Clinical Case Reports and Clinical Study
OPEN ACCESS | Volume 13 - Issue 1 - 2026
ISSN No: 2766-8614 | Journal DOI: 10.61148/2766-8614/JCCRCS
Afaf Khouna 1, Sara Bouabdella 1, Nada.Zizi 1,2, Siham Dikhaye 1,2
1 Department of Dermatology, Mohammed VI University Hospital of Oujda, Medical School of Oujda, Mohammed First University of Oujda, Morocco.
2 Department of Epidemiology, Clinical Research and Public Health Laboratory, Medical School of Oujda, Mohammed First University of Oujda, Morocco.
*Corresponding author: Afaf Khouna, Department of Dermatology, Mohammed VI University Hospital of Oujda, Medical School of Oujda, Mohammed First University of Oujda, Morocco.
Received: February 02, 2021
Accepted: February 20, 2021
Published: March 04, 2021
Citation: Khouna A, Bouabdella S, Zizi N, Dikhaye S. “ A New Case of a Primary Necrotizing Fasciitis of the Chest Wall ”. Clinical Case Reports and Clinical Study, 2(6) ; DOI: 10.61148/2766-8614/JCCRCS/024
Copyright: © 2021 Afaf Khouna. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Necrotizing fasciitis or necrotizing bacterial dermo-hypodermitis is a bacterial dermo-hypodermitis affecting the soft tissue and muscular fascia. It occur most frequently along the lower aspects of the body. The primary chest involvement is exceptional. It is a rare condition, rapidly progressive, and a devastating evolution, responsible for a mortality rate of up to 30 to 76%. The most cases reported in the literature are secondary to a medical procedure such as thoracic drainage, or transparietal biopsy. Only an early diagnosis and a rapid and adapted management are able to improve prognosis. We report a new case of a primary chest wall necrotizing fasciitis in a diabetic patient.
Introduction :
Necrotizing fasciitis (FN) is a rare infection of the subcutaneous tissue and deep fascia [1]. It occur most frequently along the lower aspects of the body, such as the legs, perineum, and lower abdomen [2]. The primary chest involvement is exceptional, and constitutes a diagnostic and therapeutic emergency. The most cases reported in the literature are secondary to a medical procedure such as thoracic drainage, or transparietal biopsy [1]. In addition to this, chest wall necrotizing fasciitis has been highly lethal [3]. We report a new case of a primary chest wall necrotizing fasciitis in a diabetic patient.
Presentation of the case :
A 53-year-old Moroccan lady, with unbalenced diabeties since 3 years, who has been poorly balanced. She was admitted to the emergency department for a big necrotic lesion of the back with foul smell discharge, evolving since 3 weeks, wich had started with a little painful red papule expanding and becoming necrotic. On the top of the lesion she has applied a mixture of medicinal plants. She had not taken any antibiotics. Clinical examination found a feverish patient (39 °), with an hypotension 100/40 mmHg and 94% in saturation. She had a giant and painful necrotic lesion in the posterior chest wall, surrounded by a peripheral erythema (figure 1).
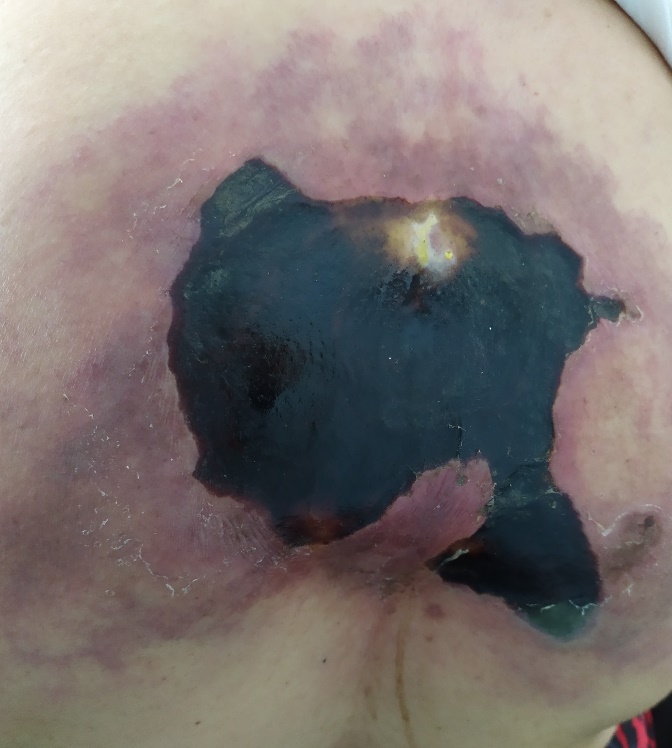
Figure 1 : Giant and painful necrotic lesion in the posterior chest wall, surrounded by a peripheral erythema
In addition, no infectious portal of entry has been found . Laboratory analysis revealed a hight level of CRP 320 mg / l with a leukocytosis 17210 / mm3, hyperglycemia at 3.5 g / l and a hight level of lactate 6.48 mmol / l. HIV serology was negative. CT scan showed a large collection of dorsal subcutaneous soft tissues with infiltration of adjacent fat and an important subcutaneous emphysema (figure 2).

Figure 2 : Thoracic CT scan with a large collection of dorsal subcutaneous soft tissues with infiltration of adjacent fat and an important subcutaneous emphysema
Emergency surgical debridement was required. A full-thickness necrosis of the posterior chest wall was found, involving the skin, fascia, and muscle layers. The patient then benefited from a large necrosectomy exposing part of the trapezius and large dorsal muscles with abundant washing and the placement of two Delbet blades for drainage (figure 3).
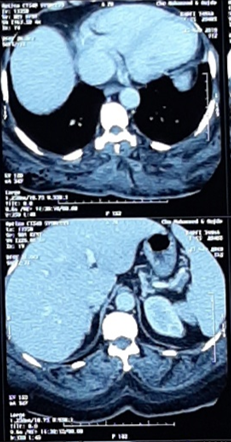
Figure 3 : Necrosectomy exposing part of the trapezius and large dorsal muscles with the placement of two Delbet blades.
The resultant defect in the posterior chest wall was covered with mesh. The surgical treatment was associated to a triplé probabilist antibiotic therapy with ceftriaxon 2g / d, metronizal 500mg / 8h and gentamycin 320 mg / d. Deep pus culture showed a multibacterial infection by staphylococcus aureus, klebsiella pneumoniae and proteus mirabilis sensible to ceftriaxon and gentamycine. The postoperative outcome was uneventful and the patient was stable at day 2 on post operative. The negative pressure wound therapy (VAC) could not be done because of the unavailability of the treatement.
Discussion :
Necrotizing fasciitis (NF) or necrotizing bacterial dermo-hypodermitis is a bacterial derma-hypodermitis affecting the soft tissue and muscular fascia [4]. It is the most severe stage of infections of the skin and softs tissus. It affects all the cutaneous planes (epidermis, dermis, hypodermis), deep fascias and sometimes muscles underlying [1]. Unlike cellulite which is limited to the dermis [5]. It is a rare condition, rapidly progressive with devastating evolution, responsible for a mortality rate of up to 30 to 76%. The recognized risk factors are age> 50, diabetes, peripheral vascular disorders (36%), chronic alcoholism and drug addiction (15 to 20%) and immunosuppression (cancers, immunosuppressive treatments, chemotherapy) [1].
In a large series of 166 patients with necrotizing fasciitis, the extremities were the most common site of infection (57.8%), followed by the abdomen (12.1%), perineum (12.1%), buttocks (10.2%), head and neck (8%), and chest (5%) [3]. The primary involvement of the chest wall is exceptional. The few rare clinical cases reported in the literature are secondary to thoracic drainage, pulmonary or esophageal surgery, transparietal pulmonary biopsy or thoracic empyema [6]. A recent Moroccan study has reported 7 cases of primary necrotizing fasciitis of the chest wall [1].
NF is caused by microorganisms called ‘flesh eating bacteria’, mainly represented by group A beta-haemolytic streptococcus [4]. However, in reality, these bacteria do not feed on the flesh, but release toxins, which are deadly for living cells, or which, by their effects on the immune system, lead to the production of free radicals [5].
In 1977, Giuliano classified NF into Type I and II based on microbial source. Type I is a polymicrobial infection involving mixed aerobic and anaerobic bacteria. Type II is caused by Group A Streptococcus alone or in association with S. aureus. Some studies later classified NF caused by Vibrio spp as Type III [7]. Multi-microbial associations have been found in 40 to 90% of NF. The main germs found are group B streptococcus and Clostridium Perfringens [5]. It has been reported that polymicrobial infections may present in a more insidious manner, unlike monomicrobial infections wich often present in a fulminate fashion [3]. In our case, it was a multibacterial infection caused by klebsiella pneumoniae and proteus mirabilis wich are present just in 6,1% in the literature [8]. Staphylococcus aureus was also present in our case wich is reported in 10,4 % of cases [8].
Clinical features of chest wall necrotizing soft tissue infection are similar to those seen at other sites including wound pain, skin blistering, crepitus, foul-smelling watery discharge from the wound, and dramatic deterioration in the patient's condition. Because there are few early symptoms (cutaneous manifestations appear late), diagnosis is difficult and may require biologycal exams and radiographic imaging [3].
Early diagnosis and treatment are the two main factors responsible for the prognosis [1]. The antibiotic treatment must be started immediately, even before the results of the microbiological analyses. The recommended antibiotic treatment consists in the association of β-lactamine, imidazole±aminoside [4]. It is complementary to the surgery because the local diffusion of antibiotics is weak because of the vascular thromboses responsible for the necrosis of the deep planes [5].
Wong et al. proposed a different approach to the debridement in necrotizing fasciitis, involving the classification of the affected area into the three surgical zones: (1) Necrotic tissue, which is completely excised; (2) infected but potentially salvageable soft tissue, which is carefully assessed and progressively cut back; and (3) non-infected skin, which is left alone [3].
The additional use of a negative pressure wound therapy (VAC) and hyperbaric oxygen therapy for management of NF of the chest wall has been reported with success.[4]
Conclusion :
Our case is added to the few cases published in the literature of a primary NF of the chest wall, to alarm, against this entity specially in diabetec patient. Only an early diagnosis and a rapid and adapted management are able to improve prognosis.