Clinical Case Reports and Clinical Study
OPEN ACCESS | Volume 13 - Issue 1 - 2026
ISSN No: 2766-8614 | Journal DOI: 10.61148/2766-8614/JCCRCS
Zayd BERRERHDOCHE1,2, Azeddine LACHKAR1,2, Drissia BENFADIL1,2, Fahd ELAYOUBI1,2
1Department of otolaryngology head and neck surgery, , University Hospital Center Mohammed VI, OUJDA, Morocco.
2Faculty of Medicine and Pharmacy, Mohammed Ist university, Oujda, Morocco.
*Corresponding Author: Zayd BERRERHDOCHE, Department of otolaryngology head and neck surgery, , University Hospital Center Mohammed VI, OUJDA, Morocco.
Received: November 03, 2022
Accepted: November 07, 2022
Published: November 11, 2022
Citation: Zayd BERRERHDOCHE, Azeddine LACHKAR, Drissia BENFADIL, Fahd ELAYOUBI (2022) “KYSTE GEANT DE LA 2e FENTE BRANCHIALE: A PROPOS D’UN CAS. SECOND BRANCHIAL CLEFT CYST: A CASE REPORT.”, Clinical Case Reports and Clinical Study, 1(8); DOI: http;//doi.org/11.2022/1.152.
Copyright: © 2022 Zayd BERRERHDOCHE. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
Amygdaloid cysts are benign dysembryological cystic tumors that develop in the antero-lateral part of the neck, they represent 2% of laterocervical tumors of the neck, they are among the most frequent gill anomalies, they represent 6.1 at 85.2% of second cleft anomalies. They are due to the persistence of the cervical sinus during the differentiation of the branchial apparatus. They are manifested by a laterocervical swelling located at the anterior edge of the sterno-cleido-mastoid muscle. Their cystic nature is confirmed by ultrasound and CT. Treatment consists of surgical excision.
We report the case of a 33-year-old man who consulted for a huge right laterocervical swelling which had been evolving for 16 months without any other associated symptoms. An exploratory cervicotomy with anatomo-pathological study was performed, the histological diagnosis retained was an amygdaloid cyst without signs of malignancy.
The objective of this work is to analyze the anatomo-clinical characteristics and to discuss the methods of management and the therapeutic indications of this affection.
INTRODUCTION :
Tonsilloid cysts are among the most common gill anomalies, accounting for 6.1 to 85.2% of second cleft anomalies. They are due to the persistence of the cervical sinus during the differentiation of the branchial apparatus. The usual site is the middle third of the anterior border of the sterno-cleido-mastoid muscle but they can be located at any point from the middle constrictor muscle of the pharynx to the supraclavicular region. We report this rare case of a huge laterocervical amygdaloid cyst.
PATIENT AND OBSERVATION:
A 33-year-old patient, chronic smoking and occasional alcoholism with no other notable pathological history, who presented for 16 months a right laterocervical swelling which increases in volume gradually, without associated otological or rhinological signs, the clinical examination found an enormous right laterocervical tumefaction going from the tip of the mastoid above to the supraclavicular region below, painless, slightly mobile, non-pulsatile measuring almost 70mm in long axis, of renitent consistency, its full limit was impossible to specify, the adjacent skin was healthy. Examination of the oropharynx, nasopharynx and pharyngolarynx was normal. The injected cervico-facial CT objectified the presence of (Figure 1).The cervico-facial MRI found a cystic mass under the right angulomandibular wall with a thick wall in its upper part of the same dimensions associated with lymph nodes in the territories of IIa and IIb suggesting a cyst of the 2nd branchial cleft (Figure 2).The PET scanner (Figure 3) shows a relatively intense hypermetabolic area with a necrotic center under the right angulomandibular (49mm*54mm*69mm) The diagnosis of a cervical cyst was retained, The patient benefited from a left cervicotomy with a complete resection of the cyst, the postoperative course was simple. Histological examination confirmed the diagnosis of an amygdaloid cyst without signs of malignancy (Figure 4).
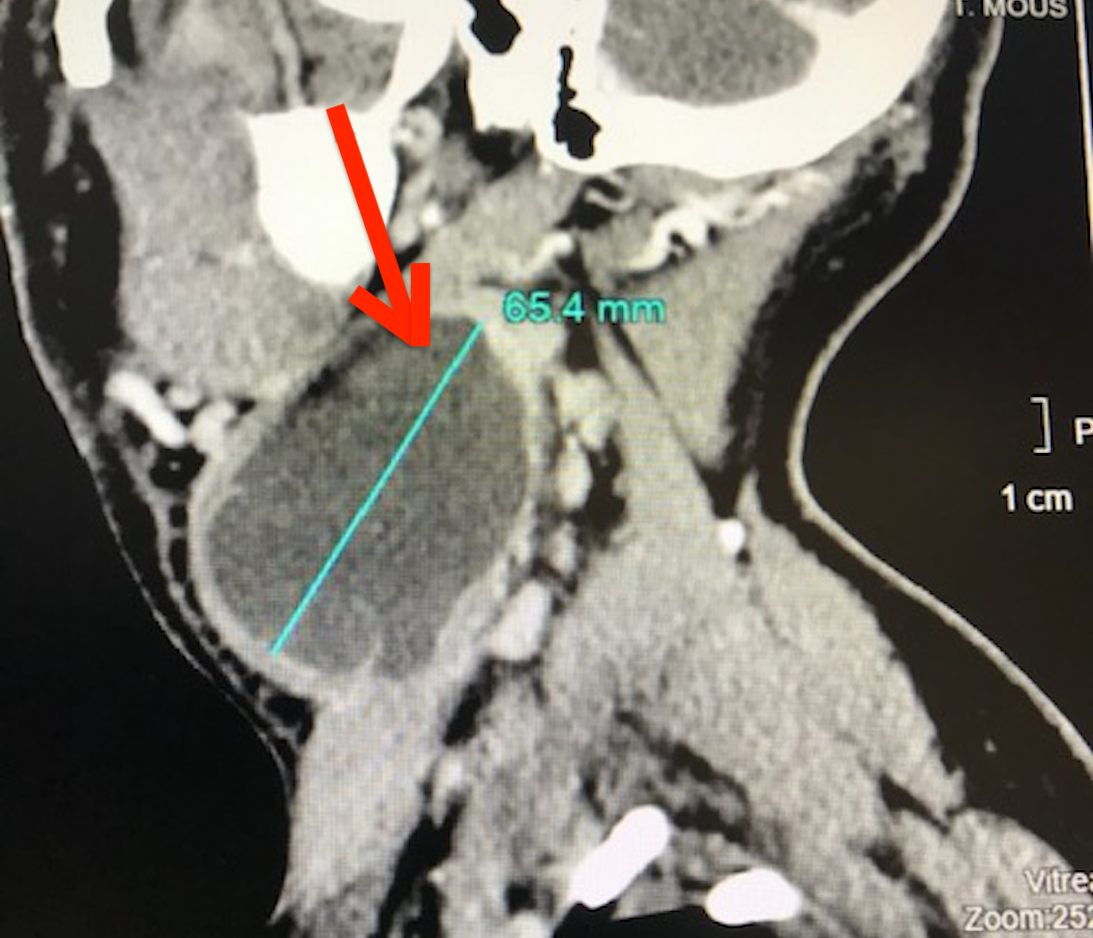
-Figure 1 :cervico-facial CT scan injected in sagittal section showing a voluminous pseudo-cystic formation of 65/50mm right isolated heterogeneous extending from the mandibular angle to the supraclavicular region responsible for extrinsic compression of the anterior surface of the internal jugular vein without satellite lymphadenopathy.
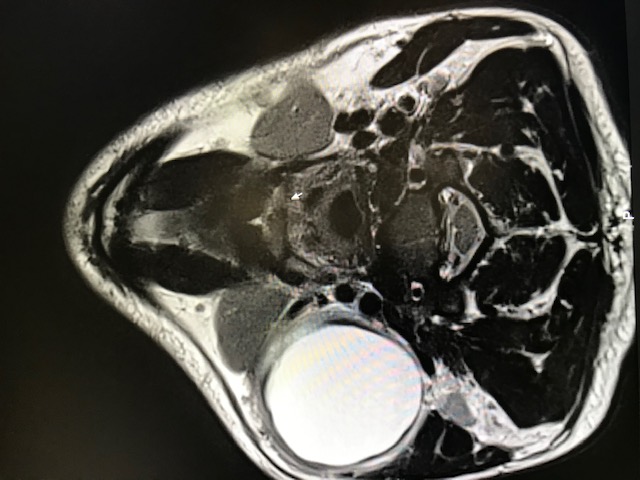
- Figure 2: T2 cervico-facial MRI in axial section found a cystic mass under the right angulomandibular with a thick wall in its upper part of the same dimensions associated with gonglions in the territories of IIa and IIb suggesting a cyst of the 2nd branchial cleft.

-Figure 3: PET scanner in axial sectionshowing a relatively intense hypermetabolic area with a necrotic center under the right angulomandibular measuring (49mm*54mm*69mm).
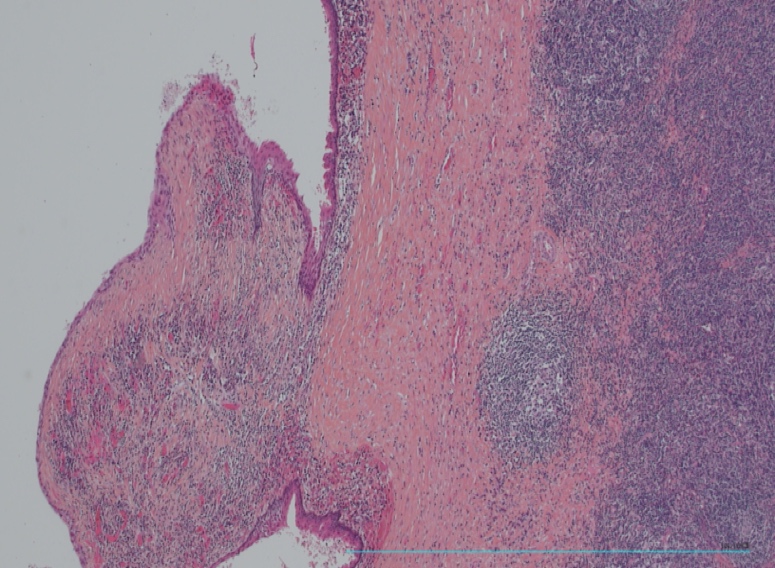
-Figure 4:The tonsilloid cyst: lined by a squamous-type epithelium with the presence of keratin and lymphoid tissue.
DISCUSSION :
Congenital cysts and fistulas of the face and neck are infrequent and poorly understood malformations of embryological origin. The ENT must recognize these lesions early to allow appropriate management [1.3]. Amygdaloid or lymphoepithelial cysts or cysts of the cervical sinus are rare benign cystic dysembryological tumors that correspond to defects in resorption of the second branchial arch [2.4] and which develop at the level of the antero-lateral part of the neck. The frequency of tonsilloid cysts versus second cleft abnormalities ranges from 6.1 to 85.2% [1.2]. The age of discovery is later than for the other congenital anomalies, with two frequency peaks, children under 5 years old and between the 2nd and 3rd decades, without any gender predominance.
Clinically, a cervical sinus cyst appears as an oval, renitent, mobile swelling under the superficial planes, most often located near the carotid bifurcation in the subhyoid position [4.5]. Although these lesions are congenital, they are usually only identified between the second and fourth decades of life, when they increase in size or become symptomatic; it sometimes communicates with the skin or the pharynx [2] spontaneously or following superinfection. Communication with the outside takes place through a narrow channel called the external cervical fistula, the external orifice of which is often located at the junction of the middle third and lower third of the anterior border of the sterno-cleido-mastoid muscle.
CT or MRI are particularly indicated to differentiate the lesion from other parapharyngeal tumours: a hemangioma, lymphangioma or dermoid cyst, metastatic adenopathy whose distinction with a degenerated amygdaloid cyst or an intracystic metastasis is very difficult and confirmation remains histological after surgical excision [1.2]. Current imaging and particularly magnetic resonance (MRI) confirms the cystic nature and the proximity of the great vessels of the neck, without prejudging the primary or secondary nature of the malignant tonsilloid cyst. The observation of a fistula of the second cleft, especially if it is bilateral, should lead to the search for a branchiootorenal syndrome by renal ultrasound. These cysts have been classified into four stages by Bailey [4]. Type I: superficial cyst, under the superficial cervical fascia, Type II: cyst under the middle cervical fascia, in the pre-vascular region (most common), Type III: inter-vascular cyst, in the fork between ACI and ACE , Type IV: intravascular cyst, between the pharyngeal wall and the carotid axis.
Histologically, the tonsilloid cyst is lined by an epithelium of different types, most often squamous cell [2], it may also be a ciliated columnar epithelium of ectodermal origin. Some authors believe that the presence of keratin, the presence of lymphoid tissue are mandatory criteria for the diagnosis of tonsilloid cyst [2]. The differential diagnosis arises especially when there is an isolated laterocervical mass without a fistula which should suggest in the child a unilocular cystic lymphangioma, a lipoma or an adenopathy [5]. Infection is the complication most often revealing this malformation complicating its surgical excision of the cyst. The tonsilloid cyst, sometimes rapidly evolving and compressive, can cause feelings of discomfort and bradycardia by rapid and significant compression of the carotid bulb, in this case the cyst must be punctured to relieve the patient. Malignant transformation within the branchial cyst is described in the literature but it remains exceptional, only 15 cases have been published in the world literature, including 4 in situ carcinomas and 11 infiltrating squamous cell carcinomas [3]. The diagnosis of malignant branchial cyst must be the subject of greater reservations and should only be retained after having ruled out a metastasis within the branchial cyst of a distant primary carcinoma as well as a simple cystic evolution of a lymph node. metastatic
Conclusion :
Therapeutic management is always surgical, it must be carried out as soon as possible to limit the risk of inflammatory changes related to infectious episodes, it will then be advisable to operate only after complete cooling of the infections by an appropriate antibiotic therapy. The fistulous path can be identified by catheterizing it with injection of methylene blue. The dissection continues in contact with the fistulous path, it stops quickly in the event of an external blind fistula. If the fistula continues upward, a second incision is needed to follow its course. The rupture of the fistula at its upper part is usually without consequence, the residual fistula draining into the oropharynx. Finally, it is not useful to perform a routine tonsillectomy.
STATEMENTS
Bid guarantor:
The corresponding author is the guarantor of the submission.
Thanks :
Nothing.
Funding :
There are no funding sources to declare.
Availability of data and materials:
Supporting documents are available should further analysis be required.
Competing interests:
The authors declare that they have no competing interests.
Consent to publication:
Written informed consent was obtained from the patient for the publication of this case report and all accompanying images. A copy of the written consent is available for review by the editor of this journal.
Ethical approval and consent to participate:
Ethical approval was obtained to proceed with the present study. Written informed consent was obtained from the patient for participation in this publication.