Clinical Case Reports and Clinical Study
OPEN ACCESS | Volume 13 - Issue 1 - 2026
ISSN No: 2766-8614 | Journal DOI: 10.61148/2766-8614/JCCRCS
Eyad Zein Aldean 1, Ashraf Essameldin Elsanie 2
1 Specialized Medical Care Hospital, UAE.
2 Radiodiagnosis , Specialized Medical Care Hospital, UAE
*Corresponding authors:Eyad Zein Aldean, UBMS ORL-HNS, Specialized Medical Care Hospital, UAE.
Ashraf Essameldin Elsanie, Radiodiagnosis , Specialized Medical Care Hospital, UAE.
Received: February 03, 2021
Accepted: February 21, 2021
Published: March 03, 2021
Citation: Eyad Z Aldean, Ashraf E Elsanie. “ Sudden Sensorineural Hearing, a Possible Late complication of Covid 19”. Clinical Case Reports and Clinical Study, 3(1) ; DOI:10.61148/2766-8614/JCCRCS/027
Copyright: © 2021 Eyad Zein Aldean, Ashraf Essameldin Elsanie. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
,
Introduction:
COVID-19 was originally thought to resemble the flu, with pneumonia lung manifests. However, it has become clear the past couple months that the virus also attacks the brain, heart, kidneys, vascular system, caused severe inflammatory responses, causes venous thromboembolism (VTE) and can cause multi- organ failure. Within the brain, COVID-19 patients have been observed with ischemic stroke, intracranial hemorrhage, focal cerebral arteriopathy, hypoxic-ischemic encephalopathy, encephalitis and acute hemorrhagic necrotizing encephalopathy.
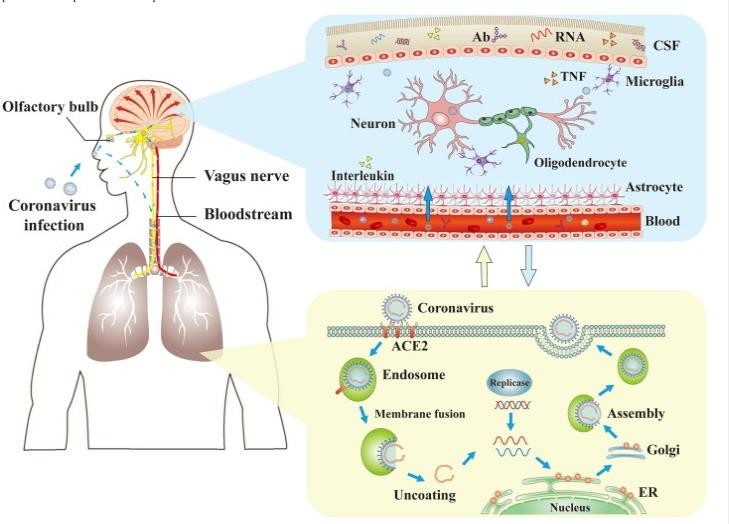 |
The mechanisms of coronaviruses infections and neurological damage caused by coronaviruses.
Ab: antibody; ACE2: angiotensin-converting enzyme 2; CSF: cerebrospinal fluid; ER: endoplasmic reticulum; TNF: tumor necrosis factor.
The coronaviruses can cause nerve damage through direct infection pathways (blood circulation pathways and neuronal pathways), hypoxia, immune injury, ACE2 and other mechanisms. Meanwhile, the coronaviruses have detrimental effects to attack the lung tissue and causes a series of lung lesions such as hypoxia. Furthermore, the coronaviruses can enter the nervous system directly through the olfactory nerve, and also enter the nervous system through blood circulation and neuronal pathways, resulting in neurological disorders.
I will present a case of sensorineural hearing loss secondary to demyelination of Left middle cerebellar peduncle area ,as COVID 19 possible late complications.
46-year-old male, tested positive for COVID 19 seven weeks ago, when he had developed cough and fever and had been admitted for two weeks, and treated with hydroxychloroquine
He presented with a 3 –day- history of sudden left sided hearing difficulty with tinnitus No history of recent head trauma, ototoxic medication or noise exposure
Past medical history: he has type 2 DM (poorly controlled) with HTN
Investigations:
At the onset of his hearing loss his white cell count was within normal range with a slightly elevated C- reactive protein . Full autoimmune screen including rheumatoid factor, antinuclear antibody, antineutrophil cytoplasmic antibody, centromere antibody was negative. Angiotensin converting enzyme, immunoglobulins and complement C3 and C4 were within normal range. A viral screen for influenza and HIV was negative.
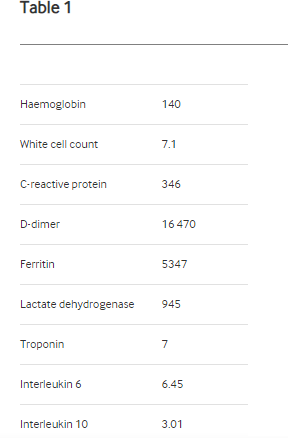
Inflammatory markers are shown in table 1.
 |
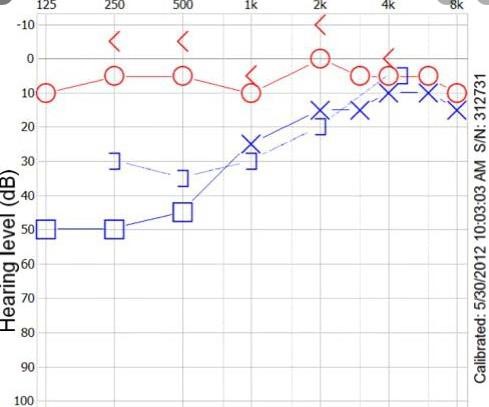
Pure Tone Audiometry revealed, left-sided low frequency moderately severe sensorineural hearing loss.
 |
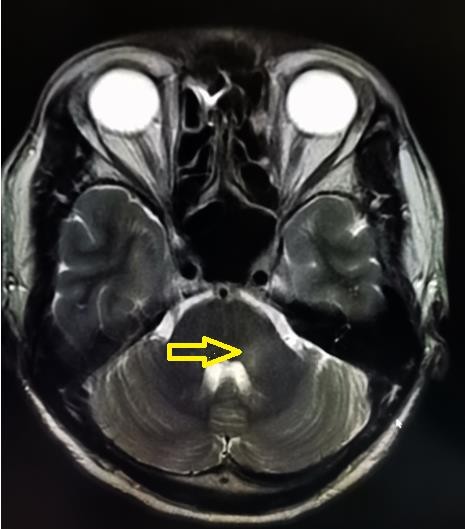
MRI brain revealed, area of abnormal signal, compatible with Demyelination.
 |
He was referred to Neurologist who treated him by a short course of oral corticosteroids.
Hearing improved clinically and the revised PTA after a month showed near -normal hearing levels.
Conclusion