Clinical Case Reports and Clinical Study
OPEN ACCESS | Volume 13 - Issue 1 - 2026
ISSN No: 2766-8614 | Journal DOI: 10.61148/2766-8614/JCCRCS
N Chikanya1*, C Hutchinson2, A Niblock1
1Haematology department, Antrim Area Hospital, N. Ireland.
2Radiology department, Antrim Area Hospital, N Ireland.
*Corresponding Author: N Chikanya, Haematology department, Antrim Area Hospital, N. Ireland.
Received: October 12, 2022
Accepted: October 17, 2022
Published: January 18, 2023
Citation: N Chikanya, C Hutchinson, A Niblock (2023) “Is there any future role for uncovered biliary stents?”, Clinical Case Reports and Clinical Study, 1(8); DOI: http;//doi.org/01.2023/1.151.
Copyright: © 2023 N Chikanya. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
,
A 73 year old woman was admitted with RUQ pain, pale stools, dark urine and painless jaundice. Her liver biochemistry showed a cholestatic picture. She proceeded to ultrasound which showed an Ill-defined hyperechoic mass lesion at the head of pancreas with dilatation of the pancreatic and common duct. A CT abdomen and pelvis reported a large upper abdominal mass in keeping with malignancy, likely pancreatic origin, extending from the superior head of pancreas to the inferior surface of the liver. She was subsequently discussed with gastroenterology who proceeded to ERCP and put in a metallic CBD 10mm expanding metal covered stent with palliative intent. The patient then developed pain in the neck with swollen right tonsil and associated cervical lymphadenopathy which was biopsied. An endoscopic ultrasound was performed, and biopsies of pancreatic mass collected which at histology were reported as EBV positive diffuse large B Cell Lymphoma.
Patient subsequently proceeded to have 6 cycles of chemotherapy with R CHOP. Unfortunately, the journey with chemotherapy was interrupted with recurrent bouts of neutropenic sepsis which responded well to antibiotics. The suspected source of infection was suspected to be biliary based on fluctuating obstructive LFTs. Following treatment, the PETCT had shown the pancreatic mass had resolved completely.
The patient then presented again with lethargy, generalised unwellness and fevers. Her bloods showed a cholestatic picture and leucopenia. She was commenced on iv antibiotics for infection of unknown source. She proceeded to have an MRCP which showed that the metallic biliary stent had migrated and was now present in the third part of the duodenum. There was also pneumobilia and mid CBD stricture.
This case demonstrates a few learning points:
Although initial imaging was highly suggestive of pancreatic cancer which would have led to a palliative diagnosis, biopsy is always crucial given that high grade lymphomas can arise from any tissue and be potentially curable.
Although the stent was initially put in for palliative measures it was beneficial that the stent was coated allowing its removal. In this case it spontaneously migrated, but on the other hand we would have wanted it removed by endoscopy to prevent any further infective episodes. If this patient had a bare metal stent inserted, it would have required an extensive operation to restructure her biliary system and raises the question is there any future role for bare metal stents in the biliary system.
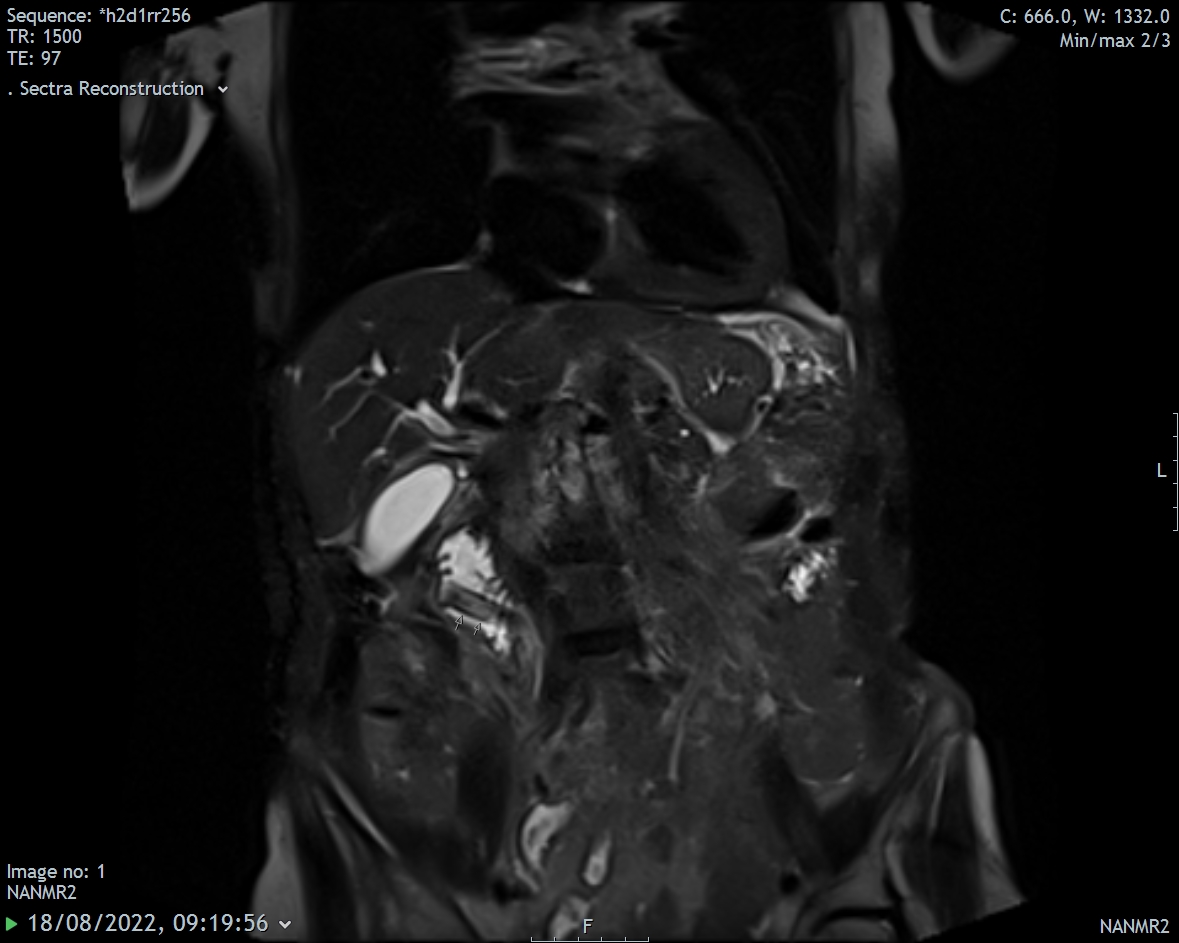
Coronal T2FS MRI image demonstrating the upper extent of the biliary stent in the third part of the duodenum (arrows), removed from the common bile duct
Conflict of interest statement: The authors have no conflict of interest to declare