Clinical Case Reports and Clinical Study
OPEN ACCESS | Volume 13 - Issue 1 - 2026
ISSN No: 2766-8614 | Journal DOI: 10.61148/2766-8614/JCCRCS
Charl H. Woo1*, Cristóbal S Berry-Cabán2, Daniel C. Kim1, Jose J. Diaz1
1Physical Medicine and Rehabilitation Residency Program, Larkin Community Hospital, South
Miami, FL 33143
2Department of Clinical Investigation, Womack Army Medical Center, Fort Bragg, NC 28310
*Corresponding author: Charl H. Woo, Physical Medicine and Rehabilitation Residency Program, Larkin Community Hospital, South MIami, FL 33143 Email: charlie.h.woo@gmail.com
Citation: Charl H. Woo, Cristóbal S Berry-Cabán, Daniel C. Kim, Jose J. Diaz (2023) “Case Report: Abdominal Pain from Incarcerated Recurrent Obturator Hernia with Richter Component”, Clinical Case Reports and Clinical Study, 1(9); DOI: http;//doi.org/01.2023/1.159.
Copyright: © 2023 Charl H. Woo. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
Obturator hernia is a rare type of hernia found most predominantly in chronically ill elderly females with high mortality if diagnosis is delayed. Although it may show physical symptoms of an intestinal obstruction with radiological abnormalities on abdominal and pelvic computed tomography (CT) scan, many of these hernias can be undetected due to lack of specific symptoms or findings. Here we present an 85-year-old female with body mass index 18.08 kg/m2 who presented with abdominal pain, nausea and vomiting most prominently in the left lower quadrant with radiation down the left leg. She was a known case of previous obturator hernia approximately 15 years prior to the recurrent episode. Following exploratory laparotomy with manual manipulation, the incarcerated Richter hernia was resected with anastomosis and the defect in the left obturator foramen was repaired with bioabsorbable mesh retroperitoneally. No complication was observed postoperatively. Although extremely rare, recurrent obturator hernia should be considered in elderly and thin female patients, especially with symptoms of bowel obstruction and history of prior obturator hernia.
Objective: Objective of this care report is to provide evidence on the rarity and difficulty of early diagnosis on obturator hernia and associated complications. Diagnostic findings for obturator hernia on physical exam, imaging studies, as well as surgical treatment for repair are also provided.
Obturator hernia is a rare cause of intestinal obstruction that occurs most commonly in elderly thin females [1]. Clinical diagnosis of obturator hernia is often difficult, even among experienced clinicians due to nonspecific findings. As a result, high morbidity and mortality rates occur from delayed diagnosis with poor prognosis. Although physical exam can provide some evidence, computed tomography (CT) scan provides radiological findings more specific for obturator hernia and its early surgical treatment options [2]. The present case report provides highlights on the rarity of recurrence of obturator hernia with its Richter component, and details surgical treatment plan and difficulty on accurate diagnosis.
Case Presentation
An 85-year-old female was admitted due to abdominal pain in the lower left quadrant continuing for 2 days with 1 episode of nausea and vomiting in the morning. The patient described the pain as intermittently grabbing in nature that reoccurred every few minutes. She also complained of pain radiating down her lower left extremity. The patient had a history of an obturator hernia repair approximately 15 years earlier. Her body weight was 44 kg, and body mass index (BMI)
was 16.52 kg/m2. During her physical examination, the patient had diffuse rebound tenderness with involuntary guarding but showed soft abdomen with mildly increased bowel sounds without distention or rigidity. Scattered gas was observed in non-obstructed pattern in the small and large bowel in abdominal radiography (Figure 1).

Fig. 1. X-ray of the abdomen. Note distended loop of bowel
Radiograph of the abdomen showing distended loop of bowel (white arrow
A CT scan of the abdomen and pelvis was performed for further examination (Figure 2). The CT revealed postoperative changes of the bowel with mild small bowel distention with fluid in the mid abdomen however, a definitive diagnosis of obturator hernia based on the initial CT scan was not confirmed by the radiologist.
|
|
Fig. 2. Computed Tomography scan of the abdomen. Note thickened loop of bowel entrapped in the left obturator foramen which was confirmed later (white arrow).
Due to the patient’s inconclusive imaging and the non-resolving pain in the abdomen, while hospitalized, an exploratory laparotomy by midline incision was made near the pervious herniorrhaphy incision site. Upon opening, a non-foul-smelling serous fluid with markedly dilated bowel was identified. Examination revealed a partially incarcerated, recurrent obturator hernia of the large intestine, containing mesentery on the left in the area previously observed at the last operation (Figure 3). The bowel was transected proximally and distally incorporating the pervious anastomosis. Two pieces of bioabsorbable mesh were used intraoperatively. The first piece was rolled and placed into the opening of the obturator canal to fill the hernia. The second piece was then placed over the opening in the retroperitoneum that was later closed over and repaired. The bowel was re-approximated with a surgical stapler between the two ends of the small bowel. The patient tolerated the procedure well, and no complications were observed postoperatively. She was discharged 19 days post herniorrhaphy.
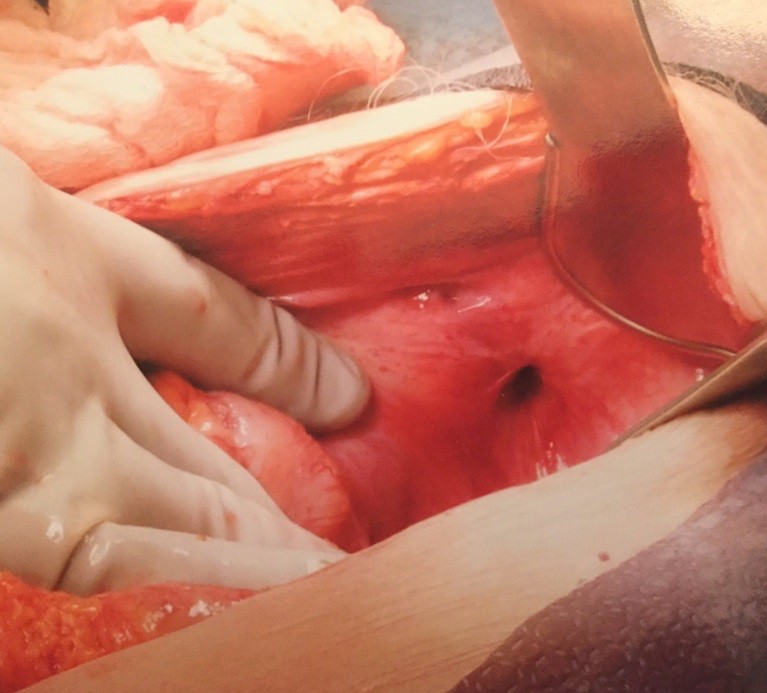
Fig. 3. Recurrent obturator hernia in the left obturator foramen
Upon completion the surgical procedure, the CT scan was re-evaluated by the radiologist again. After careful re-evaluation, the radiologist did indeed addend to confirm the diagnosis of left obturator hernia.
Discussion
Obturator hernia is a rare pelvic hernia responsible for approximately 0.4% of all bowel obstructions and approximately 0.073% of all hernias [1]. Obturator hernia is difficult to diagnose because symptoms from initial physical exam are nonspecific. Furthermore, imaging studies sometimes fail to provide accurate findings. Unlike most other abdominal wall hernias, obturator hernia is associated with high mortality if diagnosis is delayed [3]. Obturator hernia shows a high predisposition to incarceration and strangulation, leading to associated sepsis and bowel resection from possible necrosis [1]. Due to its rarity, difficulty in early diagnosis, and high tendency for bowel strangulation, mortality can be as high as 25% [4]. A report of 13 patients, included 7 who required bowel resection, 5 who developed infectious complications, and 2 who died [5].
Obturator hernia, first described by Ronsil in 1724 and first successfully operated by Obre in 1851, presents with the hernia sac sliding through the obturator foramen where the obturator nerve passes [6]. With the involvement of the obturator nerve being compressed by the hernia in the foramen, it is not uncommon for patients to present with neurological signs such as radiating pain, grabbing and tingling on the ipsilateral side of the involvement. Howship-Romberg sign reflects the pain most commonly exhibited in patients with obturator hernia, which demonstrates the acute pain by the incarceration of the anterior division of obturator nerve on the medial side of the thigh and exacerbation of this pain with the extension, abduction and medial rotation of the thigh [7, 8]. It is considered pathognomonic of obturator hernia and is seen up to 15-50% [2]. In 20% of cases palpable mass can be found in the proximal medial aspect of the thigh at the origin of the adductor muscles [6, 9]. High suspicion for obturator hernia should arise in thin, elderly patients with signs of bowel obstructions and neurological symptoms down the leg or pain upon extension, abduction and medial rotation of the thigh.
Our patient did not exhibit the pathognomonic Howship-Romberg sign but exhibited signs of bowel obstructions including vomiting and abdominal pain with grabbing pain radiating down the ipsilateral leg. There was also more difficulty in early clinical diagnosis of obturator hernia due to nonspecific physical findings with unclear radiological findings on initial CT. However only after careful re-evaluation on the initial CT imaging of the abdomen the radiologist confirmed a thickened loop of bowel entrapped in left obturator foramen (Fig. 2). This illustrates the challenge to confirm accurately obturator hernia even by an experienced radiologist, showing true difficulty for early imaging diagnosis.
Early CT imaging can aid early diagnosis with reduced morbidity and mortality associated with obturator hernia [10]. Standing X-ray of the abdomen shows evidence of small bowel obstruction in cases of obstructed obturator hernia [2]. The best diagnostic imaging modality is CT. CT imaging of bowel herniating through the obturator foramen and lying between the pectineus muscle anteriorly and obturator externus muscle posteriorly is diagnostic [2]. This is best demonstrated by low axial CT image in inguinal and upper thigh region. Asymptomatic bilateral obturator hernia can also be diagnosed by CT [11]. In cases of unclear radiological findings with continuing physical symptoms such as pain or neurological abnormalities, laparotomy is recommended for further examination.
Many techniques have been described for obturator hernia repair, but surgical repair is not standardized. Currently there is no absolute, clear method of choice for repair of single or multiple obturator defects [1]. Some reported methods include sac ligation, direct suture repair, local flaps by using periosteum, bladder, or uterine ligament, autologous tissue plug with rib cartilage, and prosthetic repair with tantalum gauze or Teflon [12-14].
In our patient, obturator hernia was found via exploratory laparotomy. After reduction of the distended bowel and anastomosis was completed after resection, a bioabsorbable mesh was used to fix the defect in the obturator hernia and to prevent further recurrence by covering the opening in the retroperitoneum. With no standardized method to fix obturator hernia, it is usually determined by the attending surgeon on which approach to pursue to obtain the best results.
Resection was required in our patient because the bowel appeared in the process of reducing that the antimesenteric Richter’s hernia of the bowel had ruptured.
Richter hernia is described to show partial strangulation of the circumference of the intestine’s antimesenteric border through an abdominal wall defect [15]. In most cases of Richter hernia, the intestinal lumen stays free and does not exhibit symptoms of intestinal obstruction, as less than two thirds of the bowel circumference is involved [16]. Obturator canal is not a common place for Richter hernia; femoral ring (71%) is the most common site, followed by deep inguinal ring (23%) and ventral or umbilical hernia (6%) [16]. Treatment is bowel reduction of the incarcerated segment and fascial defect repair [17]. There is currently no standardized method of herniorrhaphy, and Richter hernia can be repaired by laparotomy or laparoscopy. The significance of our case portrays the rarity of the recurrence of obturator hernia that has high mortality and morbidity. Given how uncommon Richter component is, in such a location gives an opportunity to reiterate the awareness and skills necessary for early diagnosis and timely treatment for best patient outcome possible.
Conclusion
Obturator hernia is a rare type of hernia due to low occurrence rate. It is most prevalent in chronically thin, elderly women. Although physical symptoms may be non-specific Howship- Romberg sign is pathognomonic for obturator hernia. Diagnostic imaging of choice for obturator hernia is CT. Reduction of the bowel and “patch” covering is frequently used as the primary method for herniorrhaphy. Richter hernia is present when the wall of the intestinal lumen is partially incarcerated leaving the lumen free and not completely obstructed. The femoral ring and inguinal ring are common sits of Richter hernia; however, it can also occur in obturator foramen although rare. Although physical exam findings and initial radiological evaluations may not be confirmatory, physicians should be well aware of the possibility of encountering obturator hernia and not be reluctant to proceed with exploratory laparotomy based on clinical correlation due to high mortality and morbidity associated with obturator hernia.
Disclosures
Human subjects: Consent was obtained from the participant in this study. Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following: Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work. Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work. Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work