Clinical Case Reports and Clinical Study
OPEN ACCESS | Volume 13 - Issue 1 - 2026
ISSN No: 2766-8614 | Journal DOI: 10.61148/2766-8614/JCCRCS
Hao Thai Phan
Pham Ngoc Thach University of Medicine, Vietnam
*Corresponding author: Hao Thai Phan, Pham Ngoc Thach University of Medicine, Vietnam.
Received: June 26, 2023
Accepted: June 30, 2023
Published: July 03, 2023
Citation: Hao Thai Phan (2023) “A Case of Spontaneous Axillary Vein Thrombosis”, Clinical Case Reports and Clinical Study, 3(9); DOI: http;//doi.org/06.2023/1.181.
Copyright: © 2023 Hao Thai Phan. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
Axillary vein thrombosis is known as upper limb deep vein thrombosis which is a less common condition than lower limb deep vein thrombosis. Repeated trauma secondary to sport or job related arm movements and positions has been recognized as the predisposing factor for upper limb deep vein thrombosis. We describe a 48-year-old healthy female office worker admitted with swelling and pain in her right upper limb. Her history was unremarkable and fully vaccinated against Covid-19. Venous duplex ultrasound confirmed the presence of axillary vein thrombosis. Coagulation studies, immune diseases and cancer screening for secondary thrombosis were unremarkable. The patient was treated with full anticoagulation using low molecular weight heparin. On subsequent follow-up at one week, the patient was symptom free and duplex sonography showed no evidence of thrombosis. We will continue anticoagulation for a minimum of 3 months.
Introduction
Lower limb deep vein thrombosis (DVT) is a common and well-described condition which has recently noticed. The risk factors for lower limb DVT comprises of the underlying components of Virchow’s triad: venous stasis, hypercoagulability, and injury to the intima of veins.
Upper limb thrombosis, involving the axillary or subclavian vein, is a less common phenomenon1. This condition is subject to the same risk factors as the formation of lower limb DVT. Another way of assessing the risk factors for upper limb DVT is by considering endogenous (e.g., thrombophilia and pregnancy) and exogenous (e.g., external compression of the vein by the cervical rib or a solid tumor) causes, although it may occur spontaneously2.
The relatively fixed position of the axillo-subclavian vein in the thoracic outlet predisposes it to repeated trauma with arm movements, leading to the compression of the vein in the costo-clavicular space. The axillo-subclavian compression between the clavicle and the first rib may also be exaggerated with frequent strenuous arm movements (e.g., tennis and valley balls) or when the upper extremity is in particular positions such as the rigid military style of sitting with the back straight and the shoulders placed posteriorly and inferiorly (e.g., sitting at a computer desk)3. We report a case of spontaneous axillary vein thrombosis.
Case Report
A 48-year-old right-hand dominant woman woke up with acute pain and swelling in her right upper limb. She is a office worker and often reaches out to pick up the items on the shelf everyday. She had no intrinsic risk factors for thromboembolic disease and she doesn't take birth control pills.
On physical examination revealed erythema, heat, swelling, and tenderness localized to the ulna border of her right arm. There was no systemic feature of illness.
Laboratory tests including routine full blood count showed mild hypochromic microcytic anemia with low serum iron 4.43 µmol/l (7-26 µmol/l) and low ferritin 4.0 ng/ml (≤73.3 ng/ml), renal and liver profiles, inflammatory markers, thrombophilia test, immune diseases and viral screen were unremarkable, with the exception of elevated D-dimer 6410ng/ml (<500ng/ml). Brain MRI was normal.
Venous duplex ultrasound of her right arm demonstrated compressible radial, ulnar, and brachial veins with decreased compressibility in the right axillary vein and confirmed the presence of thrombosis extending throughout brachial and basal veins. Although there was no obvious symptom or sign of pulmonary embolism, we decided to proceed with chest computed tomography It showed thrombosis of the bilateral lobar pulmonary arteries (Figure 1). Abdominal computed tomography only had bilateral ovary cysts. Gastric and colon endoscopy were unremarkable.
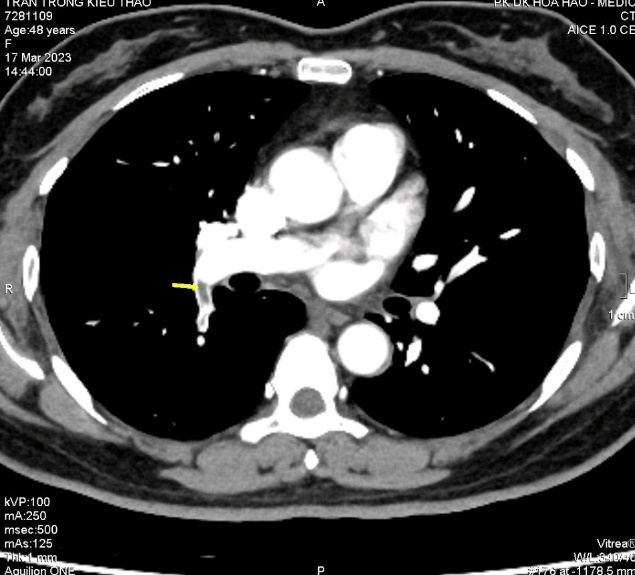
Figure 1. Lobar pulmonary thrombosis (yellow arrow head)
We treated the patient with anticoagulation using subcutaneous low molecular weight heparin and iron supplement, and her signs and symptoms gradually resolved over the next few days. On subsequent follow-up at one week, she remained well and asymptomatic and repeated venous Doppler ultrasound revealed complete resolution of the left axillary thrombosis.
Discussion
Thrombosis of the subclavian vein was first described in 1875 by Sir James Paget4, who named it “gouty phlebitis”. However, he incorrectly attributed this syndrome to vasospasm rather than to thrombosis. In 1884, von Schrötter5 independently described this condition and postulated that it resulted from occlusive thrombosis of the subclavian or axillary veins. In recognition of these physicians, Hughes6 coined the term “Paget–Schrötter syndrome” in 1949 to describe the syndrome of spontaneous primary thrombosis of the axillary or subclavian vein.
The estimated incidence of DVT from all causes is 131.5 per 100 000 person-years. Nonetheless, this may be an underestimation because a number of DVTs remain asymptomatic and therefore undiagnosed7. Prior to 1967, thrombosis of the axillary or subclavian vein was estimated to account for 1% to 2% of all DVTs. Since then, its incidence has risen due to increasing usage of central venous cannulation (CVC) and it is now estimated that upper limb DVT makes up 4% to 10% of all episodes of DVTs, with an approximate annual incidence of 3.6 per 100 000 persons8. Thrombosis is thought to occur in the dominant arm in 80% of cases3.
A thorough history taking and an appropriate physical examination are usually sufficient to suggest this diagnosis9. This may then be confirmed with a venogram or venous ultrasound scan. Differentiating between primary and secondary upper limb venous thrombosis is crucial in view of their different natural histories. Primary thrombosis accounts for 20% to 50% of all upper limb DVTs8,10. It includes real idiopathic cases and Paget–Schrötter syndrome, which is attributed to repetitive effort.
Major risk factors for secondary DVT are CVC, cancer, and upper extremity surgery11. Approximately, between 30% and 40% of all upper limb DVTs are cancer-related and 70% of secondary cases are related to CVC12. In a study, 38.5% of the patients who had a peripherally inserted central catheter line developed upper limb DVTs13.
As is the case for lower limb DVT, the diagnosis of upper limb DVT is crucial considering its potentially life-threatening complications such as pulmonary thromboembolism14.
It is predicted that the incidence of upper limb DVT will increase. The incidence of secondary upper limb DVT will increase due to more frequent usage of subclavian vein catheters, especially in patients with cancers, who are already at higher risk of developing this condition. The use of permanent pacemakers is also increasing, which will further add to the incidence of this disease. With our population’s increasingly sedentary lifestyle and the increasing employment opportunities in the information-technology industry with repetitive workload on the upper limb in an almost fixed position15.
Conclusion
Upper limb thrombosis is a less known and rarer condition than lower limb thrombosis and has been particularly associated with exogenous factors, including sports and occupation. Nevertheless, diagnosis of upper limb DVT is similarly crucial, and recognition and treatment of potential complications such as pulmonary embolism are vital.
Conflict of interest
None