Clinical Case Reports and Clinical Study
OPEN ACCESS | Volume 13 - Issue 1 - 2026
ISSN No: 2766-8614 | Journal DOI: 10.61148/2766-8614/JCCRCS
Humberto Morais 1*, Hilaryano Ferreira 2, Tchitchamene Nelumba 3
1 Department of Cardiology. Hospital Militar Principal/Instituto Superior, Luanda República de Angola
2Department of Cardiology, Hospital Professor Doutor Fernando Fonseca, Lisbon, Portugal
3Department of Pediatric Cardiology, Hospital Santa Cruz, Lisbon, Portugal
*Corresponding author: Humberto Morais – Hospital Militar Principal/Instituto Superior Rua Pedro Miranda 40-42 Maianga Luanda Republica de Angola
Received: February 11, 2021
Accepted: February 17, 2021
Published: February 22, 2021
Citation: Humberto Morais, Hilaryano Ferreira, Tchitchamene Nelumba (2021) Surgical Treatment Versus Percutaneous Closure of Ruptured Sinus of Valsalva Aneurysm: A Systematic Review and Meta-Analysis. Clinical Case Reports and Clinical Study, 2(2) ; DOI: 10.61148/2766-8614/JCCRCS/026
Copyright: : © 2021 Humberto Morais, This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
A sinus of Valsalva aneurysm may occur as a congenital or acquired defect at the junction of the aortic media and the surrounding fibrous tissue. They are generally asymptomatic until a complication sets in, thus can cause compression and or rupture of adjacent cardiac structures, resulting in symptoms which prompt urgent management. This condition may be managed surgically or percutaneously. We aim to evaluate the outcomes in surgical versus percutaneous closure of ruptured sinus of Valsalva. This Systematic review and meta-analyses statement included 254 patients, stratified in two groups, percutaneous group (70 patients) and surgical group (184 patients). Overall poor outcome occurred in 31 patients OR 0.75 (P= 0.51, I2=53%). Sub-analysis showed an occurrence of residual shunt (OR 1.71, P=0.47, I2=0%), aortic regurgitation “de novo” (OR 1.11, P=0.87), sinus of Valsalva aneurysm recurrence (OR4.28, P=0.31), pericardial effusion (OR 0.74, P=0.71, I2=0%), with a mortality OR 0.46 (CI 95% [0.08-2.75], P=0.39, I2=0%). The present study showed that when compared to surgical treatment the percutaneous closure of ruptured sinus of Valsalva is safe and effective, being an excellent alternative in selected patients.
Introduction
Sinus of Valsalva aneurysms (SOVAs) are rare but well-known cardiac pathologies. Congenital SOVAs is caused by absence of elastic tissue between aortic media and the annulus fibrosus. (1) Ventricular septal defect (VSD), aortic regurgitation (AR), and bicuspid aortic valve (BAV) are the most frequently lesions associated with this SOVAs type. In patients undergoing cardiac surgery, they are often seen in Asian rather than in Western populations (2). The right sinus of the Valsalva is the most frequently affected, followed by the non-coronary sinus. Aneurysms of the left sinus are rare (3).
SOVAs can be asymptomatic until a complication arises. Their most frequent complication is the aneurysm rupture into the adjacent cavities, mostly to right ventricle (fig.1) followed to right atrium (3-7). Other complications include compression of the adjacent structures, causing obstruction of the left or right ventricular outflow tract, (8,9) compression of the coronary arteries leading to angina, or myocardial infarction (10). Rarely dissection by SOVA of the interventricular septum may occur (11).
Conventional surgical repair with cardiopulmonary bypass is the most widely used repair technic of ruptured SOVAs worldwide with low mortality rates. However, morbidity may arise from cardiopulmonary bypass and thoracotomy (3-7).
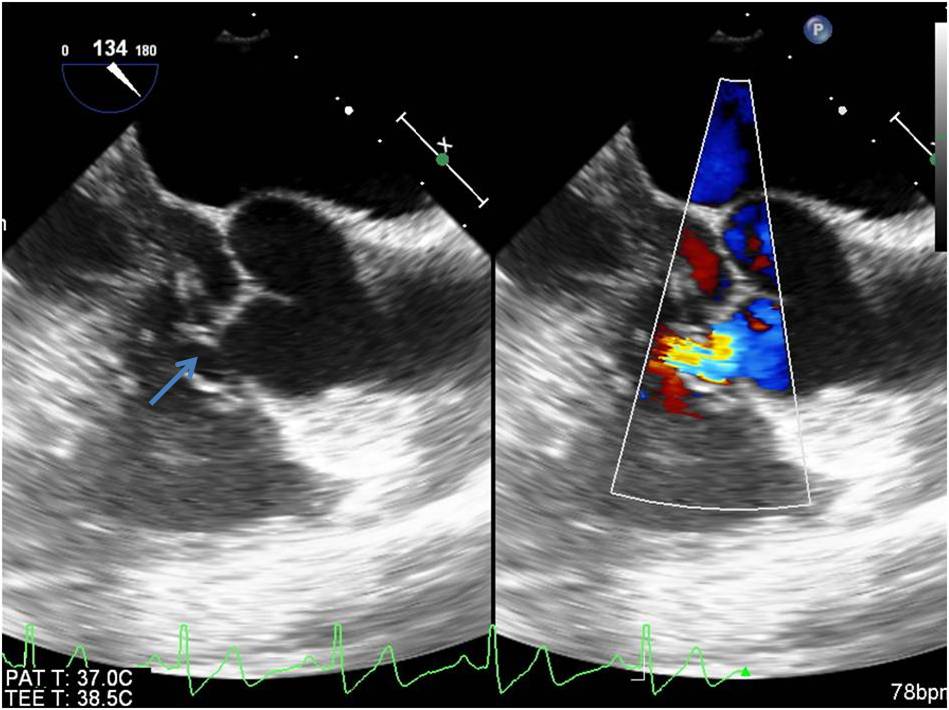
Figure 2 - Transesophageal echocardiography long axis view showing rupture of right sinus of Valsalva into right ventricle (arrow)
Percutaneous treatment of SOVA rupture was first attempted by Cullen et all, in 1994 using Rashkind umbrella device in a patient who had previous cardiac surgery for a ruptured SOVA (12). Since then, several series on this type of treatment have been published, utilizing the several closure devises, with good immediate mid-term or long term results (13-24). However, the number of patients included in each study is small from 4 to 25. In turn, data on direct comparison of surgical treatment versus percutaneous closure of SOVAs are scarce (25-27). Thus, the aim of this systematic review and meta-analysis is to evaluate the outcomes in surgical treatment versus percutaneous closure of ruptured SOVAs.
Methods
We conducted a search on PubMed and BVS Salud databases through January, 28 2021 using the MeSH term [’Sinus of Valsalva aneurysm and ‘surgery’ and ‘percutaneous closure’] according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement (PRISMA) (28) (fig. 2). Two investigators working independently screened all titles and abstracts of the studies for eligibility. Duplicate citations were discarded after the preliminary search results were obtained. Furthermore, the references list of all included studies and relevant review studies were also manually searched.
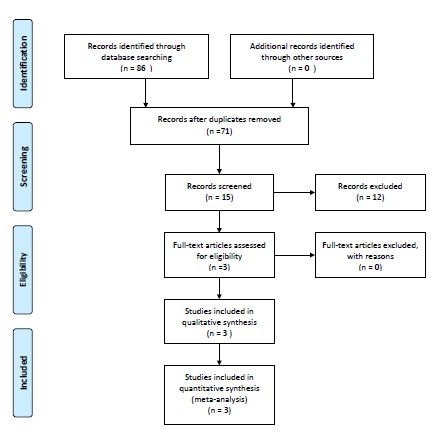
Figure 2 Flow chart according to Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA)
Inclusion criteria
We included in the meta-analysis only original articles that compare surgical treatment with percutaneous treatment of ruptured SOVAs
Exclusion criteria
We excluded from the meta-analysis articles other than original research articles and non-English language articles.
Data extraction
Data extraction was performed independently by two of the authors. We used standardized extraction forms that included author, year, study design, age, sex, follow-up duration, presence of major complications (residual shunt, aortic regurgitation “de novo”, pericardial effusion, aneurysm recurrence), and mortality. The primary outcomes were poor outcome defined by the presence of major complications and all-cause mortality. Secondary outcomes included incidence of residual shunt, aortic regurgitation “de novo”, pericardial effusion and aneurysm recurrence.
Quality Appraisal
The quality appraisal was established according to Le Floch and colleagues criteria. (29) This tool appraises the quality of the study based on the following questions: Did this article give an answer to the research question? Did the article focus clearly on the research question? Was the methodology appropriate? Do you believe the results? (Can it be due to chance, bias or confounding?). To be included, the article had to score “yes” on every question.
Statistical analysis: All comparisons were estimated on an intention-to-treat basis. The categorical variables were described as percentages and estimated by odds ratio (OR) with a two-tailed 95% confidence interval (CI). Continuous variables were described as mean and standard deviation and analysed by weighted mean difference (WMD). Statistic value I2 assessed by Q test was used to quantify the degree of interstudy heterogeneity. Considering the intrinsic variation in study design, we calculated the OR and WMD estimates using random-effects model for all comparisons. All P values were two-tailed, and the statistical significance was set at 0.05. Statistical analyses were performed using the Revman software package (Review Manager, Version 5.4. Copenhagen, The Nordic Cochrane Centre, the Cochrane Collaboration).
Results
A flow diagram of study selection is shown in Figure 1. A total of 86 papers were initially identified, of which 71 non related to the theme were excluded. After review of the full texts of the 15 remaining studies, 12 were excluded based on the absence of a direct comparison of surgical treatment with percutaneous closure of SOVA ruptures. Thus, three articles published between 2014 and 2020 with a total of 254 patients were included in this systematic review (25-27).
Table 1 shows baseline study characteristics. Three studies including a total of 254 patients with SOVA were included in these meta-analyses. 184 patients underwent surgical correction and 70 patients underwent percutaneous correction.
|
Studies |
Liu S et all 2014 |
Xiao JW 2017 |
Yang K 2020 |
|
Sample size, n |
35 |
85 |
134 |
|
Surgical treatment, n |
20 |
56 |
108 |
|
Percutaneous closure, n |
15 |
29 |
26 |
|
Age (yrs) mean±SD |
43 (16-74) |
37.6±611.9 |
39.2 ± 16.1§ |
|
34.6 ± 11.4¥ |
|||
|
Male n (%) |
23 (65,7%) |
59 (69,4%) |
85 (63,4%) |
|
Follow-up, months |
(2–240) |
(8–152) |
1–124 § |
|
1–84 ¥ |
|||
|
NYHA classification |
|
|
|
|
I |
NR |
0 |
53 |
|
II |
NR |
32 |
52 |
|
III |
NR |
40 |
25 |
|
IV |
NR |
13 |
4 |
Table 1 Clinical characteristic of the patients
Overall poor outcome occurred in 31 patients (24 in surgical vs 7 in percutaneous group). There was a tendency for lower rate of poor outcome in percutaneous group, but with no statistical difference OR 0.75 (P= 0.51, I2=53%) (fig 3). Sub-analysis although non-significant showed an overall higher tendency for individual poor outcome in surgical group OR 1.23 (P= 0.71, I2=0%). Residual shunt (OR1.71, P=0.47, I2=0%), aortic regurgitation “de novo” (OR1.11, P=0.87), SOVA recurrence (OR4.28, P=0.31). However there was a trend towards lower tendency for pericardial effusion in the percutaneous closure group, it was non-significant (OR 0.74, P=0.71, I2=0%) (fig. 4). Publication bias analysis was assessed and can be seen on the funnel plot, showing a symmetrical distribution of the outcomes (fig 5).
When it comes to mortality patients presented an OR 0.46 (CI 95% [0.08-2.75], P=0.39,I2=0%). although higher all mortality events occurred in the surgical group, it was not statistically significant (fig 6).
Figure 3 Forest Plot Showing Overall Poor outcome
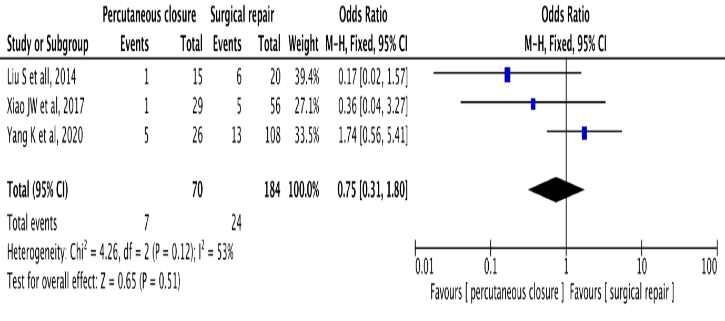
Figure 4 Forest Plot – Sub-analysis showing each individual outcome
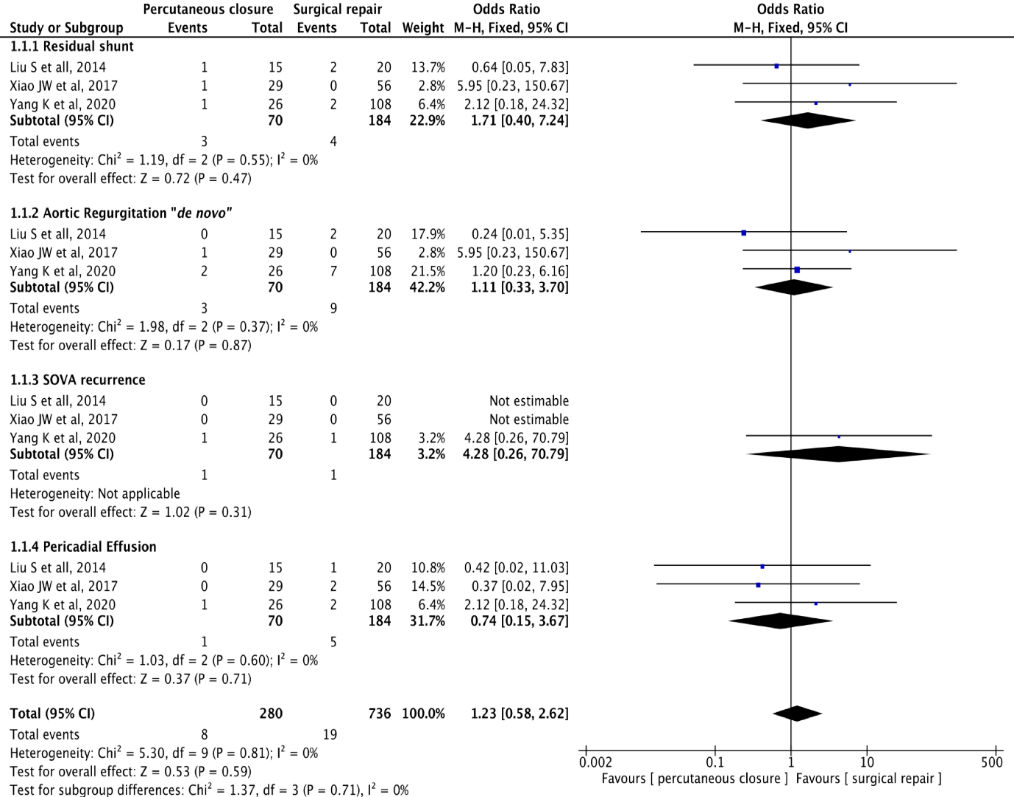
Figure 5 Funnel Plot - Risk of bias assessment, showing a symmetrical distribution of individual outcomes.
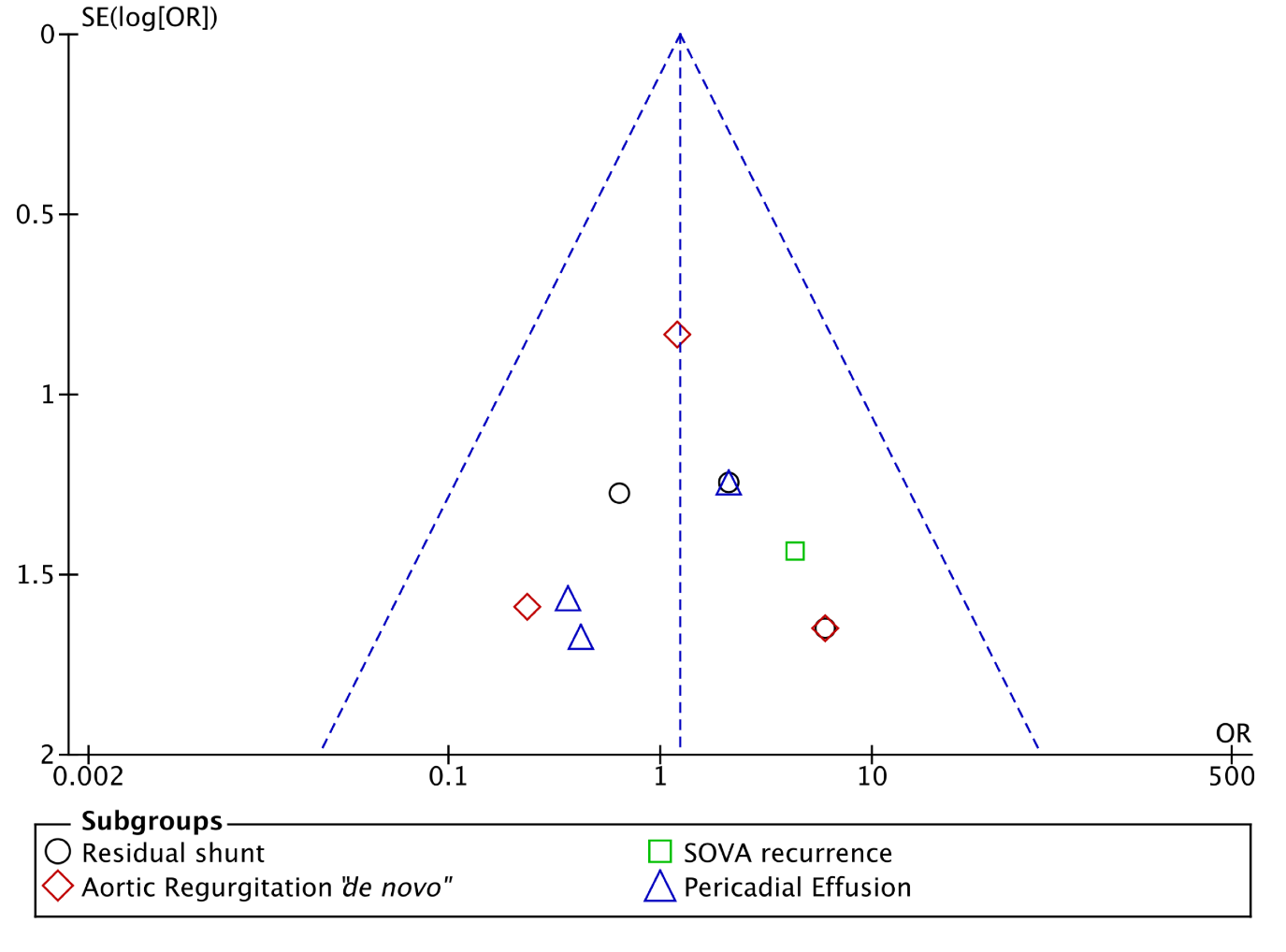
Figure 6 Forest Plot - Showing Overall Mortality 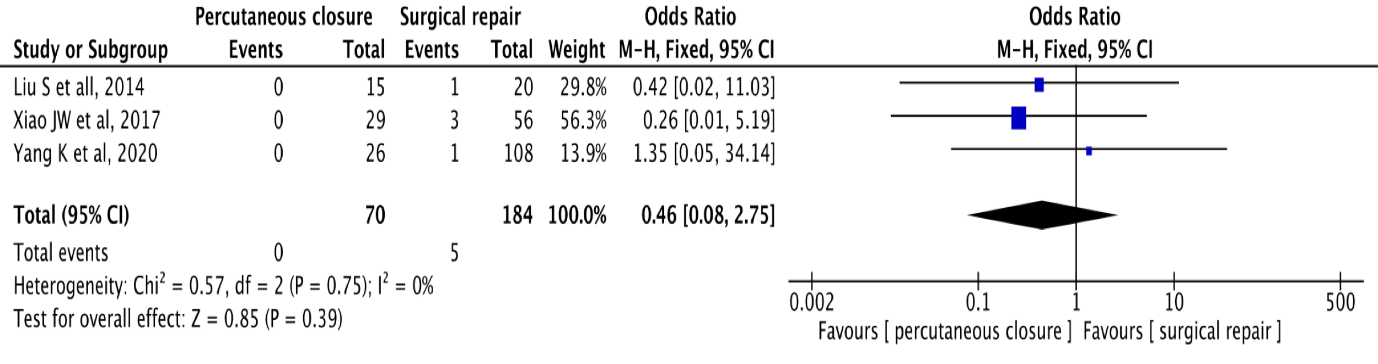
Discussion
Traditionally, surgical repair is the main treatment option for ruptured SOVAs because of the acceptably low mortality and good long-term outcome (3-7). With the development of minimally invasive interventional technics, percutaneous closure is becoming a promising alternative to surgery in appropriately selected patients. (13-24)
In this meta-analysis we included three studies, totalling 254 patients that directly compared surgical treatment with percutaneous transcatheter closure of ruptured SOVAs. (25-27)
The main results of this meta-analysis show that although not statistically significant there was a tendency for lower rate of poor outcome, defined by the presence of major complications or death, in the percutaneous group.
Residual shunt is a worrisome complication reported by several centres. (13,15,22,23) A trivial residual shunt can be detected after the procedure in up to 8% of patients undergoing percutaneous closure of ruptured SOVAs. These shunts generally disappear over time (14,15,17,19-22,24). Our meta-analysis showed that three (1.63%) of the surgically treated patients had important residual shunts. In one of these patients, the residual shunt (patch leak) was successfully treated via percutaneous with the placement of 3 occluders. (25) On the other hand, in the group of patients treated via percutaneous, one patient had a severe residual shunt with haemolysis. This patient was successfully operated one week after the percutaneous procedure. (25). All trivial shunts disappeared during follow-up period.
Aortic regurgitation (AR) “de novo” or progressive AR is another complication of both treatments and accounts for about 6,1% out of 163 percutaneous treated patients. Procedure-related aortic regurgitation may be severe and of sudden onset, requiring urgent surgical repair. (21,22) Our meta-analysis shows that in surgical group nine (4.8%) patients had “de novo” AR while, in group of patients treated via percutaneous only three (4,2%) had this complication. In percutaneous group one patient develop severe occluder-related “de novo” AR and was sent to surgery (26). The remainders “de novo” AR were trivial.
Our study showed that six patient had pericardial effusion, five (2.71%) in surgical group in three of which pericardiocentesis was performed, and one (1.4%) patient in patients treaded percutaneously.
Our meta-analysis showed that there was no occluders’ migration, which contrasts with what has been reported in patients underwent percutaneous closure of ruptured SOVAs published in other series (21,22,24)
In long-term follow-up, the recurrence of SOVA has been reported in several studies, both in surgical series (3) and in percutaneous treatment series. (21,24) The present meta-analysis shows that recurrence of SOVA occurs in one patient in each group, suggesting that such recurrence might be independent of the choice of the treatment (27).
Our meta-analysis shows that three perioperative deaths (1,6%) occur in surgical group: Two patients died of low cardiac output syndrome (25,26) and one patient died of respiratory failure (26). Furthermore, in follow up period another two (1,0%) patients died in surgical group: one patient died of infective endocarditis (26) and other patient died 74 months after surgery of unknown causes. (27). On the other hand, no early or late deaths in percutaneous treated group occurred. These results regarding to mortality are consistent with those reported in several studies. In percutaneous treated patients the early mortality is null (13-24), while early mortality in patients with surgically treated ruptured SOVA although low, it still exist. (2-7).
The studies included in our meta-analysis were not randomized, so it is not possible to exclude bias in the results. It is known that patients with other associated cardiac malformations are treated surgically. While patients treated percutaneously are carefully chosen. Contra-indication for this type of treatment are related to size of the defect, and to presence of concomitant pathologies such as large ventricular septal defect, severe aortic regurgitation or suspected infective endocarditis (15,30)
Conclusions
In conclusion, our meta-analysis showed that when compared to surgical treatment the percutaneous closure of ruptured SOVAs is safe and effective, being an excellent alternative in selected patients. Randomized studies comparing the two types of treatment should be done to better demonstrate the real importance of percutaneous treatment of this pathology.
Declarations
Financing: nothing to declare
Competition of interests: The authors declare no conflicts of interest.
Acknowledgments: nothing to declare
Author’s contribution
Study design: HM
Data collection: HM and TN
Writing of the manuscript: HM and HF
Revisions and approval of the final manuscript: All authors
Supervision: HM