Clinical Case Reports and Clinical Study
OPEN ACCESS | Volume 13 - Issue 1 - 2026
ISSN No: 2766-8614 | Journal DOI: 10.61148/2766-8614/JCCRCS
Arun Nadarajah1*, Chuang Tzu-Yi (Arron)1, Chong Hon Ian1
1Department of General Surgery, Cairns Hospital, North Cairns, Queensland, Australia
*Corresponding Author: Arun Nadarajah, Department of General Surgery, Cairns Hospital, North Cairns, Queensland, Australia.
Received: March 01, 2023
Accepted: March 06, 2023
Published: March 10, 2023
Citation: Arun Nadarajah, Chuang Tzu-Yi Arron, Chong Hon Ian (2023) “Rare complication of ventriculoperitoneal shunt – Inguinal-scrotal hernia with shunt in situ in an elderly male”, Clinical Case Reports and Clinical Study, 2(9); DOI: http;//doi.org/03.2023/1.165.
Copyright: © 2023 Arun Nadarajah. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
Ventriculoperitoneal shunt is commonly used to reduce the intra-cranial pressure in hydrocephalus patient. Migration of distal end of ventriculoperitoneal shunt has been reported in many studies as common complications. It is noted that migration of distal tip of VP shunt to scrotum through inguinal hernia can occur in paediatric population. This case report demonstrates an unusual VP shunt migration to scrotum in an elderly male.
Introduction
In the case of hydrocephalus, a ventriculoperitoneal (VP) shunt is used to redirect cerebrospinal fluid from within the ventricles to a different place.(1) Distal catheter migration is one of the uncommon side effects of shunts, and the scrotum has been mentioned among other body regions. Although incidences of distal catheter migration into the scrotum in paediatric patients have been documented, cases in adult patients are uncommon because of destroyed processes vaginalis. In this report we shall illustrate a rarer event of inguinoscrotal hernia from migrated VP shunt in an elderly adult.
Case Report
Mr. AT is a 55 years old male who was admitted under rehabilitation for 3 months post- bilateral cerebral bleeding with interventricular extension bilaterally. He has a past medical history of mitral valve replacement in 2014 secondary to mitral valve infective endocarditis, immune-mediated glomerulonephritis and he has been on long term anticoagulation.
A right external ventricular drain was initially inserted for obstructive hydrocephalus, which was complicated by ventriculitis. A long course of flucloxacillin and vancomycin was given and subsequently a right VP shunt was inserted. While he was in the rehabilitation unit, he had noticed a growing lump at this right groin, which has given him discomfort especially when he was walking or urinating. On the examination, there was an obvious protrusion/lump extending to right scrotum noted both on standing and lying. The lump was easily reducible with positive cough impulse. Incidentally, there was also a cough impulse at the left groin area. The impression was that he has bilateral reducible inguinal hernia, in which right is larger than left. He subsequently had a Xray (Figure 1) which demonstrate that the distal part of VP shunt is located at the pelvic area. A computed tomography (CT) of abdominal/pelvis (Figure 2-4) was conducted and showed that the tip of the VP shunt is seen within the right inguinal canal, with fluid present adjacent to the end of the VP shunt. The incidental findings of a small right hydrocoele and a left inguinal hernia were noted.
A neurosurgical consult suggests that no urgency of reposition was required given the VP shunt is still functioning and the hernia is reducible. Mr. AT was organised for elective laparoscopic bilateral inguinal hernia repair.
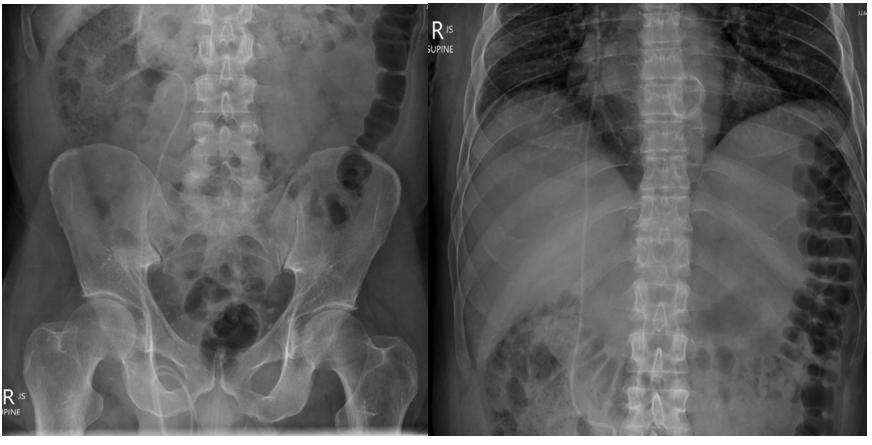
Figure 1-3: Coronal view computed tomography scan of the abdomen with arrows further demonstrating the migration of distal tip of VP shunt to right scortum.
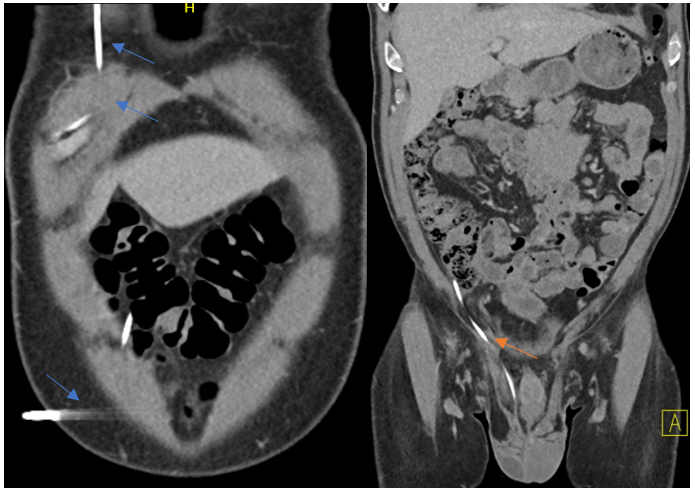

Figure 2: Coronal view computed tomography scan of the abdomen with orange arrows indicating
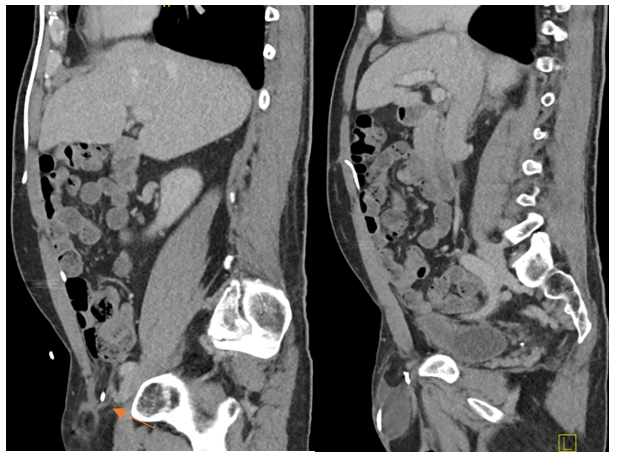

Sagittal view computed tomography scan of the abdomen with arrows demonstrating the position of VP shunt

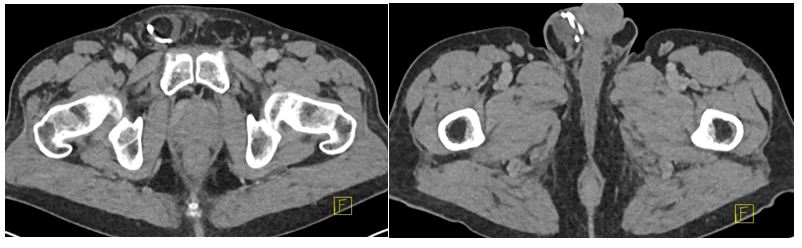
Axial view computed tomography scan of the abdomen with the inguino-scrotal position of VP shunt
Discussion
VP shunt placement is the highest utilised surgical treatment option for hydrocephalus. VP shunt migration to scrotum is a rare complication and it is more commonly reported in paediatric population. Hence, there is a chance that this diagnosis could be missed in a geriatric patient in rehabilitation with very mild symptoms. The overall incidence of migration to the scrotum in relation to other sites is 14%. (2) The VP shunt in scrotum can cause progression of inguinoscrotal hernia, scrotal oedema, hydrocele and shunt extrusion from scrotum.
The processus vaginalis generally closes completely at the age of 2-year. It can however remain patent in up to 15 to 30% of the population till adulthood. (3, 4) The patent processes vaginalis can allow the cerebrospinal fluid drains from the abdominal cavity to scrotum, resulting in hydrocele. This flow creates a ‘trough effect’ which migrates the shunt into the scrotum. (5) As there is a smaller peritoneal cavity with higher intra-abdominal pressure in children, there is higher chance for the distal part of VP shunt migrates to the scrotum through the patent processus vaginalis. (6)
Only a few cases of distal catheter migration into scrotum in adults were reported. With the limited evidence, some said VP shunt migration into scrotum can be associated with serious complications including acute scrotum or shunt extrusion. (7)
The recommendation for the management includes closure of the defect with repositioning of the distal catheter and hernial sac repair. It is suggested that both groins should be explored even the other side has no obvious hernia. This is believed that the intra-abdominal pressure is high in patients with VP shunt and a higher risk of recurrence can occur. Hence, a laparoscopic approach along with catheter truncation is recommended.
Conclusion
In this case report, distal catheter migration of a VP shunt into a right inguino-scrotal hernia (scrotum) in an elderly male is depicted. Given that majority of these migrations happen in a paediatric population this case is more unique. Given the diagnosis was made while the patient was in rehabilitation, it is important to look out for the rare but possible case of a mildly symptomatic inguinal hernia being caused by a VP shunt migration. This will help facilitation earlier elective or emergent surgery on evaluating the patient properly as opposed to dismissing it as a less urgent outpatient matter in the geriatric population.
Acknowledgements:
AN and TC were involved in the conception, draft and writing of the manuscript. AN was responsible for manuscript edition and HC provided overall oversight over this project.