–night difference in DBP was not statistically significant. These data suggest that specific clinical, lifestyle, and biochemical factors contribute to inter-individual variation in daytime, night-time and day–night differences in SBP and DBP. Variation in day–night differences in BP is largely non-genetic. There was a significant increase in plasma cortisol in April in our case indicating possible circadian clock dysfunction.
The view once expressed that the circadian rhythm in BP was the result of the rest-activity cycle has long been revised to recognize the action of an endogenous component [22]. From monitoring during continued bedrest [23] and studies conducted under free-running conditions [24] to the demonstration of internal desynchronization between the circadian rhythms in BP and other physiological functions [25], the endogenicity of the circadian rhythm in BP is no longer disputed. This fact does not detract from the great susceptibility of BP to respond to a host of different external factors [26], including the BP-lowering effect of sleep. A change in climate, space and weather may also have influenced BPs but such possibility is least likely in this case (27-29].
It should be noted that large increases in cardiovascular disease risk are associated with Vascular Variability Disorders (VVDs), defined as an abnormal circadian variation in BP and/or HR. With MESOR-hypertension, VVDs include Circadian Hyper-Amplitude-Tension (CHAT) defined as too large a circadian amplitude of BP, ecphasia defined as an odd timing of the circadian BP rhythm but not of HR, an excessive pulse pressure and excessive pulse pressure product, and a deficient heart rate variability [1]. Newer devices now offer the capability of recording activity concomitantly, which represents an advantage, notably when data are analyzed solely in terms of dipping by calculating a day-night ratio instead of following a chronobiologic approach to characterize the circadian variation in terms of its rhythm parameters [27,28].
In brief, the larger decline in BPs during nighttime as compared to daytime accounts for a 107% increase in the day-night excursion in SBP. The findings indicate that treatment with homeopathic medication may be helpful in the decrease in nocturnal hypertension with improvement in dipping. The relatively small but significant excursion in BP and HR observed in this case may have resulted in part from the reduced activity caused by the disease and from the fact that measurements were taken manually, which implies that the patient was awake while taking a measurement. Automated measurements enabled by ambulatory monitoring devices would have overcome this limitation.